Introduction
Food is a minor source of vitamin D, which can be obtained in the form of cholecalciferol (vitamin D3) or ergocalciferol (vitamin D2). On the other hand, the cutaneous production of vitamin D is very efficient, being responsible for about 85-90% of the total vitamin D.1,2) 7-Dehydrocholesterol (7-DHC) is converted to pre-vitamin D3 and later to vitamin D3 by the action of ultraviolet radiation in the epidermal cells. Vitamin D3 is metabolized in the liver to calcifediol (25-hydroxyvitamin D), and finally calcitriol (1,25-dihydroxyvitamin D), the active form of vitamin D, is synthesized in the proximal tubular cells of the kidney.1-4
The primary function of calcitriol is to control the homeostasis of calcium-phosphorus metabolism. Calcitriol is responsible for increasing intestinal absorption of calcium and phosphorus, increasing resorption of calcium from the bone matrix into the bloodstream, and decreasing renal excretion of calcium and phosphorus. Parathyroid hormone (PTH) and calcitriol form a tightly controlled feedback cycle in which PTH is a major stimulator of calcitriol synthesis in the kidney, while calcitriol exerts negative feedback on PTH secretion.1,2,5) Thus, vitamin D deficiency can result in severe hypocalcemia and secondary hyperparathyroidism, which causes bone demineralization and can lead to rickets in children, with a peak incidence between the ages of 3 and 18 months.5,6 In addition to the classically described skeletal changes, hypovitaminosis D and resultant hypocalcemia can lead to other clinical complications such as laryngospasm and bronchospasm, seizures, tetany, myopathy, arrhythmias, and dilated cardiomyopathy.2,7
According to the American Academy of Pediatrics, in the pediatric population, vitamin D insufficiency is defined by systemic 25-hydroxyvitamin D levels below 20 ng/mL, and deficiency is defined by levels below 15 ng/mL.2,8 Current recommendations indicate that all infants, children, and adolescents should receive at least 400 IU of vitamin D daily from diet or supplementation. It is acknowledged that breast milk is not sufficient to provide adequate levels of this vitamin, so all infants should be supplemented with vitamin D (400 IU/day) during the first year of life.2,3,8-10 Breast milk is estimated to contain between 5 and 136 IU/L of vitamin D, depending on the season.11 Although infant formulas have some vitamin D in their composition, supplementation is also recommended for infants consuming these formulas.
There are several risk factors for hypovitaminosis D, namely exclusive breastfeeding without supplementation, low maternal vitamin D levels, darker skin, insufficient sun exposure, chronic diseases associated with intestinal malabsorption, and some medications (anticonvulsants and antiretrovirals).3,4,8,9,11
Herein is described a case of hypovitaminosis D and severe hypocalcemia with serious consequences that proved fatal, with the aim of raising awareness of the importance of universal vitamin D supplementation in the first year of life.
Case report
A six-month-old melanodermic female infant was admitted to the Emergency Department (ED) with worsening cough and respiratory distress. She was apparently well until three days before admission.
The girl had been born at 37 weeks’ gestation without complications, with a birth weight of 2845 g (P15-50) and adequate postnatal growth and psychomotor development. She had been exclusively breastfed until 5 months of age, without cholecalciferol supplementation because the family did not understand this indication. Family history was unremarkable.
On admission to the ED of a secondary hospital, she was poorly reactive, with an immeasurable peripheral oxygen saturation (SpO2) and poor peripheral perfusion. Physical examination revealed scattered crackles on lung auscultation, palpable hepatomegaly four centimeters below the right costal margin, and peripheral edema. Chest radiograph showed bilateral diffuse hypotransparency and exuberant cardiomegaly. Capillary blood gas analysis revealed severe acidosis with pH 6.94, partial pressure of carbon dioxide (pCO2) 56 mmHg, bicarbonate (HCO3) 12.2 mmol/L, calcium (Ca2+) 0.72 mmol/L, and lactate 10.6 mmol/L. Analytical evaluation of cardiac function revealed elevated cardiac enzymes, with cardiac troponin I (cTnI) 1627.6 pg/mL, creatine kinase-myocardial band (CK-MB) 223.9 U/L, and N-terminal pro-B-type natriuretic peptide (NT-proBNP) 102570 pg/mL. The remainder of the laboratory study revealed hemoglobin (Hb) 9.9 g/dL, leukocytes 9,600/µL with 10.4% neutrophils and 83.0% lymphocytes, platelets 399,000/µL, and C-reactive protein (CRP) <3 mg/L.
While in the ED, the girl had multiple episodes of extreme bradycardia requiring resuscitation and ventilatory and inotropic support, and was admitted to the Pediatric Intensive Care Unit (PICU). Cardiac evaluation with transthoracic echocardiogram showed severe cardiomegaly with dilated left ventricular cavity and global dysfunction. Cardiogenic shock was suspected and the patient was transferred to a tertiary PICU with more specialized medical care. She also had multiple brief generalized seizures after starting anticonvulsant therapy.
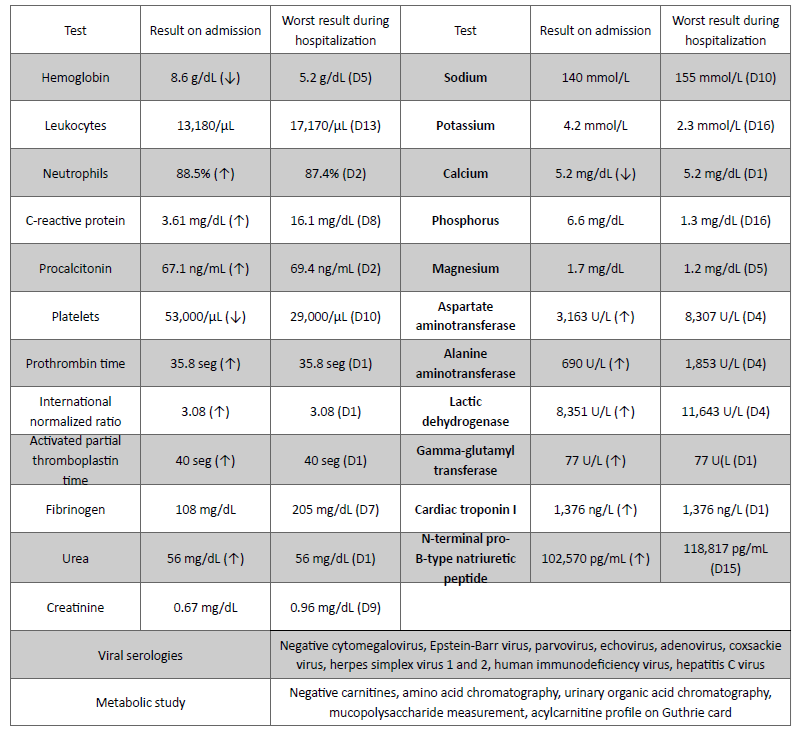
On admission to the tertiary PICU, laboratory tests were performed (Table 1). Platelets and fresh frozen plasma were administered for thrombocytopenia and prolonged prothrombin time. The patient was initially treated empirically with ceftriaxone and later with piperacillin-tazobactam and linezolid due to fever and elevated analytical inflammatory parameters. During hospitalization, she was systematically evaluated by Pediatric Cardiology. Serial echocardiograms were performed and showed no structural abnormalities despite reduced left ventricular ejection fraction (LVEF = 22%) and enlarged ventricles with a maximum left ventricular diameter of 41 mm (Figure 1). The patient presented with refractory hypotension despite optimization of inotropic support (dopamine 14 mcg/kg/min, adrenaline 0.4 mcg/kg/min, and milrinone 0.5 mcg/kg/min).
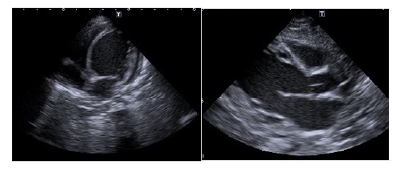
Figure 1 Transthoracic echocardiogram (apical and parasternal long-axis views) showing cardiomegaly and left ventricle dilation.
Etiologic study was performed. Viral serologies (cytomegalovirus, Epstein-Barr virus, parvovirus, echovirus, adenovirus, coxsackievirus, herpes simplex virus 1 and 2, human immunodeficiency virus, and hepatitis C virus) and metabolic study (carnitines, amino acid chromatography, urinary organic acid chromatography, mucopolysaccharide measurement, and acylcarnitine profile on a Guthrie card) were performed, showing no abnormal results (Table 1). Severe persistent hypocalcemia (5.2 mg/dL; reference values 8.5-11 mg/dL), hyperparathyroidism (PTH 220 pg/mL, reference values 14-72 pg/mL), and severe vitamin D deficiency (3.6 ng/mL; reference values >15-20 ng/mL) led to the hypothesis of dilated cardiomyopathy secondary to hypocalcemia due to hypovitaminosis D. The mother also had vitamin D deficiency (12.8 ng/mL - moderate deficiency). Human metapneumovirus was identified in bronchial secretions (PCR test). Blood and urine cultures were negative. No signs of bone disease were observed in the radiologic studies performed.
The patient was started on replacement therapy with calcitriol and calcium gluconate, which resulted in a slight improvement in cardiac function. Inotropic support was stopped and the girl was extubated without complications. Antibiotic therapy was also suspended due to the absence of bacterial infection.
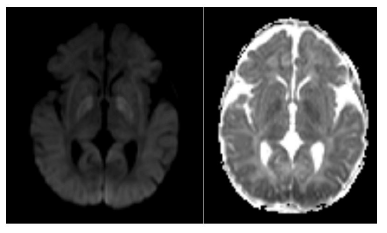
After weaning from sedation and analgesia, she maintained an altered mental status with spontaneous eye opening but no fixation or gaze following, poorly reactive isochoric pupils, and symmetrical but small amplitude mobilization of the four limbs. Transfontanellar ultrasound showed diffuse cerebral edema, and brain magnetic resonance imaging revealed severe hypoxic-ischemic encephalopathy consistent with the clinical findings (Figure 2). The electroencephalogram showed diffuse slowing of brain activity without epileptic activity.
Considering the severe hypoxic-ischemic encephalopathy with a very poor prognosis, the multidisciplinary team decided to initiate comfort measures and palliative care. The patient was transferred to the ward and died 19 days later.
Discussion
This clinical case documents a series of serious complications of hypocalcemia due to hypovitaminosis D, namely dilated cardiomyopathy with severe heart failure and cardiogenic shock requiring resuscitation and inotropic and ventilatory support.
The patient presented with values compatible with severe vitamin D deficiency and hypocalcemia with secondary elevation of PTH requiring multiple corrections. Radiologic evidence of rickets usually appears later in the course of the disease, but was not observed in this case.7
As previously mentioned, there are many risk factors for hypovitaminosis D, namely exclusive breastfeeding without supplementation, low maternal vitamin D levels, dark skin, and insufficient sunlight exposure.3,4,8,9,11 This patient was at a critical age for the development of the above complications, was melanodermic, had been exclusively breastfed until five months of age, had never received vitamin D supplementation, and her mother also had levels compatible with vitamin D deficiency.
The cutaneous synthesis of vitamin D depends on several factors, such as geographic region, season, time of day, area of body surface exposed to the sun and duration of exposure, use of sunscreen, skin pigmentation, obesity, and age.5 The lower cutaneous synthesis of vitamin D in darker skin has been classically accepted, considering the role of melanin in blocking ultraviolet radiation. As a result, darker-skinned people need more sun exposure (about five to ten times more than lighter-skinned people).1,3,12 This is not recommended due to the risks of excessive sun exposure in young children.3
Breast milk is the most nutritious food for infants, but does not contain enough vitamin D. On the other hand, the mother of the patient in this case also had reduced vitamin D levels, and this deficiency is vertically transmitted from mother to child.3,4,11 Dawodu et al. demonstrated a significant association between low levels of vitamin D in breastfeeding mothers and their children.13 All these factors contribute to the need for vitamin D supplementation in the first year of life (400 IU/day).2,3,8-10
Seizures associated with severe hypocalcemia are a known complication of hypovitaminosis D.6,7 However, in this case, the seizures appear to have resulted from cerebral hypoperfusion due to the multiple episodes of extreme bradycardia requiring resuscitation.
Dilated cardiomyopathy is the most common form of cardiomyopathy in children (1.13 cases in 100,000 children).11 Most dilated cardiomyopathies have an idiopathic etiology (50-70%).14 Other known causes of dilated cardiomyopathy include genetic and metabolic disorders, viral infections, and ionic disturbances. Calcium ions play an essential role in the regulation of myocardial contractile function, and although hypocalcemia is a rare cause of dilated cardiomyopathy, some cases have been described in the literature.8,11,12,15
Uday et al. described three clinical cases of infants diagnosed with dilated cardiomyopathy with low serum calcium and vitamin D levels and elevated PTH levels.7 In Portugal, Moniz et al. and Laranjo et al. also described cases of infants with a clinical condition compatible with dilated cardiomyopathy due to hypocalcemia secondary to hypovitaminosis D.8,11 In the present case, the authors believe that there was a previous dilated cardiomyopathy secondary to hypocalcemia and hypovitaminosis D decompensated by metapneumovirus respiratory infection.
As described in the literature, early detected cases may be reversible with supplementation.8,11,15 However, this patient presented a very severe clinical picture, with prolonged cardiogenic shock leading to cerebral anoxia and ultimately death, despite a slight improvement in cardiac contractility after initiation of supplementation therapy.
Conclusion
This case highlights the importance of vitamin D supplementation in infants during the first year of life, not only to ensure proper bone development, but also to prevent cases of cardiomyopathy that can lead to heart failure, cardiogenic shock, and even death. Dilated cardiomyopathy secondary to hypocalcemia due to hypovitaminosis D is potentially reversible with targeted therapy. In this particular case, the progression to peri-arrest and subsequent hypoxic-ischemic encephalopathy contributed to the outcome.
Authorship
Clara Picão de Carvalho - Conceptualization; Data curation; Investigation; Project Administration; Resources; Visualization; Writing - original draft; Writing - review & editing
Filipa Carmo - Conceptualization; Data curation; Investigation; Resources; Visualization; Writing - original draft; Writing - review & editing
Rosa Martins - Writing - review & editing
Eugénia Matos - Data curation; Writing - review & editing
Erica Torres - Conceptualization; Data curation; Supervision; Writing - review & editing
Mónica Rebelo - Data curation; Writing - review & editing