Introduction
The population is aging, leading to an increase in the number of chronic diseases and average life expectancy (INE,2023). In Europe, 85% of the population currently dies from chronic diseases such as cancer, cardiovascular disease, or dementia. Chronic diseases are characterized by their slow progression, fluctuations in disease trajectory, long duration, and uncertain prognosis. Therefore, it is a great challenge to treat chronic diseases for an increasingly longer period, until very advanced stages of their progression (Divo et al, 2014). In the advanced stages of chronic disease, patients normally suffer from pain and other physical and psychological symptoms, so they could benefit from a palliative care approach (Moens et al, 2014; Barbosa A, 2006). It is therefore essential to identify patients who could need this approach, which englobes physical, psychological, social, and spiritual care, to promote quality of life in all its aspects (SPICT-PTTM, 2019).
There is evidence from randomized controlled trials that early access to specialized palliative care can promote quality of life, reduce time of hospital admission and hospitalizations, and even prolong survival (Vanbutsele et al, 2018; Kavalieratos et al, 2016). However, recent evidence shows that palliative care typically arrives late in the disease trajectory and access to palliative care is unequal (Allsop et al, 2018; Mason et al, 2018).
The patients with palliative needs are in hospitals and long-term care units, but especially in the community, so Primary Health Care teams are in the best position to identify these patients. Indeed, the needs of approximately 85-90% of people at the end of life can be met with primary palliative care provided by family doctors (Afshar et al, 2020).
One of the barriers to timely access to palliative care is the difficulty in the identification of patients who could benefit from them and defining the right time to do so (Hawley, 2018). The identification process should not be based solely on predicting mortality or survival but must also focus on anticipating needs whenever they occur and predicting the course of functional decline to trigger a holistic assessment and develop a proactive palliative care plan (ElMokhallalati et al, 2020). The SPICT™-PT is a clinical tool that supports the identification of patients who might benefit from a palliative care approach, the planning of future care and can be used in different settings (SPICT-PTTM, 2019)
National and international studies have evaluated palliative needs in a hospital context (Bourmorck et al, 2023; De-Bock et al, 2018; Gómez-Batiste et al, 2014; Hamano et al, 2018; Hamano et al, 2019; Highet et al 2013; Martins, 2020; Piers et al, 2021; Wijmen et al, 2020), and to date, it has not been possible to identify national studies within the scope of Primary Care, which makes it extremely important to carry out a study in this area.
This study aims to evaluate palliative needs in a list of patients of a Portuguese Family Health Unit.
1. Methods
A single-center observational, cross-sectional study was conducted in a Portuguese Family Health Unit. The protocol was submitted for consideration of the Health Ethics Committee (reference nr. 112/CES/JAS) and the Local Information Protection and Security Committee, by which it was approved. Informed consent was dispensed by the Local Information Protection and Security Committee.
Sample
We included patients aged 65 years or older from a family physician’s list. Patients who had face-to-face or non-face-to-face contact with the family health team during the study period were included, up to the representative sample size, which was determined considering a confidence interval of 95% and a precision level of 5%, from the total number of patients on the aforementioned list, at the date of data collection.
Patients with a record of last contact with the family health team exceeding 2 years ago were excluded.
Data collection instruments
A convenience sample of patients that contacted the family physician during the study period was asked to participate in this study. The SPICT-PTTM tool, 1st and 2nd part, was applied, as well as a collection of sociodemographic data (age, gender, institutionalization or not, level of independence through the Barthel index and main underlying disease).
The SPICT™ tool helps identify patients with deteriorating health due to serious illness or advanced conditions, prompting holistic assessment and future care planning. SPICT™ is available in multiple translations including Portuguese (SPICT-PTTM), by the authors Mariana Mira e Paulo Reis-Pina (https://www.spict.org.uk/the-spict/spict-pt/), its use having been authorized by both authors. Palliative care needs are considered whenever we have at least two general indicators (1st part) and at least one clinical indicator (2nd part).
Statistical Analysis
A descriptive analysis was carried out to evaluate the frequencies of the variables in the sample, followed by an inferential analysis to look for significant relationships between them. Nominal variables were evaluated in terms of absolute frequencies and percentage of each category, while continuous variables were evaluated in terms of minimum and maximum values, median and interquartile range. Categoric variables were expressed as counts and percentages and were compared with Pearson’s chi-square test or Fisher exact test as appropriate. The chi-squared test was used to compare the nominal variables between groups. Binomial analysis was also performed. The analyses were completed using IBM SPSS®, version 27.0 (IBM Corporation, NY, USA). A p-value of less than 0.05 was considered statistically significant.
2. Results
2.1 Sociodemographic characterization
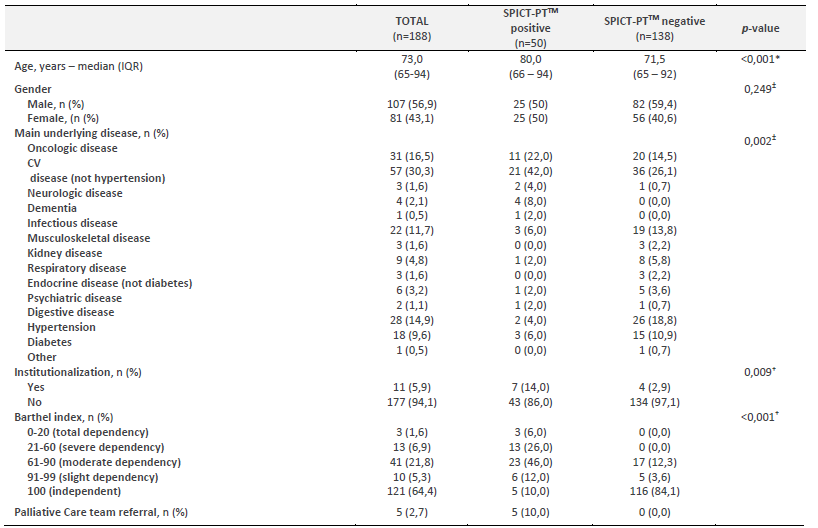
A total of 188 patients aged 65 years or older were included during the study period, of which 56,9% were male. Table 1 shows patients' characteristics. Cardiovascular disease was the most frequent main underlying disease in the total sample (n=57, 30,3%), followed by oncologic disease (n=31, 16,5%) and hypertension (n=28, 14,9%).
2.2 Characterization of the patients with palliative care needs
Of the study population, 50 patients (26,5%) were identified as having palliative care needs (SPICT-PTTM-positive) (Table 1).
The median age of the SPICT-PTTM-positive was significantly higher than that of the SPICT-PTTM-negative (80,0 vs 71,5, p<0,001). There were no statistical differences concerning gender (p=0,249). As mentioned above, cardiovascular disease was the main underlying disease in both groups. The second most frequent condition in SPICT-PTTM-positive patients was oncologic disease. We found statistically significant differences when analysing the association between the SPICT-PTTM scale and the main underlying disease (p=0,002).
We performed a simple linear regression to test if a positive score was associated with specific groups of diseases, but it was not possible to affirm that. A binomial analysis was performed to evaluate the proportion of positive scores among groups of diseases, and we found that negative scores are higher in groups of diseases like hypertension (26/2, p<0.001), diabetes (15/3, p=0.008), respiratory diseases (8/1, p=0.039) and musculoskeletal disease (19/3, p<0.001). From this study sample, 11 patients (5,9%) were institutionalized. Among institutionalized patients, 63,66% were SPICT-PTTM-positive while among non-institutionalized patients 26,3% were SPICT-PTTM-positive. Regarding the dependence level, we also found significant differences between SPICT-PTTM-positive and SPICT-PTTM-negative patients (p<0,001).
From the analysis of the SPICT-PTTM-positive patients, we observed that the most frequent general indicators were “depends on others for care due to increasing physical and/or mental health problems” (84%), followed by “persistent symptoms, despite optimized treatment for the underlying condition(s)” (68%). The lowest prevalence was the indicator concerning the request from patients or families for palliative care (10%). Regarding specific indicators, the most frequent among SPICT-PTTM-positive patients were “not able to communicate by speaking; little social interaction” (58%) followed by “urinary and faecal incontinence” (50%).
2.3 Characterization of the patients referred to the Palliative Care team
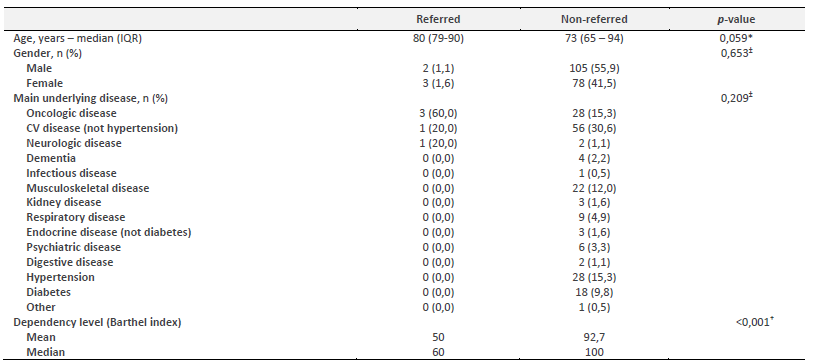
In addition to the described data, we carried out an analysis of the patients referred to the Palliative Care team. As we can see in Table 1, all the patients referred to the Palliative Care team were SPICT-PTTM-positive. Oncologic disease was the most frequent condition of the patients referred (60%). We found no statistically significant differences between referred and non-referred patients regarding age (median), gender, and main underlying disease (Table 2). However, as expected, patients referred to the Palliative Care team have a significantly higher level of dependency (p<0,001).
3. Discussion
To our knowledge, this was the first study that addressed palliative needs in Primary Health Care in Portugal using the SPICT-PTTM tool. Around a quarter of the assessed patients aged 65 or older have palliative needs. A study carried out in Primary Health Care in Japan, also using the SPICT scale, showed that 17.3% of patients had palliative needs, although they used a different cut-off point to that used in this study, meaning that a direct comparison of the results cannot be made (Hamano et al, 2019). Another study, which used the NECPAL scale associated with the Surprise Question, showed that around 8% of patients over the age of 65 presented palliative needs (Gómez-Batiste et al, 2014). Our study, which includes both face-to-face contacts and non-face-to-face contacts may explain this value, which is higher than those found in the literature.
The general practitioner's (GP) knowledge of the health status of their patients, as well as a closer monitoring of both their patients and their families, inherent to Family Medicine, allows for a more reliable assessment of the current health status, even through non-face-to-face contacts with your family healthcare team.
Non-oncological diseases represented a large proportion of patients with palliative needs, which reflects the heterogeneity of the primary care population, as seen in the literature (Gómez-Batiste et al, 2014; Hamano et al, 2018, Hamano et al, 2019).
Of the patients with palliative needs identified, 10% were referred to the Palliative Care Team. The identification of palliative needs, as we know, does not mean the need for referral to a team specialized in Palliative Care, but rather the need to initiate a process of promoting discussion with patients and their families, to plan the adequacy of future care. It also demonstrates the importance of timely identification of patients who benefit from palliative care integrated into their general care, to better adapt the care provided by family health teams, using palliative care principles in their clinical practice.
In our study, of the 11 institutionalized patients, seven (63,6%) had palliative needs and none of them were referred to a Palliative Care Team. Although it was not specifically addressed in this study, the question remains whether the GP would consider that these users will have greater monitoring and support, namely by a nursing team in the institutions, or if the palliative needs they do have, do not motivate referral to a palliative care team. As we know, the causes for institutionalization could be social issues or lack of family support, and not due to multimorbidity or chronic illnesses at the end of life. In fact, although these patients had a mean age of 82,4 years, 63,6% of them had a Barthel score of at least 75 points. Further investigation is needed to understand how and to what extent institutionalized patients access palliative care.
Of the users who were referred to a Palliative Care Team, 60% had oncological disease. However, given that the number was too small, it does not allow for the drawing of conclusions and/or generalizations.
Our results and the lack of studies in the Primary Care only allow us to speculate about the advantages of early identification of palliative needs. The authors believe that it will allow the GP to be more aware to these patients, anticipating care that will predictably be necessary, whether in clinical, family, economic or social terms. It also allows the GP to introduce primary palliative interventions as conversations about advanced care planning especially with non-oncological patients that have a more uncertain disease trajectory, involving patients and families in decision making processes.
By carrying out this study, we verified that the SPICT-PTTM tool is easy to use and quick to complete, which could represent a helpful instrument for Family Medicine in identifying patients with palliative needs and in initiating the palliative approach, offering a starting point for introducing advanced care planning.
Despite the innovative results and this being the first study to apply the SPICT-PT tool in a community setting in Portugal, some limitations must be highlighted. The most important limitation was the restriction of the population to a small sample from a list of patients of a general practice unit, a sample limited to patients who contacted their unit during the study period and not randomized, which makes it difficult to generalize the results. More studies will be needed, particularly comparing rural communities and urban areas or other geographic areas, based on different lists of patients and with randomized samples, to analyze and compare the results of this study. On the other hand, the restriction in this study to a population over 65 years of age limited the identification of palliative needs in younger patients, so further studies will also be needed to understand palliative needs in these age groups. It is also of interest to understand what kind of actions are initiated after the identification of patients with palliative needs as well as the nature and complexity of those needs.
Although primary care providers are pivotal in the generalized provision of palliative care, barriers to achieving that can be identified. Barriers reported by primary care providers include bureaucratic procedures, communication difficulties and lack of skills or confidence (Carey, 2019). Growing demands on palliative care delivery will pose a challenge in future years for health systems to adapt to changes in population needs (Etkins et al, 2017).
Conclusion
Of the study population, 50 patients (26,5%) were identified as having palliative care needs, and 10% of which were referred to palliative care. Traditionally it is easier to identify palliative needs in oncological patients since the disease’s trajectory is easier to predict. However, non-oncological diseases, especially in primary care, represent many patients with palliative needs that need to be addressed timely.
General practitioners have a privileged position to identify patients with palliative needs due to their knowledge of their health conditions and their social, emotional, and familiar circumstances. Referral to palliative care should be analysed in context, depending on the availability of Community Palliative Care Teams.
This study opens an opportunity to better evaluate the needs of patients facing life threatening conditions in the community and further investigation is needed to understand the nature of the identified needs and its complexity.
Author contributions
Conceptualization, D.P., E.F., T.C., I.G. and C.R.; data curation, D.P., E.F. and L.S..; formal analysis, E.F. and L.S.; investigation, D.P., E.F. and T.C.; methodology, D.P., E.F. and T.C.; project administration, D.P. and E.F.; resources, T.C. and C.R.; supervision, T.C., I.G. and C.R.; validation, D.P. and E.F.; visualization, D.P.; writing-original draft, D.P. and E.F.; writing-review and editing, D.P., E.F., T.C., I.G. and C.R.