Introduction
Hyperkalemia (HK) is a medical condition characterized by abnormally high levels of serum potassium (K+).1HK is most commonly caused by reduced urinary excretion of potassium, which is often observed in patients with kidney diseases such as chronic kidney disease (CKD). Other risk factors for HK include male gender, non-black race, lower body mass index, advanced age, smoking, a history of diabetes mellitus, coronary artery disease, or heart failure, and the use of angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and potassium-sparing diuretics.2-5The most commonly used definition for the severity of HK can be classified as mild (>5.0 to <5.9 mEq/L), moderate (6.0 to 6.4 mEq/L), and severe at thresholds (>6.5 mEq/L).6
HK can lead to serious electrophysiological disturbances, such as cardiac arrhythmias. Specifically, severe HK is an independent predictor of hospitalizations, in-hospital mortality, and all-cause mortality.4-7It is also important to note that chronic HK can be asymptomatic, so it is important to frequently monitor these patients to detect any changes and prevent potential complications.1-7An increase in K+ has several consequences for myocardial action potential, so HK can manifest with different types of electrocardiogram (ECG) abnormalities.1,5,7-9
The treatment of acute HK requires various procedures aiming at preventing or minimizing electrophysiological effects on the heart to reduce the immediate risk of arrhythmias.9 This requires intravenous access, continuous cardiac monitoring through ECG, quantifying the absolute concentration of potassium in the blood, as well as the rate of increase in its concentration. However, neither serum potassium levels nor ECG alone are sufficient to determine the need for treatment, and the physician must consider the clinical context. To minimize the damage caused by HK, it is necessary to stabilize cardiac cell membranes, shift extracellular K+ into cells (or redistribution), and eliminate K+ from the body.10 One way to do this is through the administration of certain potassium-binding medications.
This part of HK treatment is particularly subject to a lack of consensus among healthcare professionals.7,8This is particularly evident when considering the introduction of new potassium-binding drugs and their application in patients suffering from HK due to CKD or adverse effects of prevalent medications, notably the renin-angiotensin-aldosterone system inhibitors (RAASis).2,3Real-world studies show additional evidence in this regard. The observational REVEAL-ED study found that treatment decisions by healthcare professionals were often influenced by initial potassium levels in patients and confirmed the lack of a standardized treatment protocol for HK in emergency settings, echoing findings from previous studies.11
Defining how to optimally manage HK is crucial. In August 2021, experts from Europe and North America formed a steering group, both cardiologists and nephrologists, aiming to address HK management in cardiorenal disease.12 Current clinical guidelines recommend different procedures to protect the heart and to eliminate K+ and protect the heart allowing for the reversion of the proarrhythmogenic effects.13,14In an emergency situation, it is essential to begin dialysis treatment, but there are logistical challenges that need to be addressed before starting this treatment.12 Despite the existence of some statements regarding the treatment of HK, there is still no unanimous agreement on ideal practices among the Portuguese medical community.11,13
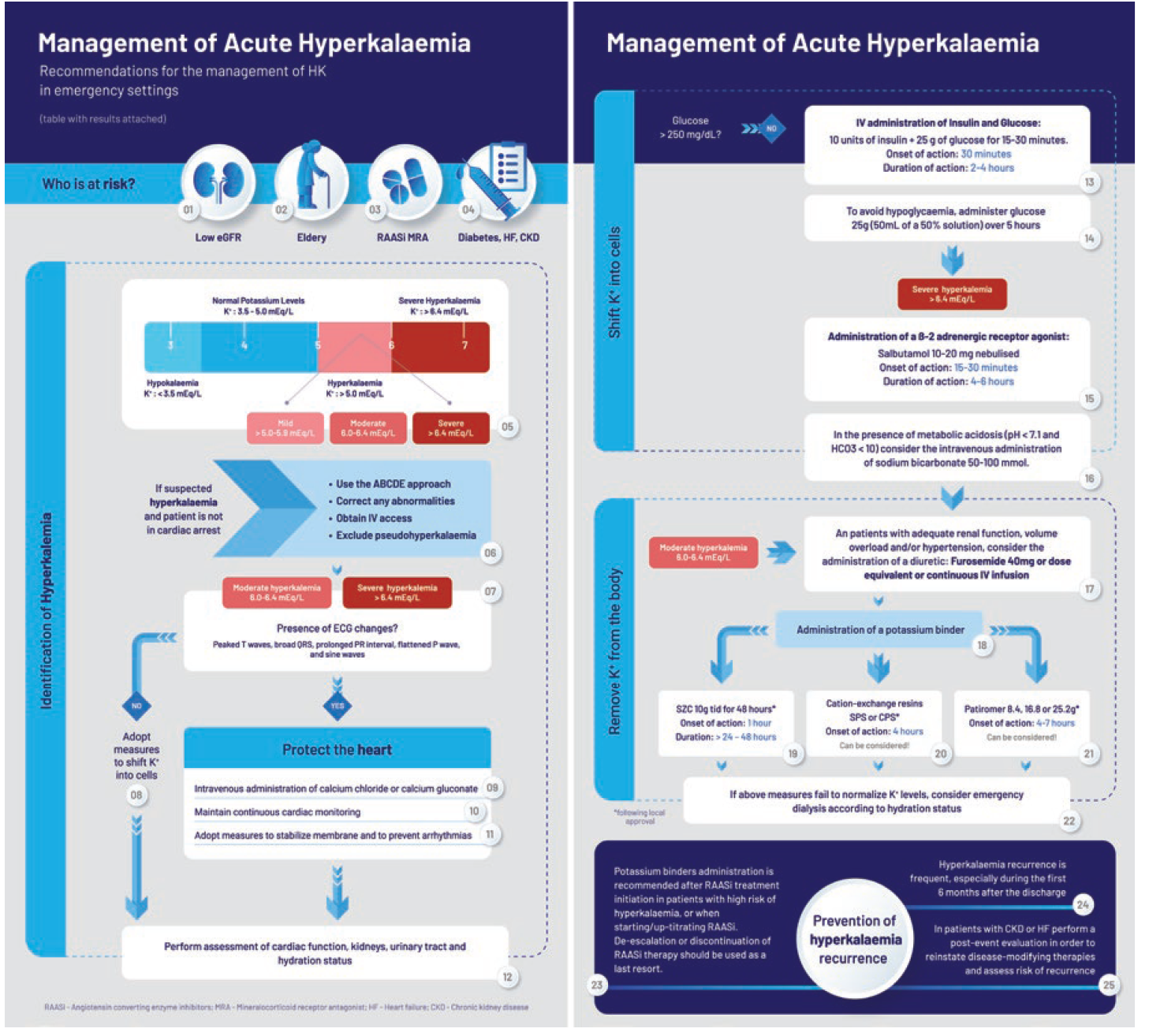
This study aims to define a consensus on the effective management of HK in Portuguese emergency settings among healthcare professionals. Secondarily, we aim to develop a comprehensive visual tool with recommendations to facilitate the understanding and implementation of good practices in emergency setting, with the ultimate goal of improving patient outcomes and optimizing the management of HK-related emergencies.
to facilitate the understanding and implementation of good practices in emergency setting, with the ultimate goal of improving patient outcomes and optimizing the management of HK-related emergencies.
Methods
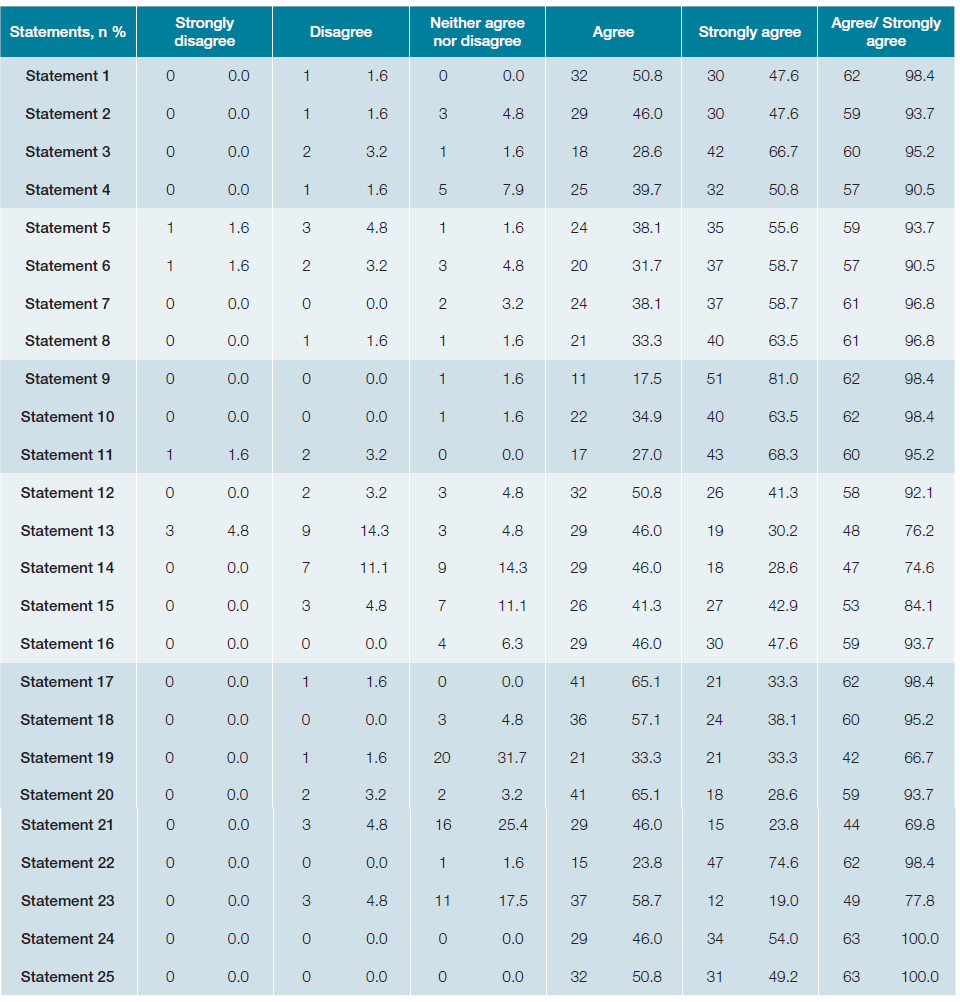
This is an observational, cross-sectional qualitative study, based on the Delphi consensus methodology.15,16Specifically, we assembled a panel of six Portuguese experts on HK management in emergency situations within the national context, including members of the “Núcleo de Estudos de Urgência e do Doente Agudo” and Directors of emergency care from different hospitals of the country. Based on the European Resuscitation Council Guidelines 2021,17 the experts identified five main topics: “Who is at risk?”, “Identification of hyperkalemia”, “Protect the heart”, “Remove K+ from the body” and “Prevention of hyperkalemia recurrence”. These topics were further discussed by the group and 25 statements to represent crucial applicable steps in the treatment of this clinical condition were defined (Table 1). These informed an anonymous online questionnaire developed using Google Forms.
The questionnaire was distributed through email, among doctors selected based on their expertise on attending HK-related emergencies. Participants were asked to indicate the level of agreement with each statement using a 5-point Likert scale (‘strongly disagree’, ‘disagree’, ‘neither agree or disagree’, ‘agree’, and ‘strongly agree’). The initial round lasted between July and August 2023. The consensus was defined by a concordance of at least 65% for those classified as “agree”/ “strongly agree”. The questionnaire results were analyzed by the independent investigator to produce an agreement score for each statement. After this round, the results were reviewed by the expert panel. Survey iterations would be performed until the consensus threshold was achieved; however, due to the levels of agreement received after the first round, the expert panel agreed that further rounds were unnecessary.
Results
A total of 63 specialist doctors participated in the online questionnaire. All participants completed the entire questionnaire, with no missing values.
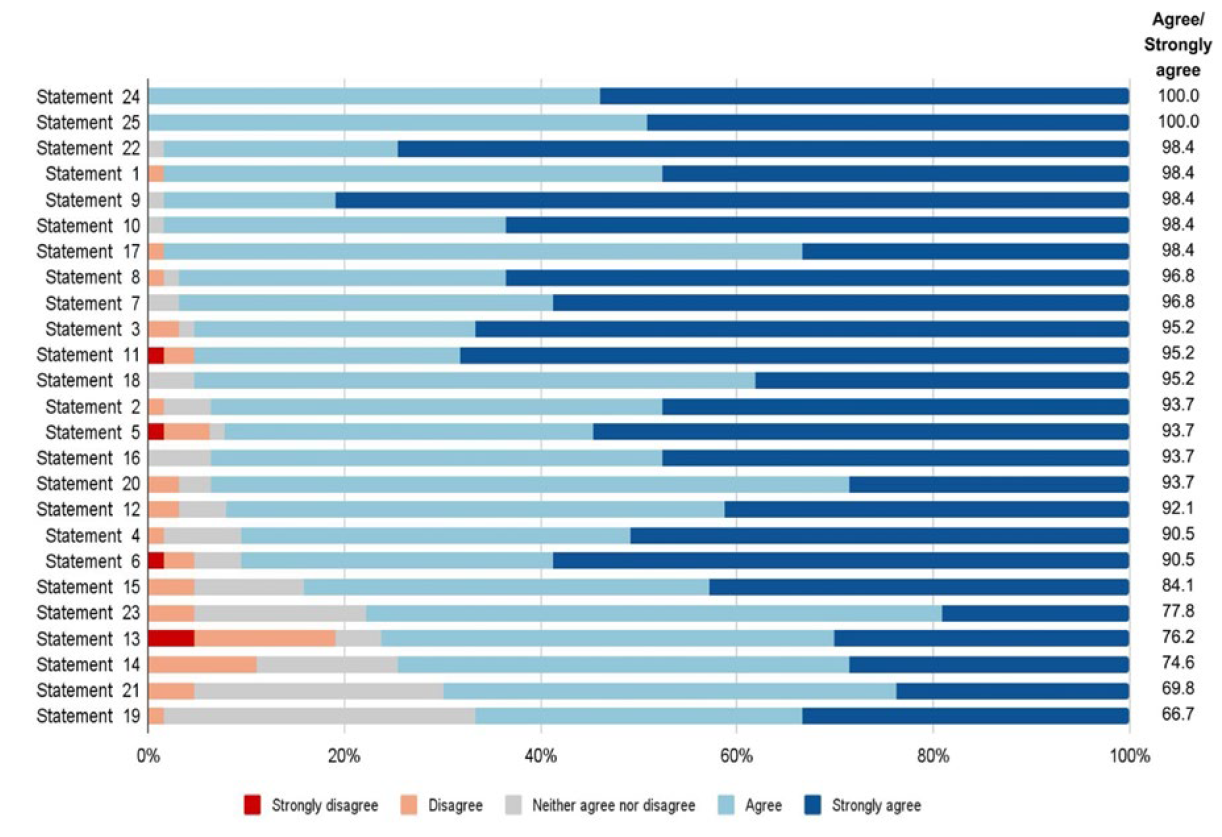
The 25 predefined statements reached a very high consensus (Fig. 1, Appendix). More than 90% participants agreed/strongly agreed with 19 statements and at least 66% agreed/strongly agreed with the remaining 6 statements. Statements 19, 21 and 23, related to the potassium management by the administration of SZC, patiromer and scavengers in patients on iRAAS, had the lowest consensus with 32%, 21% and 11% of “neither agree or disagree” answers, respectively. The highest rate of disagreement (disagree/strongly disagree) was 19% for statement 13, on insulin treatment. The remaining statements always had a low percentage of disagreement, with 56% of the statements having disagreement rates below 2%. Based on these highly consensual 25 statements, the involved experts developed a visual tool with the recommendations for the management of HK in an emergency context (Fig. 2). Consensus was defined as at least 65% of agree/strongly agree.
Discussion
The results show strong recognition that HK is predictable, treatable and manageable through treatment optimization. This study yielded consistent results on the 25 predefined statements related to HK management in Portuguese emergency settings. Notably, statements regarding the administration of SZC, patiromer and potassium scavengers in patients on iRAAS treatment had the lowest consensus levels and the statement with the highest rate of disagreement was about insulin treatment. The results obtained informed the recommendations presented in Fig. 2.
There is overall consensus on the populations in higher risk of HK and poor clinical outcomes. HK is a critical concern for patients with chronic kidney disease, particularly those with a lower eGFR.
Also, that the elderly population faces an elevated risk due to factors like reduced renin activity, decreased plasma aldosterone levels, and the frequent use of non-steroidal anti-inflammatory drugs (NSAIDs). Moreover, patients on medications such as iRAAS, ARBs, MRAs, or potassium-sparing diuretics are also susceptible to hyperkalemia. Importantly, hyperkalemia is associated with higher mortality risk, and individuals with both hyperkalemia and underlying conditions like heart failure, type 2 diabetes, or chronic kidney disease face even greater mortality risks. Additionally, prolonged exposure to hyperkalemia further escalates mortality risk, underscoring the importance of prompt management and monitoring. These results are in line with literature. The risk factors associated with hyperkalemia, including reduced eGFR, advanced age, medication use, and underlying medical conditions like heart failure, diabetes, and chronic kidney disease, are widely recognized in medical literature.8 The increased mortality risk associated with hyperkalemia, especially in patients with comorbidities, is also well-documented.
Regarding lower agreement on the management of potassium elevation in patients with CKD on iRAAS treatment is in line with the general uncertainty on this subject. This is particularly evident when considering the introduction of new potassium binding drugs (such as SZC and patiromer) or adverse effects of prevalent medications such as iRAAS.7,8The medical community lacks consistent guidelines on managing HK in cardio-renal patients, leading to varied practices among cardiologists and nephrologists.18 The use of iRAAS is critical for the kidney and cardiovascular protection in patients with chronic kidney disease.14 However, these agents can lead to hyperkalemia, and the risk may be potentially enhanced in patients with high potassium levels such as patients receiving potassium-sparing diuretics and potassium supplements, concomitantly with iRAAS.12 Clear strategies to minimize hyperkalemia risk that do not interfere with optimal iRAAS therapy should be prioritized in patients with CKD. These strategies may include the use of potassium-binders, based on evidence of these agents to effectively achieve normokalemia while optimizing RAASi treatment18 however their adoption is not yet widely applied, possibly due to limited access to these potassium binders.19 Interestingly, in individuals with CKD, there is a lower risk of death related to high potassium levels when compared to those with normal kidney function. However, it is important to note that in CKD situations, high potassium still significantly increases the risk of both short-term and long-term mortality.5
The insulin-glucose treatment to manage HK is less consensual than other statements which may be related to the risk of hypoglycemia after treatment.15 Patients in higher risk of post treatment hypoglycemia include age (> 60 years old), pretreatment blood glucose ≤ 100 mg/dL (≤ 5.6 mmol/L), and pretreatment potassium > 6 mmol/L.16 In high-risk groups glucose must be monitored for at least 4-6 hours after administration.
This study illustrates a high degree of alignment among experts, emphasizing the potential for improving HK management in emergency contexts. However, it has some limitations, namely a potential selection bias as the participants in the consensus process are all internal medicine specialists. It would be valuable to explore the perspectives of cardiologists and nephrologists despite their attendance in general emergency rooms being less common in the Portuguese context. One might suggest that setting a more stringent consensus criteria would necessitate an additional round for achieving more robust results. The decision to conduct only one round was based on the observation that the results obtained already reflected significant consensus among the experts, surpassing the 65% cut-off point for consensus. Nonetheless, we acknowledge that additional rounds could potentially enrich the dialogue among experts and further strengthen the study's findings. However, it's important to note that the Delphi consensus method commonly encompasses a range of 55% to 100%, with the standard threshold typically considered at 70%.15,16
Conclusion
This study established a consensus on the effective management of HK in Portuguese emergency settings among 63 healthcare professionals. Our panel of distinguished Portuguese experts has worked collaboratively to formulate and endorse recommendations, covering critical aspects including the epidemiology, underlying mechanisms, optimal management, and treatment strategies for acute HK. Remarkably, most of the statements reached consensus levels of at least 90% agreement, which reinforces the credibility and reliability of our re-commendations. We have also developed a visually informative tool, designed to foster a more unified clinical approach among Portuguese health professionals. We believe the implementation of these recommendations will contribute for optimization of the management of HK-related emergencies, improving patient clinical outcomes.