Functional health literacy, defined by the term health literacy, constitutes a multidimensional concept which has evolved in recent decades. Typically construed as the application of a set of skills to access, understand and assess information and take appropriate decisions related to health for oneself, family or community, health literacy has become an important determinant of health and outcomes (Nutbeam, 2008; Poureslami et al., 2016; Rudd, 2015). Low patient literacy can negatively influence a number of health outcomes, including medication adherence (Martins et al., 2017) chronic pain management (Edward et al., 2018), knowledge on disease (Moraes et al., 2017), need for care and hospitalization in chronic disease (Taylor et al., 2017) and mortality (Wolf et al., 2010).
It is important to consider aging in the health context, particularly in relation to low levels of functional health literacy. Older adults are among the healthcare users most impacted by low functional health literacy. The effect of low literacy is also greater in situations of chronic disease, which require long-term care, as well as low income and low education settings (McCulloch, 2015; Parnell, 2015). Health literacy is negatively associated with the variables age (Chesser et al., 2016; Kobayashi et al., 2016) and with cognitive decline (Geboers et al., 2018). In older adults, low health literacy acts as a progressive barrier to the individual´s involvement in protection behaviors, health promotion, as well as control of acute or chronic conditions (Chesser et al., 2016).
However, it is important to bear in mind that functional health literacy is not a non-modifiable condition, but a health determinant which should be exploited in health practice by health professionals from the field to help enhance the self-care skills of the individual (Santos et al, 2017). In this context, Rudd (Morony et al. 2015; Rudd, 2013, 2015; Rudd & Keller, 2009) highlight the health-related materials produced to inform, guide and prepare patients for self-care, which are often written for a level exceeding the average reading skills of the lay public. This scenario can have disastrous consequences in situations of low health literacy and act as a confounder in studying the concept. Therefore, healthcare should also center on health professionals´ communication skills in facilitating understanding of information and promoting active engagement of individuals, as well as be sensitive to the settings in which health actions are implemented (Rudd, 2015).
Improving the quality of healthcare services involves implementing strategies aimed at measuring health outcomes. To achieve this goal, appropriated strategies and interventions for low functional health literacy are important and require that professionals have skills and knowledge in this area (Moraes et al., 2017). These strategies, if well planned and targeted, lead to improved health literacy skills, particularly regarding health of older adults and management of chronic diseases. These benefits can extend to include patient self-care management, positively impacting communication, treatment compliance and health status, translating to greater life satisfaction for older patients and lower cost burden for health systems (Chesser, 2016; Vargas et al., 2014).
Understanding the impact of functional health literacy on health outcomes in older adults is vital to providing effective care (Parnell, 2015). In this context, previous interventions involving health literacy have sought mainly to make health information and services more usable (Jacobs et al., 2017). To achieve this goal, health professionals should have the necessary knowledge and skills on health literacy to promote this among their patients (Karuranga et al., 2017), ensuring that patients are actively involved in self-care (Loan et al., 2018).
Given the social gradient of the older contingent of the population, which, owing to higher vulnerability calls for adaptation in the delivery of healthcare services, the objective of this study was to identify, synthesize, and assess the available evidence on the aims and effects of interventions used by health professionals for older adults with low health literacy.
Methods
This systematic review of the literature with meta-analysis was registered on the International Prospective Register of Systematic Reviews (PROSPERO) under no. CRD42018087014 and was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement (Moher et al., 2009). The study centered on addressing the research question devised based on the PICO (Problem/population, Intervention, Control and Outcomes): what were the aims and effects of interventions used by health professionals for older adults with low health literacy?
Search strategy
The databases searched were Medline (via PubMed), COCHRANE library, PsycINFO, SCOPUS, Web of Science, Scientific Electronic Library Online (SciELO), Literatura Latino-Americana e do Caribe em Ciências da Saúde (LILACS) and the Banco de Dados em Enfermagem (BDENF). The search strategy entailed the use of Health Descriptors (Descritores da Saúde - DeCS) and Medical Subject Headings (MeSH), in their possible permutations, using the Boolean operators AND/OR: Health Literacy and health personnel. Although the problem (P) was related to older adults with low health literacy, it was decided not to include the descriptor (MeSH) “aged” (entry terms Elderly) in the search because it acted as a limiter. The references of the articles included in the review, and of other relevant reviews, were hand-searched (Clement et al, 2009; Lowe et al, 2013). The selection process commenced in December 2017 and was finalized in April 2020, where 2000 was defined as the lower limit for publication date. The Medline search strategy (via PubMed) applied is outlined in Table 1.
Table 1 PubMed Search Strategy
| Search strategy | Total of articles | |
| #1 | "Health Literacy"[Mesh] OR "Health Literacy" OR “Literacy, Health” | 7,870 |
| #2 | "Health Personnel"[Mesh] OR "Health Personnel" OR “Personnel, Health” OR “Health Care Providers” OR “Health Care Provider” OR “Provider, Health Care” OR “Providers, Health Care” OR “Healthcare Providers” OR “Healthcare Provider” OR “Provider, Healthcare” OR “Providers, Healthcare” OR “Healthcare Workers” OR “Healthcare Worker” | 641,433 |
| #3 | ((("Health Literacy"[Mesh] OR "Health Literacy" OR “Literacy, Health”))) AND (("Health Personnel"[Mesh] OR "Health Personnel" OR “Personnel, Health” OR “Health Care Providers” OR “Health Care Provider” OR “Provider, Health Care” OR “Providers, Health Care” OR “Healthcare Providers” OR “Healthcare Provider” OR “Provider, Healthcare” OR “Providers, Healthcare” OR “Healthcare Workers” OR “Healthcare Worker”)) | 1,871 |
| #4 | ((("Health Literacy"[Mesh] OR "Health Literacy" OR “Literacy, Health”))) AND (("Health Personnel"[Mesh] OR "Health Personnel" OR “Personnel, Health” OR “Health Care Providers” OR “Health Care Provider” OR “Provider, Health Care” OR “Providers, Health Care” OR “Healthcare Providers” OR “Healthcare Provider” OR “Provider, Healthcare” OR “Providers, Healthcare” OR “Healthcare Workers” OR “Healthcare Worker”)) | 1,283 |
Study selection
After reading article titles and abstracts, studies were screened according to the eligibility criteria for inclusion: a) original study articles in which health professionals planned, applied, or evaluated interventions for older adults with low health literacy; b) involving populations aged ≥ 50 years and/or with mean age ≥ 60 years. The age bracket for older adults was broadened to reflect the importance of health promotion and disease prevention in individuals aged under 60 years (WHO, 2015); c) randomized clinically-controlled trials; d) published in Portuguese and English; and for exclusion: e) Studies which involved the planning, application or evaluation of health education interventions but did not draw on the health literacy concept, despite including older participants; f) non-clinically-controlled trials, discussion articles, editorials, summaries, notes, books, book chapters, abstracts presented at annals of congresses, dissertations, theses, qualitative studies, bibliographic studies, documental (desk)-based studies, case studies, and surveys.
Study selection was performed by searching the scientific databases, identifying potential studies based on title, abstract and key words. The articles retrieved were then screened by reading the full texts. Selection differences were discussed and resolved by consensus. When no consensus could be reached, a third researcher was consulted to deliberate on the issue.
Quality assessment
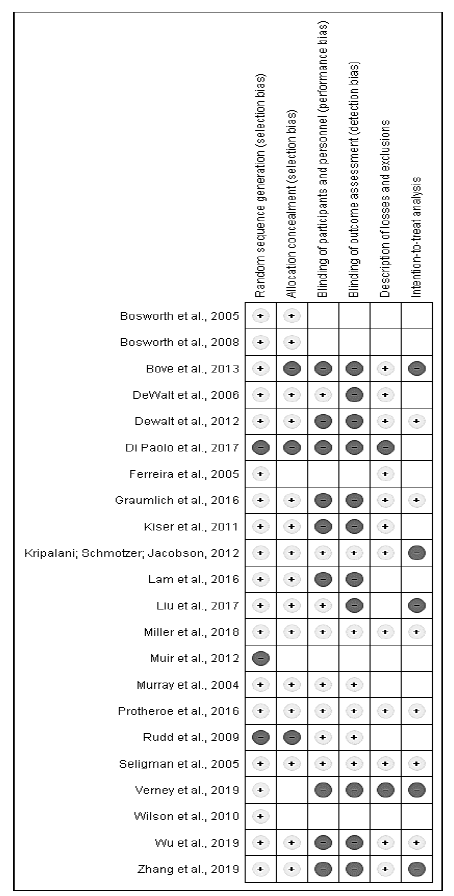
The Cochrane Handbook for Systematic Reviews of Interventions was used to assess the quality of the articles (Higgins, 2011) and the following study characteristics were rated: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, description of losses and exclusions, and intention-to-treat analysis. Studies lacking a clear description of these characteristics were classified as unclear or not reporting these items.
Data analysis
The meta-analysis was performed using the random effects model and measures of effect were based on post-intervention values. For the meta-analysis, a comparison of health literacy strategies versus control group or usual care in the assessment of glycemia and hypertension outcomes was carried out. An alpha value = 0.05 was adopted as statistically significant. The heterogeneity statistic of treatment effect among studies was assessed using Cochran´s Q-test and the inconsistency test (I2). All analyses were performed using the software Review Manager 5.1 (Cochrane Collaboration).
Results
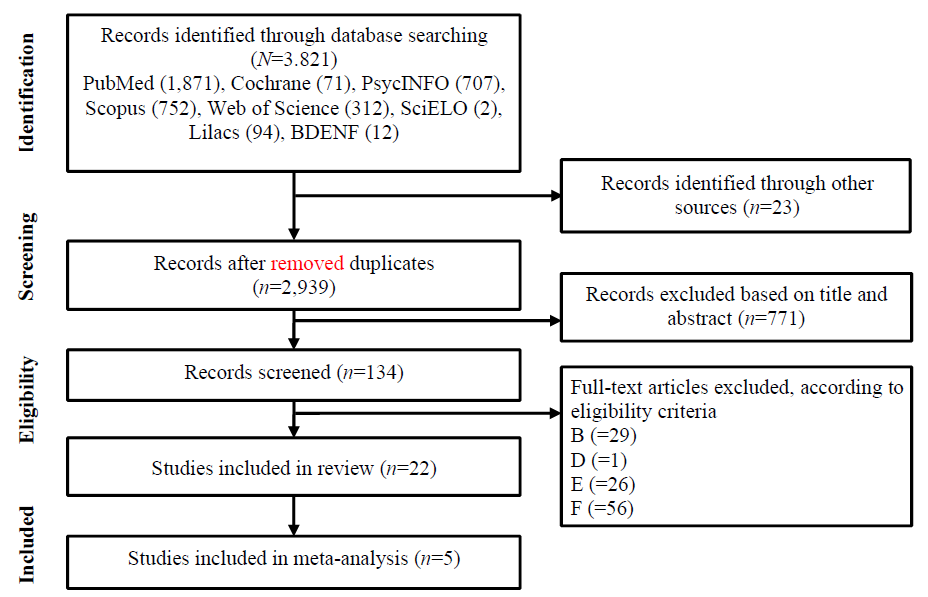
The flow chart of the study selection process is depicted in Figure 1. The 2,939 records (after removal of duplicates) were screened based on title and abstract. A total of 134 studies were eligible for review of full text. Overall, a total of 22 studies were included in the present review.
Description of studies
A synthesis of caractheristics of the studies, including information on setting and methodology, is given in Table 2.
Of the studies that carried out an assessment of health literacy, 2 (10.53%) used the results to select the study sample, comprising older adults with low health literacy (DeWalt et al., 2006; Lam et al., 2017). Low or limited health literacy levels were found in most of the studies (Bosworth et al., 2008; DeWalt et al., 2012; Graumlich et al., 2016; Kiser et al., 2012; Kripalani et al., 2012; Miller et al, 2018; Protheroe, 2016; Seligman et al., 2005). A longitudinal study found major disparities in scores among individuals with different age, skin color and gender (Verney et al., 2019).
Intervention strategies
The interventions employed different technical resources and methodologies (Table 3). Approaches included cognitive training sessions (Verney et al., 2019), an individual self-management educational intervention (Kiser et al., 2012), use of the teach-back method (Liu et al., 2018) and FamLit (Wu et al., 2019), delivery of written material containing practical accessible information about the health/disease status of the target subjects of the intervention, complemented by consultations with professionals (DeWalt et al., 2006; Rudd et al., 2009), use of graphically-enhanced interventions (Kripalani et al., 2012), videos accompanying booklets (Di Palo et al., 2017; Ferreira et al., 2005; Muir et al., 2012; Wilson et al., 2010), and use of telemedicine or telephone for educational intervention or support/follow-up (Bosworth et al., 2008; Bove et al., 2013; DeWalt et al., 2012; Muir et al., 2012; Protheroe, 2016). Some interventions employed tailored interventions via an iPad app, mPATH-CRC, as a tool for improving Colorectal Cancer Screening rates (Miller et al., 2018) and the digital Medtable program (Graumlich et al., 2016) and Talking Pill Bottles (Lam et al, 2017), both for pharmacy care. One study used the group method to promote interactive exchanges, scenario simulations and other activities (Zhang et al., 2019).
The period for which strategies were applied ranged from short-term (1-3 months), medium-term (6-12 months) to long-term (24-36 months and 10 years).
Table 2 Characteristics of Included Studies and Results for Primary Outcomes
| Author | Country | Population | Study Design / Sample | Health Literacy Test | Professionals involved |
|---|---|---|---|---|---|
| Zhang et al. | China | Hypertensive community-dwelling patients from Pundong new area in Shanghai. | RCT, N=1618 (I: 1041; C: 577). Age: 35-80 years. | Health Literacy Management Scale | Specialists. |
| Wu et al. | United States of America | Heart failure patients and primary care partners. | RCT, N=47 (I: 23; C: 20). Mean age: 66 years. | Not evaluated | Interventional medical practitioner with experience in cardiovascular care. |
| Miller et al. | United States of America | Population of urban, suburban, and rural area, served by academic health system. | RCT, N=450 (I: 223; C: 227). Age: 50-74 years | Single-item screening question. | Research assistant. |
| Liu et al. | China | Nursing home residents. | RCT, N= 260 (I: 126; C: 134) Mean age: I: 79,18; C:79,07 | Chinese Citizens Health Literacy Questionnaire. | Nurses. |
| Di Palo et al. | United States of America | Patients hospitalized with HF, recruited from 35 hospitals. | RCT, N=120 (I: 51; C: 43). Mean age: I: 69.7; C: 67.9 | Not evaluated | Interdisciplinary Team of the Navigator Team (NT) (Nurse, Pharmacist and Nutritionist). |
| Lam et al. | United States of America | Users of two community pharmacies, with prescription for hypertension. | RCT, N=134 (I: 68; C:66). Mean age: I: 68.9; C: 71.1 | Short-Test of Functional Health Literacy in Adults (S-TOFHLA). | Pharmacists. |
| Protheroe et al. | United Kingdom | Patients with Type 2 Diabetes Mellitus, recruited from family physicians. | RCT, N=76 (I: 39; C:37) Mean age: 64.7 years. | New Vital Sign (NVS). | Lay Health Trainers (LHT)* and Nurses |
| Graumlich et al. | United States of America | Population with Type 2 Diabetes Mellitus, attended at outpatient clinics. | RCT, N=674 (I: 326; C: 348). Mean age: 63.8 years. | Rapid Estimate of Adult Literacy in Medicine (REALM). | Nurses. |
| Bove et al. | United States of America | Urban population with high incidence of hypertension and diabetes, recruited from two medical centers. | RCT, N=241 (I:120; C:121). Mean age: 61 years. | Not evaluated | Nurses. |
| DeWalt et al. | United States of America | Population treated in four general clinics of internal medicine and cardiology. | RCT, N=605 (I: 303; C: 302). Mean age: 60.7 years. | Short Test of Functional Health Literacy in Adults (S-TOFHLA) in Adults (S-TOFHLA) in English or Spanish. | Health educator. |
| Muir et al. | United States of America | Population treated at a Medical Center. | RCT, N=127 (I: 67; C: 60). Mean age: 66 years. | Test of Functional Health Literacy in Adults (TOFHLA). | Doctors and adequately trained study coordinator. |
| Kripalani et al. | United States of America | Population attended in primary health care clinics. | RCT, N= 435 (I1: 121; I2: 102; I3: 116; C: 96) Mean age: 63.7 years. | Rapid Estimate of Adult Literacy in Medicine (REALM). | Doctors and Nurses. |
| Kiser et al. | United States of America | Randomized controlled trial conducted in a general academic internal medicine practice. | RCT, N=99 (I: 67; C: 32). Mean age: 63 years. | Short Test of Functional Health Literacy in Adults (S-TOFHLA). | Pharmacist, Doctor and Research Assistant. |
| Wilson et al. | United States of America | Men treated in oncology departments of two major urban hospitals. | RCT, N=70 (I1: 24; I2: 23; C: 23). Mean age: 67.4 years. | Rapid Estimate of Adult Literacy in Medicine (REALM). | Nurses. |
| Rudd et al. | United States of America | Population treated at an Arthritis Center of a teaching hospital. | RCT, N=127 (I: 16 (25%); C: 27 (43%)). | Arthritis-Adapted Rapid Estimate of Adult Literacy in Medicine (A- REALM). | Doctors, Educators and Research Assistants. |
| Bosworth et al. | United States of America | Population with hypertension, recruited in two primary care outpatient clinics. | RCT, N=636 (I; 319; C: 317). Mean age: 60.5 years. | Rapid Estimate of Adult Literacy in Medicine (REALM). | Nurses. |
| DeWalt et al. | United States of America | Patients with HF, attended at the University Center for the Practice of Internal Medicine. | RCT, N=127 (I: 62; C: 65). Mean age: IG - 63 years and CG - 62 years. | Short Test of Functional Health Literacy in Adults (S-TOFHLA). | Doctors, Pharmacists and Health Educators. |
| Bosworth et al. | United States of America | Population with hypertension, recruited in primary care outpatient clinic. | RCT, N=588 (I: 294; C: 294). Mean age: IG - 63 years CG - 64 years. | Rapid Estimation of Adult Literacy in Medicine (REALM). | Nurses. |
| Ferreira et al. | United States of America | Men aged 50 and over were recruited from two medical centers. | RCT, N=1.978 (I; 1015; C: 963). Mean age: 67.8 years. | Rapid Estimation of Adult Literacy in Medicine (REALM). | Doctors, Residents, Doctor Assistants and Nurses. |
| Seligman et al. | United States of America | Patients with Type 2 Diabetes Mellitus, treated at a public university hospital. | RCT, N=182 (I: 95; C: 87) Mean age: IG - 62.3 years CG - 63.4 years. | Test of Functional Health Literacy in Adults. Short version in English and Spanish. (S-TOFHLA). | Bilingual research assistants. |
| Murray et al. | United States of America | Population with HF, recruited at the Primary Health Care Center of the University. | RCT, N=314 (I: 122; C: 192). Mean age: IG - 61.4 years | Not evaluated | Pharmacists and Doctors. |
Nota. * Term adopted in the United Kingdom to define persons living in the local community who provide psychological and behavioral care and have received training from the UK National Qualification Nucleus.
Table 3 Synthesis of Interventions and Results for Primary Outcomes
| Author | Intervention | Control | Length of intervention and follow-up | Outcomes | Results |
|---|---|---|---|---|---|
| Zhang et al. | Group strategy for sharing experiences and scenario simulations. | Usual care. | Intensive intervention: six 1-to-1.5-hour sessions per week. Follow-up management: monthly 1h-sessions. | Self-management of community-based hypertension. | There was a significant difference in general health after the intervention for the intervention group (P < .001), with no significant difference in the control group. |
| Wu et al. | FamLit intervention guide in personal and telephone reinforcement sessions and the "Teach-To-Goal" approach | A face-to-face session focusing on the overall health of the patient. | Personal intervention sessions of 60 min for 3 months, and follow-up 3 months after the intervention. | Medication adherence and the sustained positive effect with the continued support of the care partner | The FamLit intervention group showed better medication adherence than the care control group at 3 months (87.6% vs. 80.9%), and at 6 months (87.8% vs. 74%). Medication adherence was maintained in the intervention group but decreased in the control group over time (F = 5, P = .03). |
| Verney et al. | Advanced Cognitive Training for Independent and Vital Elderly (ACTIVE): training in memory, reasoning, and processing speed in health literacy. | Contactless control, single-masked trial. | Ten sessions of 60-75 minutes, with a maximum of 5participants per group. 6-week interval between sessions, with additional reinforcements 11 and 35 months after initial training. | To investigate predictors of health literacy at baseline; explore changes in health literacy over a period of 10 years and investigate the effects of cognitive training on health literacy. | The effects of the intervention were not significant for all three cognitive training interventions: (beta = .025, 95% CI (- .095, .045); P = .478); reasoning (beta = -.016, 95% CI (-.054, .087); P = .653); and processing speed (beta = .007, 95% CI (- .063, .077); P = 841). |
| Miller Jr. et al. | 8.6-minute view about colorectal cancer screening using iPad application (mPATH-CRC) as a decision aid for colorectal cancer screening; sending automated follow-up electronic messages to support patients. | A 4.3-minute video about diet and exercise. | Screening within 24 weeks and 3 to 10 follow-up electronic messages. | Primary: Completion of a colorectal cancer screening test within 24 weeks of enrollment. Secondary: ability to indicate a preference for screening, intent to receive screening, screening discussions, and screening test requests. | mPATH-CRC group, relative to control group, showed greater chance of performing screening test (30% vs. 15%); having screening preference (97% vs 71%); planning their screening in 6 months (62% vs. 49%) and of discussing screening (76% vs. 48%). |
| Liu et al. | Handout with 66 indicators for literacy of Chinese citizens and use of teach-back method through interviews. | Traditional method. | 6 months. | Improvement of health literacy in individual or group on four dimensions (health knowledge, health beliefs, health behaviors and health skills). | Overall health literacy score was significantly higher (P < .05) in intervention group compared to control group. |
| Di Palo et al. | Patient Navigator Program of the American College of Cardiology: booklet and video adapted to health literacy and numeracy. | Usual care. | Multiple 60-minute sessions throughout hospitalization and one consultation 14 days before discharge. | Primary: Identification of hospitalized patients with HF; reduction of rate of readmissions for all causes in 30 days. Secondary: education and monitoring. | 94 (78.3%) hospitalizations confirmed as HF. There was no statistical difference between I and C groups in the 30-day HF readmission rate. Specific HF education (P = .0002); Follow up after 14 days between the group (p = .0044). |
| Lam et al. | Received antihypertensive medication and advice through Talking Pill Bottles (recordings of pharmaceutical advice). | Received medicine and usual care instructions. | 90 days. | Primary: knowledge of medication, adherence to medication, control of blood pressure (BP) and self-efficacy. Secondary: Acceptability of the use of the Talking Pill Bottles. | There was no statistical difference between I and C groups on measures of medication knowledge, self-efficacy, adherence to medication and BP control. The intervention was well-accepted by patients with low literacy: easy device control (89%); (77%) and correct medication use (74%). |
| Protheroe et al. | Individual interview with Lay Health Coaches for the patient to identify areas where they could improve their health; development of an individualized self-management plan with specific goals. | Usual care. | One meeting and three phone calls per month over a six-month period. Follow up after 7 months. | Perception of the disease, management of self-care, mental health well-being and better quality of life. | There was statistical significance between I and C groups only for mental health outcomes (P = .049) and disease perception (P = .040). |
| Graumlich et al. | Application of Medtable, structured tool, implemented in the electronic medical record in outpatient clinics to organize patient / professional collaborative interactions for medication and health education review. | Usual care. | Clinical visits with instructions to organize the medication list around the patient's daily activities. Follow-up after three and six months. | Primary: knowledge of medication and effect of intervention. Secondary: medication adherence, satisfaction, and glycemic control. | There was no statistical significance for intervention effect, drug use, adherence to the regimen or glycemic control (HbA1c). |
| Bove et al. | Application of Telemedicine: use of Internet-based communication system and telephone for programmed transmission of bidirectional data between the patient and the practice. Received a sphygmomanometer, scale and pedometer and instructions on their use. | Received the data from initial evaluation and instructed to contact primary care provider for more care. | Contact via the Internet or via voice messages on the phone, twice a week, with reminders every 2 weeks for six months. | Control of hypertension and adherence to medication. | There was no statistical difference between I and C groups for control of BP or adherence to medication. |
| De Walt et al. | 40-minute HF training, sensitive to literacy followed by support via telephone. | 40-minute training, sensitive to literacy. | For 4 weeks, 5 to 8 telephone calls lasting 10 min. each. After calls every two weeks. Follow-up: 1, 6 and 12 months after. | Primary: combined incidence of hospitalization for all causes or death. Secondary: hospitalization related to HF and HF-related quality of life. | There was no statistical difference between I and C groups for the incidence of hospitalization for all causes or death and HF-related QOL. |
| Muir et al. | Informative video on glaucoma with language adapted for health literacy level: 4th grade, 7th grade, or 10th grade | Usual care. | Individual session of 20 min. and monthly telephone calls, for a period of six months. | Primary: number of days without medication *. Secondary: medication possession ratio * | There was no statistical difference in adherence to medication between I and C groups. Individuals with inadequate or marginal health literacy skills were more likely to report the presence of a physical disability that made the instillation of adequate eye medication more difficult (p = .020). Decrease in health literacy skills was associated with decreased self-reported satisfaction with care (P = .002). |
| Kripalani et al. | After the initial consultation, illustrated medication schedules with name, indication and dosage instructions for each drug in simple language were given and a colorful picture of each medicine and an icon to indicate its purpose. | After initial consultation, they received reminders through the post approximately 25 days after the last medication filling, illustrated medication schedules, or both interventions. | Initial consultation and contact via letter every 2 weeks and telephone calls every three months for 24 months. | Adherence to the refill of cardiovascular medications. | There were no statistical differences in the rate of adherence between groups I and C groups, nor between patients with and without refill data. |
| Kiser et al. | Individual self-management education from a literacy-sensitive leaflet, with illustrations of the appropriate technique for inhaler use. Use of the teach-back method. | Usual care. | Individual session of 15 to 30 min. Follow-up after 2 to 8 weeks. | Use of appropriate inhalation technique. | There was no significant difference in the inhalation technique scores between I and C groups. Health literacy did not show significance for inhalation technique between groups. |
| Wilson et al. | Videos and pamphlets with information on radiation and its side effects and lifestyle, easy to read. One group participated in behavioral contracting. | Usual care. | Three sessions of 15 min. throughout the treatment. Follow-up at 3 and 6 months. | Self-care behaviors in the management of radiation side effects. | There was statistical significance between the three groups (2 I and 1 C) for the patterns of change in the use of radiation self-care techniques (P = .03). |
| Rudd et al. | Information materials written between the 5th and 8th grade reading level and two individualized sessions with an arthritis educator. | Leaflets on arthritis written between the 11th and 15th grade reading level and model calendars for medicine and a hospital map. | 20 min sessions follow-up after 6 and 12 months. | Primary: adherence to treatments, self-efficacy, satisfaction with care and maintaining appointments. Secondary: health and mental health status. | There was statistical significance between I and C groups for mental health measures at six and twelve months of intervention (P = .03 and .01). There was no significant difference between I and C groups in adherence to treatment, self-efficacy, satisfaction, and maintenance of commitments. |
| Bosworth et al. | Behavioral / educational intervention through personalized telephone counseling and pictorial handouts. | Usual care. | Individual and telephone meetings every 8 weeks for 2 years. Follow up at 6 months and 24 months. | Adherence to medication and improvement of health behaviors related to hypertension. | There was a percentage increase in the intervention group compared to the control group for adherence to self-reported medication (increase of 9% vs. 1%). |
| De Walt et al. | Educational booklet written below the 6th grade reading level, with images; provision of a digital weighing scale and scheduled telephone monitoring, emphasizing self-care for daily weight measurement, diuretic dose self-adjustment and symptom recognition. | General education brochure on heart failure written at the 7th grade reading level and continued with the usual care from doctor. | Individual session and scheduled phone calls of 5-15 min. (days 3, 7, 14, 21, 28, 56) and monthly, with follow-up during the third and sixth month, for 12 months. | Influence on death rates, reduction of all causes of hospital readmission due to HF, improve quality of life, self-efficacy, knowledge, and behaviors of elderly with HF and low health literacy. | There was no statistical difference in hospitalization or death rates, quality of life, knowledge and self-efficacy between I and groups C. There was statistical significance for behavior, such as monitoring weight daily (IG: 79% vs. CG: 29%, P < .0001). |
| Bosworth et al. | Standard and personalized telephone information in nine modules on literacy, knowledge about hypertension, memory, social support, patient / provider communication, medication refills, missed appointments, health behaviors, and side effects. | Usual care. | Telephone contact from 1 to 40 min. every 2 months for 24 months. | Communication between the patient and the health professional; knowledge about hypertension; drug adherence; self-efficacy and health behaviors. | There was no statistical difference in knowledge and medication adherence between I and C groups. There was statistical significance between I and C groups for self-efficacy with treatment for hypertension (P < .007). |
| Ferreira et al. | Brochure and video with simplified cognitive information on colorectal cancer and its screening, including social and emotional messages designed to motivate and empower patients to overcome barriers and increase self-efficacy. | Usual care. | Clinical visit. Follow-up ranging from 6 to 18 months. | Increase colorectal cancer screening rates. | There was statistical significance for the conclusion of screening tests for colorectal cancer between I and C groups (41.3% vs 32.4%, P < .003). Among the patients with health literacy skills lower than the ninth year, screening was completed by 55.7% of patients in IG versus 30% of patients in the CG (P = .01). |
| Seligman et al. | The communication between physicians and their patients with low health literacy was explored. | Usual care. | Clinical visit and follow-up for 12 months. | Self-efficacy to successfully manage chronic disease. | There was no statistical difference for self-efficacy post-visit and glycemic control of the patients, although HbA1c showed a decrease of .21% in IG and a .05% increase in CG. |
| Murray et al. | Focus groups; verbal education, written leaflets, and use of special medication containers, followed by computerized therapeutic monitoring. | Usual care. | 4 years of study. Nine months of intervention and computerized therapeutic monitoring for 3 months post-intervention. Follow-up at six and 12 months. | Adherence to cardiovascular drugs, prevent exacerbations and improve health-related quality of life, and patient satisfaction with pharmacy services and total direct costs. | There was no significant difference for the primary outcomes, however, these showed an improvement during the 9-month intervention period, which dissipated within 3 months post-intervention. |
Nota. * Both related to medication adherence. The presence of comorbidities, knowledge of the self-reported disease and satisfaction with care were also evaluated as results in relation to the measured level of health literacy.
Regarding intervention follow-up, most studies assessed results before and immediately after interventions, where follow-up periods for 8 (36.36%) studies were 1-, 6- or 12-months post-intervention, whereas 2 (9.09%) interventions involved ongoing assessments of results every 30 days. One longitudinal study involved assessments shortly after intervention and again at one, two, three, five- and ten-years post-intervention.
Concerning the aims of interventions, 11 (50%) studies focused on older adults diagnosed with heart disease, 3 (13.64%), 3 involved interventions for older patients with diabetes mellitus and 3 (13.64%) focused on cancer. In addition, there were interventions aimed at patients with glaucoma, rheumatoid arthritis, chronic obstructive pulmonary disease and at improving level of health literacy. The studies which applied interventions in older adults with heart disease sought to improve health outcomes by optimizing treatment, behavior and control of blood pressure, self-management and reducing rates of treatment or readmission. The strategies planned for older adults with diabetes mellitus sought to improve self-management in care and in controlling blood sugar levels, encouraging behavioral changes through healthy life-style choices and self-management of the condition (Protheroe, 2016), promoting better use of prescribed medications (Graumlich et al., 2016) or exploring physician-patient communication (Seligman et al., 2005). The studies on cancer employed strategies for increasing screening and self-care behaviors. However, primary, and secondary outcomes differed methodologically in terms of the means of assessment adopted, where authors applied published scales, specific instruments for the condition investigated, or used instruments they had devised and published. Adherence to medication and treatment was the most assessed outcome class (50.0%). Other outcomes assessed included health knowledge held (22.73%), self-efficacy (22.73%), quality of life (18.18%), physical and mental health (9.09%) and health behaviors (27.27%). Patient-professional communication, lifestyle and social support were measured (4.55%), as well as perception of the disease and self-care (9.09%), cognitive domains, memory, and reasoning (4.55%). Satisfaction was rated by 5 studies (22.73%), one of which measured patient satisfaction with pharmacy services and total direct costs. Concerning clinical outcomes, 3 studies assessed heart failure measures (13.64%), 3 blood pressure values (13.64%), 3 diabetes control (13.64%), while 2 assessed mortality and all-cause readmission for heart failure (9.09%).
Effects of Interventions
With regard to results, of the 22 studies reviewed, 3 (13.64%) reported statistically significant differences in primary outcome measures favoring the intervention groups (Ferreira et al., 2005; Liu et al., 2018; Wilson et al., 2010) and 5 (22.73%) found significant results for 1, 2 or 3 secondary outcomes (Bosworth etal., 2005; DeWalt et al., 2006; Graumlich et al., 2016; Protheroe, 2016; Zhang et al., 2019). Thirteen studies (59.09%) reported no statistically significant differences between groups. One study (4.55%) (Murray et al., 2004) observed improvement in primary outcomes at the time of the intervention, but loss of these gains during the post-intervention period.
Although not all outcomes differed statistically between intervention and control groups in the studies, most interventions had a positive effect on intragroup scores, as evidenced by comparisons of baseline versus post-intervention values.
Regarding significant results of interventions reviewed, a study investigating outcome adherence to colorectal cancer screening promoted a significant increase in disease screening rates (Ferreira et al., 2005). In the intervention group, 41.3% of patients underwent fecal occult blood tests, flexible sigmoidoscopy, or colonoscopy versus 32.4% of control group subjects (P<0.003). According to the authors, this result confirmed that a health care provider-directed intervention based on training workshops and individualized feedback on screening rates significantly increased adherence to colorectal cancer screening among older adults treated at a general clinic of a large urban area, supporting wider implementation of this type of intervention. A study addressing the outcome self-care behaviors in managing radiation side effects in prostate cancer found that self-care behaviors significantly increased in the intervention group compared to the control group from baseline to 6 months (P=0.05) (Wilson et al., 2010). Another study, assessing patients´ general health status, self-management skills and disease-management abilities identified an interaction between time and group (P<0.001) and statistically significant differences between the 2 groups for some variables in controlling behavioral risk factors such as drug compliance, physical activity, and diet (P<0.05) (Zhang et al., 2019).
Notable significant results for intervention groups include some actions centered on patients with heart failure, such as a study which applied the American College of Cardiology Patient Navigator Program (Di Palo et al., 2017). Specific education for HF was associated with statistical difference (P=0.0002), and documented education increased by 59% in the intervention group. There was a statistically significant difference in HF specific education (P=0.0002) and documented education increased by 59.0% among the intervention group. In addition, there was a statistically significant increase in scheduled 14-day follow-up prior to discharge in the intervention group (P=0.0044). The results showed that, of the scheduled appointments, patients included in the Navigator program were more likely to follow-up with a cardiologist (56.8%) than the control group (18.6%). The use of this program in the discharge process resulted in a 53.2% decrease in the number of patients discharged without a scheduled post-discharge follow-up visit. In another study, comparing the efficacy of a heart failure self-management program (DeWalt et al., 2006) results in the intervention group relative to the control, although only statistically significant for self-care behavior in terms of weight measurement, showed intragroup improvements for knowledge (mean difference in score improvement of 12 percentage points) (P<0.001) and self-efficacy (mean difference in score improvement of 2 points) (P=0.0026). A difference was also found for mortality and hospitalization rates, which were lower among intervention group patients.
The intervention group also had improved results in a study assessing knowledge and blood-pressure reading (Lam et al., 2017) showing significantly higher scores at day 90 post-intervention compared to baseline (P<0.001). Regarding self-efficacy of intervention participants, the study which tested the effect of a product launched 12 years ago in the USA called “Talking Pill Bottles” (Lam et al., 2017), consisting of a device with a base sized to accommodate most common prescription and a 60-second recording capacity, found that 101 of the 134 participants reported the highest level of confidence when faced with a situation of not having someone there to remind them to take their medication (M = 2.73, maximum score 3.0).
Self-efficacy, a secondary outcome of a study which applied an intervention for improving blood pressure control (Bosworth et al., 2005) showed a significant increase after treatment in the intervention group from baseline to 6-month follow-up, whereas the usual care group shown a decrease (P=0.007). Another study, aimed at enhancing health outcomes in arthritis patients, assessed the self-efficacy variable both at baseline and 6-months post-intervention (Rudd et al., 2009). Results showed improvement in the intervention group from baseline to 12 months compared to the standard care group. Differences between the groups were statistically significant at 6 and 12 months (P=0.05). By contrast, a study evaluating post-visit self-efficacy scores of diabetes patients found no significant difference between intervention and control groups (P=0.60) (Seligman et al., 2005). According to the authors, this lack of a difference in self-efficacy scores between the intervention and control group patients suggests that the management strategies physicians employed need to be reinforced over several patient visits.
Regarding health literacy level, one of the studies aimed at improving literacy found a significant result for the total health literacy score on 4 dimensions (health knowledge, health beliefs, health behaviors and health skills) in the intervention group relative to the control group (P<0.005) (Liu et al., 2018). Although detecting differences in health literacy in subgroups was not necessarily a goal of the other studies, some included analysis of subgroups according to literacy. For example, the study on self-management for heart failure demonstrated that, among other outcomes, the lower rate of hospitalization or death in the intervention group was greater for patients with low literacy (DeWalt el al., 2012). In a study aimed at reducing heart failure readmission rates, the intervention was tailored to patient´s health literacy and social needs (DiPalo et al., 2017). Results showed a strong correlation between the education intervention and readmission rate, with a lower rate of readmission in the group receiving the intervention which almost reached statistical significance (P=0.15).
In the study of Muir et al. (Muir et l., 2012) aimed at improving glaucoma medication adherence, subjects with inadequate or marginal health literacy skills were more likely to report the presence of a physical disability which made proper drop instillation more difficult (P=0.020). However, the number of days without medication in the 6 months following enrollment was similar for the control and control groups. For each literacy level, the number of days without medicine was fewer in the intervention than in the control group, and the magnitude of the difference increased as literacy decreased.
Ferreira et al. (2005), investigating colorectal cancer screening, found that among patients with health literacy skills less than ninth grade, screening was completed by 55.7% of patients in the intervention group versus 30% of controls (P< .01/ p=0.002). However, the study by Graumlich et al. (2016) found that patients who received the intervention had greater knowledge about indications for medications, irrespective of literacy status; the study by Protheroe et al. (2016) found evidence that the health literacy intervention can have a positive impact on the mental health of patients, while Kiser et al. (2002) found, in the literacy subgroup, greater improvement among COPD patients with low literacy compared to those with higher literacy. The results of the study by Lam et al. (2017) suggested that the intervention applied was well accepted by patients with low health literacy.
Risk of Bias
Regarding risk of bias (Figure 2), 86.36% of studies reported performing random sequence generation, under half of studies (42.1%) reported blinding of participants and 31.57% carried out blinding of outcome assessment. Description of losses and exclusions were included in 54.54% of the studies, whereas intention-to-treat statistical analysis was present in only 5 studies (27.27%).
Meta-analysis
The studies reviewed were highly heterogeneous for intervention strategies and outcomes analyzed. Consequently, the meta-analysis included only 3 studies comparing strategies for health literacy strategies versus control groups or usual care for the glycemia outcome (Graumlich et al., 2016; Protheroe, 2016; Seligman et al., 2005) and 2 studies comparing health literacy strategies versus control group or usual care for the hypertension outcome (Bove et al., 2013; Lam et al., 2017).
Review of the studies investigating glycemia outcomes revealed no statistically significant effect of the intervention for improving glycemia in this population [(0.19; 95%CI: -7.60, 7.98)] (Figure 3).
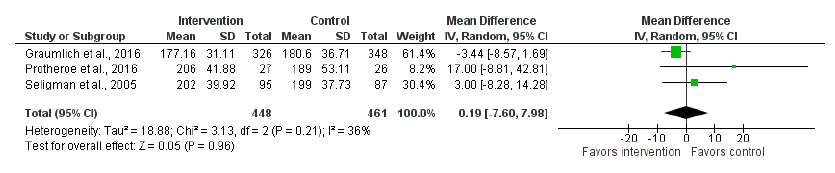
Figure 3 Strategies for Health Literacy vs. Control Group or Usual Care in the Evaluation of Blood Glucose Outcome
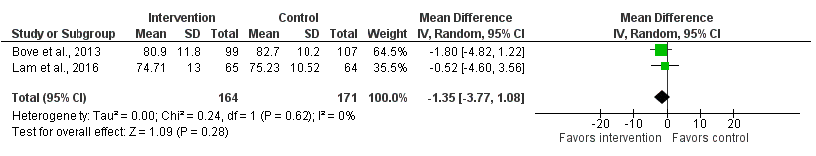
Similarly, the results of the meta-analysis of studies comparing health literacy strategies versus control group or usual care for the hypertension outcome (Bove et al., 2013; Lam et al., 2017) showed no significant effect of the interventions for absolute change in systolic and diastolic blood pressure in the population investigated - SBP [(-2.07;95%CI:-6.04,1.09)] (Figure 3); DBP [(-1.35;95%CI:-3.77,1.08)] (Figures 4 and 5).
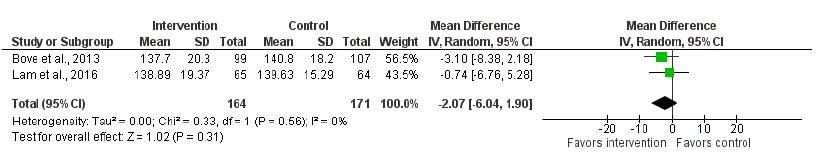
Figure 4 Strategies for Health Literacy vs. Control Group or Usual Care in the Evaluation of Diastolic Blood Pressure Outcome
Discussion
All included articles in this review were published internationally, pointing to the need to conduct more studies exploring this issue in Brazil. In the present systematic review, the evidence revealed that the goals of the interventions performed focused predominantly on disease and its management for improving behaviors such as adherence to medication and health outcomes. The results also revealed a dearth of actions aimed at promotion and prevention in this area and with a wider impact on living, socioeconomic and environmental health conditions of older adults, issues not addressed by the studies reviewed. This understanding is congruent with the recognition that healthy aging goes beyond absence of disease (WHO, 2015), calling for replacement of curative models by integral care centering on the needs of the aging population and considering the environments in which this population lives and interacts, including better quantifying resources and costs.
Regarding intervention effects, few results proved statistically significant, i.e., favorable for older adults with low functional health literacy and with potential to positively affect the health of these individuals. Given that results suggested subtle benefits of the interventions, these gains warrant further confirmation in larger studies with better methodological quality. The level of health literacy, in most studies, did not appear to be a determinant for the results obtained. However, it is important to note that the instruments used to assess health literacy level differed among studies and, although all evaluate functional health skills, associations with age differ and scores are variable. These findings corroborate some of the points made by Kobayashi et al. (2016), suggesting that theoretical understanding of health literacy and aging is hampered using instruments that assess a broad array of different constructs such as ‘health literacy”; the use of inconsistent measures of cognitive ability by the few studies examining cognitive processes and a lack of longitudinal studies exploring this topic.
The meta-analysis results of this study were not significant for glycemia or hypertension outcomes, showing that the health literacy interventions were ineffective for the target diabetic and hypertensive populations. This result may well change in the light of future studies involving larger samples with greater statistical power, but the current evidence remains inconclusive.
Limitations
This study has several methodological strengths, such as formulation of a specific research question, conducting of a systematic, comprehensive, sensitive literature search by 2 reviewers independently; where study selection, data extraction and analysis of methodological quality of the articles was also performed by 2 independent reviewers.
The RCTs reviewed were methodologically limited, whereby only 3 out of the 22 studies selected fully reported all the items rated in the bias assessment. The interventions reported in the studies reviewed varied greatly and targeted different outcomes, severely hindering the process of meta-analysis.
Comparison with other reviews
The present review differs to that of Clement et al. (2009) in scope, sample age and publication period, given the present study restricted its focus to intervention goals (health concerns) and effects, on older adults and more recent RCTs, having included 3 of the 16 studies covered in the cited review. Notwithstanding these differences, some results of the present review were similar to those found by Clement et al. (2009), namely, the methodological disparity among the studies reviewed in terms of length of the interventions, besides differences in complexity and in the measures employed, hampering the determination of evidence of effect.
Additionally, the samples involved resembled those of most of the studies in the systematic review by Lee et al. (2012), whose objective was to identify effective intervention strategies to improve health outcomes for heart disease patients with low health literacy skills.
These differences aside, the conclusions of the studies, including those of the present review, were largely in agreement, confirming that no reliable conclusive evidence is currently available on the most effective intervention strategy for improving the health of individuals with limited literacy (Clement et al., 2009; Lee et al., 2012).
The results of the present systematic review and meta-analysis suggest that the available evidence on the effect of interventions used by health professionals for older adults with low health literacy failed to promote statistically significant improvements in glycemia and hypertension outcomes. Adherence to medication and treatment, followed by self-efficacy and satisfaction, were the outcome classes assessed, but not included in the meta-analysis owing to the wide variety of different technical and methodological procedures employed in the studies reviewed. However, the positive effects observed for each type of intervention applied, yielding significant results for only some outcomes and improvements in intragroup scores, demonstrated the interventions applied had good acceptability by older adults with limited health literacy. It was not possible, however, to conclude which intervention strategies had a significant positive effect on improving health outcomes in these patients. Further randomized clinical trials of high quality and with greater methodological rigor in assessing results are warranted.
Funding
The present study was partially funded by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), under the National Program for Academic Cooperation (PROCAD).
Authors’ contributions
Helenice Scortegagna: Conceptualization, formal analysis, acquisition of funding, investigation, methodology, funding, validation, writing - review and adition.
Meire Cachioni: Methodology, project administration, supervision, writing - review and edition.
Sheila Zanini: Data curation, formal analysis, ivestigation, software, visualization, writing of original draft.
Vanessa Alonso: Visualization, writing - review and edition.
Ruth Melo: Methodology, visualization, writing of original draft.
Anita Neri: Conceptualization, metodolgy, project administration, supervision, visualization, writing of original draft.