INTRODUCTION
Brazilian jiu-jitsu (BJJ) is a physical and sports practice with a high level of contact, in which practitioners carry great combat with projection techniques (Del Vecchio, Bianchi, Hirata, & Chacon-Mikahil, 2007; Andreato et al., 2013) and attempting to dominate on the ground, to dominate the opponent through immobilisations, joint twists or strangulation (Jones & Ledford, 2012). Like other grappling fights, it is not uncommon for traumas and injuries to occur (Spano, Risucci, Etienne, & Petersen, 2019) when projection techniques are used, allowing the incidence of concussion.
A concussion is a traumatic brain injury induced by mechanical shock forces that affect the skull region (McDonald, Murdock Jr., McDonald, & Wolf, 2017; Lystad & Strotmeyer, 2018). This brain injury is inherent in the BJJ and is present in the practitioner’s daily life regardless of age, with an increase in its incidence linked to the quantity and density of the competition (Spano et al., 2019). Studies indicate that concussion in young people accounts for 3 to 8% of the incidence of all injuries at different ages (Kelly, Lissel, Rowe, Vincenten, & Voaklander, 2001); and that the high incidence in this age group may be related to the more significant proportion between head size and the body, weaker neck muscles or greater vulnerability of the developing brain (Sim, Terryberry-Spohr, & Wilson, 2008).
Previous reports have indicated the incidence of injury in combat athletes and found concussion and head injuries to be the most common (Karpman et al., 2016). Presently, prevention is designed into three broad categories: primary prevention (i.e., health promotion and specific protection against risk factors), secondary prevention (i.e., early detection, early treatment of health problems), and tertiary prevention (i.e., reducing complications associated with health problems already sustained. A Translating Research into Injury Prevention Practice framework (TRIPP) model looks at primary prevention (Mayer et al., 2015). TRIPP is needed in grappling sports (Pocecco et al., 2013; Kreiswirth, Myer & Rauh, 2014; Scoggin et al., 2014; McDonald et al., 2017; Miarka et al., 2018). In some cases, injury has occurred because injured athletes were allowed to continue training or fighting (Karpman, Reid, Phillips, Qin, & Gross, 2015; Miarka et al., 2019).
Despite the evidence showing a higher incidence of concussion in young athletes, Spano et al. (2019) reported no relationship between the occurrence of concussion in BJJ practitioners and the age group. The BJJ practitioner’s graduation can be a determining factor in susceptibility to having a concussion. The prevalence of injuries related to the belt ranking of the BJJ practitioners is higher in the white belts (42.5%) and blue belts (32.5%), with a predominance of injuries to the hand and fingers. According to Kamitani et al. (2017), the number of severe cases of head trauma in Judo athletes occurs in the first years of practice and competition. However, the comparison between the frequency of concussion cases by belt raking has not been realised. Therefore, this study aimed to analyse the association between belt ranking and the experience level in the BJJ, along with the incidence of concussion. We hypothesised that lower experienced practitioners showed a higher frequency of concussions. This study would assist in defining prevention and training methods to reduce possible damage caused by a concussion in the modality due to technical differences and experience in BJJ practice.
METHODS
This descriptive and documentary study evaluates a database about BJJ practitioners’ concussions.
Participants
An online link to the questionnaire was sent to 42 BJJ masters, or those responsible for the academies, and directly replicated through the social networks of approximately 75 BJJ schools and associations located in the United States. All participants were older than 18 years. The survey monkey platform hosted the questionnaire, which was programmed to filter, not allowing multiple responses from the same IP. Seven hundred ninety-one practitioners completed the survey in whole or in part; 13 participants were excluded because they were identified as under 18 years old. The database currently has 758 questionnaires answered by athletes in a public repository (link: https://www.mdpi.com/2075-663/7/2/53/s1). The sample calculation for 550 thousand federated practitioners obtained an n = 665, with a 99% confidence level and 5% margin of error, using Equation 1 (Francis et al., 2010):
The interpretation of each of these elements is made as follows:n = is the sample size obtained through the calculation;N = total population belonging to the survey;Z = indicated deviation from the acceptable mean value for the confidence level to be reached;e = is the maximum margin of error that the search allows;p = is the proportion we want to find in the calculation.
Following the previous protocols, no changes were demonstrated in the participants’ training, nutrition, or hydration status (Miarka et al., 2019). As provided in previous protocols, there are no ethical problems in investigating public and secondary data (Petrisor et al., 2019; Spano et al., 2019). The local Ethics and Research Committee previously approved the current research following the Helsinki WMA Declaration.
Measurement
The questionnaire had 17 questions, starting with demographic data and a previous survey about concussions suffered. The questions were related to age, gender, the number of times he suffered a concussion before joining BJJ, and how many times he suffered a concussion or became unconscious. Then, the questions were related to the practice of Jiu-jitsu: training time, frequency of weekly practice, and the total competitions that the athlete has participated in life, as indicated in the previous and valid protocol published by Spano et al. (2019).
Statistical analysis
All analyses were performed using SPSS software version 20.0 (SPSS, Chicago, USA). Descriptive data are presented as a percentage and absolute frequency. The Chi-square categorical test (χ2) was applied to assess the frequency of data prevalence. Pearson’s correlation was also performed to verify the association of concussion factors with the practice time and graduation of the BJJ practitioner. For all tests, the significance level of p ≤ 0.05 was used.
RESULTS
Seven hundred fifty-eight people answered the questionnaire. Of these, 186 people (23.2%) reported concussion cases during jiu-jitsu activity, and 566 people (74.7%) reported that they had no concussion in the practice of jiu-jitsu. The Chi-square test showed a significant difference between the level of practice about the moment when the first concussion occurred (χ2 = 721.44, df = 6, p ≤ 0.01), with a negative correlation between the ranking by degree and the moment when the first concussion happened (r = -0.875, p ≤ 0.01). The highest number of concussion occurrences occurred in the graduation of the white belt (n = 94; 49%), followed by practitioners of the blue belt (n = 64; 33.3%) followed by the purple belt (n = 18; 9.4%), brown belt practitioners in the fourth (n = 5; 2.6%) and black belt practitioners in the fifth position (n = 2; 1.0%). Some practitioners did not inform their graduation (n = 9; 4.7%) and were classified as “Not Answered.” Table 1 demonstrates the symptoms frequencies of concussion in Brazilian Jiu-jitsu, separated by belt.
Table 1. Symptoms frequencies of concussion in Brazilian Jiu-jitsu, separated by belt.
| Graduation | Symptom’s frequencies | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Headache | Dizziness | Loss of balance | Blurry vision | View stars | Blurred vision or slow movement | Memory problems | Low concentration | Nauseas | Vomiting | Loss of consciousness | |
| White | 70 | 65 | 36 | 31 | 37a | 49 | 25 | 36 | 24 | 5 | 9 |
| Blue | 49 | 46 | 21 | 20 | 39a | 40 | 17 | 27 | 17 | 5 | 5 |
| Purple | 13 | 10 | 5 | 8 | 9 | 13 | 2 | 7 | 4 | 1 | 1 |
| Brown | 5 | 3 | 2 | 1 | 1 | 4 | 3 | 3 | 2 | 1 | 2 |
| Black | 2 | 0 | 0 | 0 | 0 | 2 | 2 | 2 | 0 | 0 | 0 |
| Not declared | 3 | 2 | 1 | 1 | 2 | 3 | 2 | 2 | 1 | 1 | 1 |
| Total | 142 | 126 | 65 | 61 | 88 | 111 | 51 | 77 | 48 | 13 | 18 |
a Significant differences, when compared with other groups, p< 0.05.
Among the symptoms, blurred vision (χ2 = 5.552, df = 6, p ≤ 0.475) (r = -0.026, p ≤ 0.722), dizziness (χ2 = 6.910, df = 6, p ≤ 0.329) (r = -0.01, p ≤ 0.89), and headache (χ2 = 3.453, df = 6, p ≤ 0.75) (r = -.0054, p≤ 0.464), had no significant difference concerning concussion; however, there is a significant correlation in the group who reported “seeing stars” (χ2 = 11.614, df = 6, p ≤ 0.071) (r = 0.169, p ≤ 0.002), with white and blue belt practitioners, precisely the group that is most likely to have a concussion during training (Table 1).
Figure 1 shows the number of concussions per graduation and the time to return to BJJ training. There is a significant and strong correlation (χ2 = 190.964 df = 94, p ≤ 0.01) (r = -, 082, p ≤ 0.274) between the time to return to training in less than 24 hours and graduation, with the white and blue belt, the highest rates of practitioners who return quickly to training. Figure 2 shows the permanency of symptoms after a concussion.
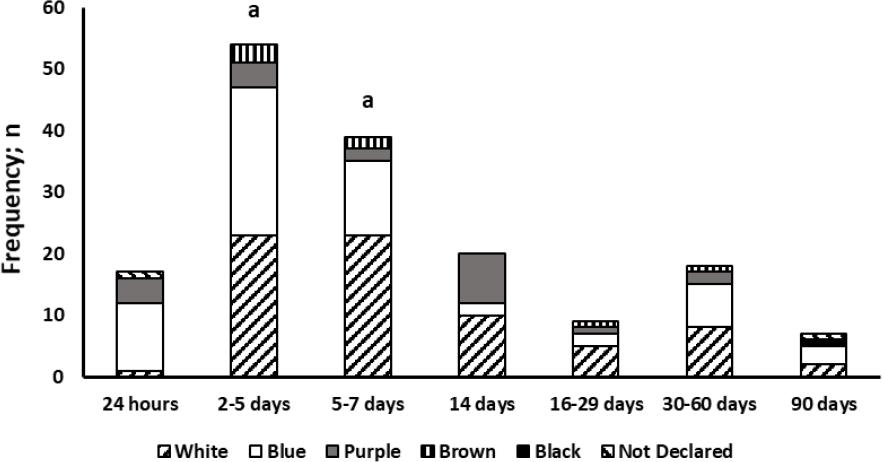
ap ≤ 0.01 white and blue belt vs. the others.
Figure 1. Occurrences of concussion per graduation and time to return to training.
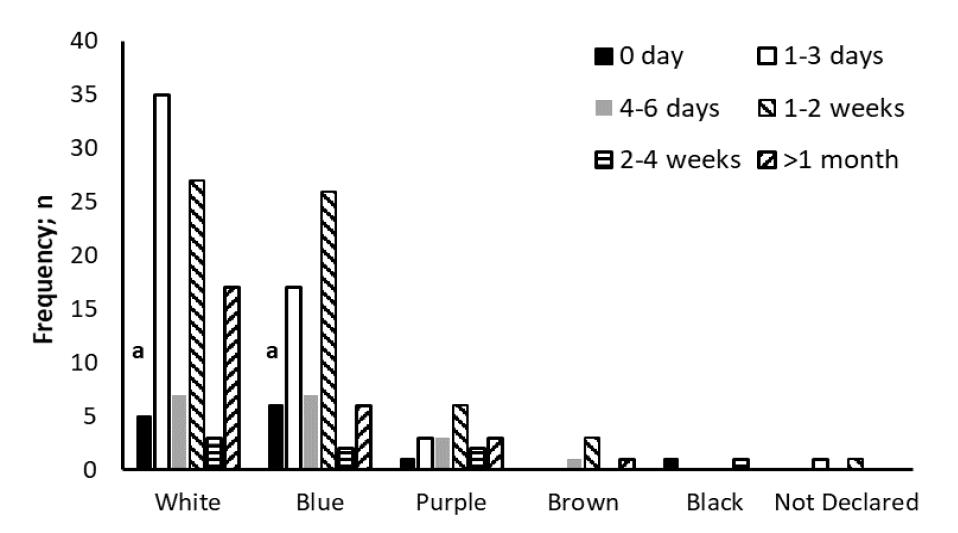
ap ≤ 0.01 white and blue belt vs. the others.
Figure 2. Duration of symptoms (days) after a concussion.
The frequency of practitioners seeking medical care has increased concerning graduation, indicating that respondents gain experience and start to seek medical care after a concussion at the time of practice. subjects with lower experience (white; n = 18, blue; n = 17, and purple; n = 8) are the least likely to seek medical care after concussion (χ2 = 14.874 df = 5, p ≤ 0.01) (r = -0.113, p ≤ 0.128) when compared to high experience subjects (brown; n = 3 and black; n = 2). Regarding the rest time after a concussion, practitioners of white and blue belts return faster than the others (χ2 = 190.964 df = 95, p ≤ 0.01) (r = -0.082, p ≤ 0.274), with few cases of purple belt practitioners, most of them return around the 14th day of rest, brown belts return between the 2nd and 30th day, whereas black belts take around 180 days to return to training. Regarding the repetition of concussion occurrences after returning to training, 14.6% (n = 27) are white belts, 7.6% (n = 14) blue belts, 2.7% (n = 5) purple belts and 1.1% (n = 2) black belts. Brown belt practitioners had no more than one occurrence of concussion.
DISCUSSION
This study analysed the association between BJJ belts and the incidence of concussion. The main results confirm that the practitioner’s technical inexperience and the absence of medical and technical monitoring by the coaches are a relevant part of the concussion occurrences. In contact sports, there is a higher risk of collisions with the head, which can lead to death in severe cases (Doperak, Anderson, Collins, & Emami, 2019). Due to the potential harm that concussion causes the athlete, sports federations have turned more attention to policy actions that can protect athletes (Spano et al., 2019). This type of effort has also been observed in combat sports organisations, where guidelines have been created to minimise the risk of concussion (e.g., stop the combat by the referee or a physician) in fighters (Bernick et al., 2021).
In combat sports, it is possible to observe manifestations of concussion such as that which occurred in knockouts and chokes (Hubbard et al., 2019). However, there must be educational campaigns to guide coaches, as the concussion diagnosis is not simple, and most observations do not necessarily result in loss of consciousness. (McCrory et al., 2013b). Therefore BJJ coaches must be aware of the concussion risks and be prepared to face and deal with these kinds of injuries is fundamental. Training in areas such as first aid, and in this case, the knowledge of head injuries and their risks should be part of the coach’s training (Matthew & Mill, 2018). There is a high probability of a concussion happening during training, so coaches having this additional knowledge would act as a risk reduction factor of concussions during training (Matthew & Mill, 2018; Petrisor et al., 2019).
It was evident that athletes returning to training in less than 24 hours present neglect of caring for the absence of a neuropsychological assessment was neglected according to guidelines from The Concussion in Sport Group, which has the purpose of assessing cognitive function as an essential component in evaluating the injury, following steps ranging from strength training to return to full-contact practise training (McCrory et al., 2013a). Because the practitioners who suffer concussions should be immediately removed from sports participation, in addition to a minimum of 24 to 48 hours of cognitive rest (McCrory et al., 2013a; Bernick et al., 2021). However, if symptoms persist between 10 and 14 days in adults or more than a month in children, they should be referred to a professional specialising in concussions for emergency care (Rabadi & Jordan, 2001; McCrory et al., 2013a).
According to Gross (1999), when the subject “seeing stars” is characterised as photopsia or phosphene. It is an entopic phenomenon characterised by the sensation of seeing light spots caused by the retina or visual cortex’s mechanical, electrical, or magnetic stimulation (Robbins et al., 2014). This luminous sensation, or luminous image, is triggered by the compression of the eyeball, which can occur when the neurons of the occipital lobe are depolarised (Gross, 1999; Robbins et al., 2014). This phenomenon causes several disorders such as migraine auras and can develop into severe symptoms such as retinal vascular avulsion (Zeni & Vilela, 2006), so the “seeing stars” is one of the most evident and immediate symptoms, as it generates an instant reaction to the moment of shock, while the other symptoms are usually noticed after this phenomenon (Robbins et al., 2014).
Preceding reports indicated that for high-performance athletes, who compete assiduously, an injury could have numerous consequences that can significantly compromise their sports career (McDonald et al., 2017; Miarka et al., 2019). For this reason, it is necessary to identify and analyse the methods that can reduce and prevent the risk of more severe injuries or improve the control by the professionals involved during physical and technical preparation, thus being able to avoid exposure both in training and in competitions (McCrory et al., 2013a; Lystad & Strotmeyer, 2018; Miarka et al., 2019; Bernick et al., 2021). In this sense, the return before than 24 hours after the injury may indicate little knowledge of the practitioners regarding the care and medical guidance regarding concussion (McCrory et al., 2013a). It can even demonstrate the lack of care/knowledge of those responsible for training in allowing a return in a short time, contradicting consolidated medical guidelines on head injury occurrences (Rabadi & Jordan, 2001; Brown, Grant, Evans, Leung, & Hides, 2021).
BJJ training is susceptible to shocks that can cause serious injuries, especially if there is no monitoring by those involved in training, either athletes or coaches (McDonald et al., 2017). In these situations, the BJJ practitioner has a high probability of being involved in a concussion during his life while training the BJJ (Matthew & Mill, 2018; Spano et al., 2019). Therefore, the athlete must be aware of the care when reacting with extreme and uncontrolled physical strength to a given stimulus during training. The absence of force control in the initial graduations is well known within the training sites and is even emphasised by the practitioners as a defect to be corrected. It is known that jiu-jitsu federations require first-aid training courses and primary medical care from teachers and black belts. However, the study did not score the participation of teachers who conducted the training in which the concussion occurred and their reaction concerning the initial assistance to the injured practitioner. It was also unclear which weight categories are most exposed to concussion. The training frequency was not analysed, so it was not possible to interpret whether the time to return to activities is related to training exposure (Rabadi & Jordan, 2001; McCrory et al., 2013a; Matthew & Mill, 2018).
There are limitations to the study because it was impossible to analyse when the concussion occurred in an opponent’s projection or during the ground fight. It was not possible to analyse when the concussion occurred because of fancy action provoked by the training partner during training and the training partner’s graduation in the concussion occurrence. It was not assessed when concussions occur in more significant numbers in training or competition. It was not analysed how the relationship was between concussions and the search for specialised medical services. However, the results demonstrated that most athletes return to training less than 24 hours after the concussion, pointing to possible negligence regarding medical care. This study addresses the first stage in BJJ of the TRIPP model, and future research can utilise the data to investigate risk influences connected with injury at different levels of experience. The TRIPP model could regulate the training actions and rules, considering graduation and expertise levels within a grappling context (Mayer et al., 2015; Miarka et al., 2018) and determine the consequence of concussions in BJJ athletes (Scoggin et al., 2014).
Such measures can reduce the occurrence of concussions during the practice of jiu-jitsu. There is a significant decrease in occurrences, which expresses that the time of practice in the modality generates the necessary experience for the athlete to avoid such injury. It is suggested that athletes train muscle strengthening in the neck so that during projections, muscle strength is more significant than kinetic strength, allowing the athlete to safely control the neck’s positioning to avoid injuries (Collins et al., 2014). Training with lower body intensity (controlled) can be used completely to develop and maintain a mentality of prevention and care with the training partner, who is directly responsible for the technical evolution of BJJ.
CONCLUSION
Our data analysis showed that concussions occur more frequently among beginners (white and blue belts). This group of practitioners deserves more attention from coaches, as they also showed a higher frequency of side effects. Coaches can create training strategies for white and blue belts to minimise the exposition. In this way, it is suggested that professionals who conduct BJJ training develop methodologies that specifically serve beginners. This methodology could be extended until the practitioner graduated with the purple belt. Our results suggested that knowledge of concussion symptoms is recommended for BJJ coaches and practitioners.















