INTRODUCTION
During the pre-COVID-19 vaccine period, the recovery prognosis was worrying, and the mortality of people infected by this disease was high (Kowsar et al., 2023). Additionally, commonly experienced clinical outcomes were hospitalization, length of stay, respiratory support, intubation, and mechanical ventilation (Gomide et al., 2022a; Gomide et al., 2022b). Such events can impair the quality of life of people diagnosed with COVID-19. These factors and changes imposed by social distancing measures have greatly affected people's quality of life (Mercieca-Bebber et al., 2023).
The World Health Organization defines quality of life as "an individual's perception of their life position in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns". During the outbreak, the quality of life of populations was reduced due to the risk of infection, mortality, and potential severe prognosis, also emphasizing the older and obese individuals (Kowsar et al., 2023; Mahmoodi et al., 2023). In addition, the recommendation for social distancing to contain the viral spread was combined with adopting a poorer health lifestyle that compromises the quality of life stability (Qi et al., 2020). For instance, during the COVID-19 first wave, general attitudes unfavourable to health were the reduction of total physical activity and greater caloric intake (Robinson et al., 2021). These behaviors have led countless people to increase body weight, the emergence of comorbidities associated with increased cardiovascular risk, and psychosocial disorders such as anxiety, loneliness, and depression, especially in older people (Sepúlveda-Loyola et al., 2020). In addition, this situation can aggravate people's quality of life in different aspects, including low family income, reduced social interaction, and illness, among others (Banks et al., 2011; Cureau et al., 2018; Gao et al., 2021; Sousa et al., 2021).
There are different proposals to measure and evaluate the quality of life. However, it generally seeks to verify variables such as functional capacity, global limitation, social aspects, pain, mental health, and vitality. Understanding quality of life as a multidimensional construct influenced by an intricate network of interconnected variables is crucial. Functional capacity, essential for daily activities and individual goals, serves as a key determinant. Global limitations impact the subjective perception of well-being. Social dynamics, encompassing social interactions and emotional support, bear relevance to mental state and overall satisfaction. The presence of pain, beyond limiting functionality, holds implications for mental health and vitality, influencing energy and mood. Mental health, intrinsically linked to quality of life, underscores the importance of emotional stability. Vitality, as an energetic attribute, contributes to an overall sense of health. The integrated assessment of these variables provides a holistic understanding of the determinants of quality of life (Campolina et al., 2011).
Therefore, neglecting quality of life can be a mistake, as observed that the risk of upper respiratory tract infection by SARS-CoV-2 was potentially higher in the presence of an impaired immune system due to unhealthy habits and a low quality of life (Ferreira et al., 2021; Nieman, 2020). Furthermore, female sex, older age, presence of comorbidities, intensive care unit admission and stay, and being mechanically ventilated are the most frequently reported factors associated with a low quality of life (Nandasena et al., 2022). Regardless of the time since discharge or recovery, COVID-19 patients’ quality of life has been significantly impacted.
However, quality of life was not verified in pre-diagnosis and post-recovery of people diagnosed with COVID-19. Additionally, sex, age, nutritional status, physical activity level, and family income have not yet been considered together to understand this impact, especially in middle-income countries such as Brazil. Thus, we aimed to compare the quality of life on pre-diagnosis and post-recovery of people diagnosed with COVID-19 and examine the impact of its signals, symptoms, and clinical outcomes on quality of life in adults and older adults, considering sex, age groups, nutritional status, physical activity level, and family income as confounding variables.
METHODS
Study design
This is a retrospective observational study. Data was collected between June and December/2021 from people diagnosed with COVID-19 between March/2020 and February/2021. This manuscript followed the guidelines of The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) (Von Elm et al., 2007) and the Checklist for Reporting Results of the Internet, list of E-Surveys (CHERRIES) conferences (Eysenbach, 2004).
Ethical aspects
The study was approved by the Ethical Review Board of the Nursing School of the Universidade de São Paulo at Ribeirão Preto, following the ethical guidelines outlined in the 1975 Helsinki Declaration. Additionally, the project was forwarded to the Municipal Health Department of Ribeirão Preto and was approved by Doc. No. 462/2020. Written informed consent was obtained from all participants included in the study after a brief explanation of the study objectives and evaluations.
Sample and data collection
The sample consisted of adults of both sexes with a positive diagnosis of COVID-19. Inclusion criteria were: age≥ 18 years old, positive polymerase chain reaction (PCR) test for COVID-19, living in Ribeirão Preto, state of São Paulo, Brazil. Exclusion criteria were: any immunologically compromised conditions, prolonged use and administration of corticosteroids and/or chemotherapy, transplant recipients, and neurodegenerative diseases.
Sample size
The sample size was calculated a priori using The Power and Sample Size Program®, version 3.043. The selected parameters were a prevalence of COVID-19 hospitalizations of 10.0% with a precision of 3.5% and a confidence interval of 95% for a finite population of 33,643 infected during data collection, reaching a minimum sample of 500 to 650 participants. The Health Secretary of Ribeirão Preto Municipal made available the telephone numbers and personal emails of 33,643 citizens diagnosed with COVID-19. From those, 3,814 telephone contacts were randomly selected using Microsoft Excel®. Seven evaluators made three phone call attempts under the supervision of the main researcher, and 647 participants answered the calls. Data from 14 individuals were disregarded because they did not meet eligibility criteria, and 124 declined to participate. Thus, the final sample size comprises 509 people diagnosed with COVID-19.
Procedures and data collection
Participants answered three questionnaires during the phone calls, and answers were introduced into a Google Forms® data set. All information collected and stored was used without identifying the study participants.
The first questionnaire, "Profile of the person diagnosed with COVID-19" (Ramos et al., 2022), presented questions regarding sociodemographic variables (age, sex, self-reported skin color, education level, and family income), self-reported anthropometric (body weight and height), which was used to derive body mass index (BMI) as weight (m) divided by the square height (m). In addition, this questionnaire also addressed questions to verify the occurrence of COVID-19 signals and symptoms (e.g. fever, headache, muscle pain, difficulty breathing, coughing, loss of taste, loss of smell, stomach upset, diarrhea, nausea, vomiting, chest pain/pressure, coryza, and sore throat), and hospitalization as a consequence of the COVID-19 infection. Finally, this questionnaire was applied by asking the participants to recall the acute moment of COVID-19 infection.
Subsequently, the "Short-Form 6 Dimensions" quality of life questionnaire, a Brazilian-validated version, was applied (Campolina et al., 2011). Participants were questioned about their quality of life before (pre-diagnosis) and after (post-recovery) COVID-19 infection. This questionnaire addresses issues related to functional capacity, global limitation, social aspects, pain, mental health, and vitality. In summary, the key outcomes of this study can be delineated as follows:
Functional Capacity: Quantifies an individual's proficiency in executing daily activities and tasks, reflecting their physical capabilities and overall health status.
Global Limitation: An all-encompassing evaluation of constraints across various life domains, offering a comprehensive perspective on limitations in functionality and participation.
Social Aspects: Relating to the social dimensions of an individual's life, this encompasses interactions, relationships, and societal engagement.
Pain: Refers to the subjective and sensory experience associated with discomfort or suffering, often indicative of underlying physical or psychological issues.
Mental Health: This denotes the state of psychological well-being, spanning emotional, cognitive, and social aspects and providing insights into an individual's mental resilience.
Vitality: This metric gauges energy, vigor, and overall vitality, offering a glimpse into an individual's sense of aliveness and robustness when confronting daily challenges.
The questionnaire was developed on a Likert scale, with the total score ranging from 0 to 6 points. The higher total score represents a better quality of life, considering the issues addressed in the questionnaire.
The Brazilian version of the International Physical Activity Questionnaire - Short Version (IPAQ-SV) (Matsudo et al., 2001) was applied to measure the physical activity level of the week prior to the diagnosis of COVID-19. The IPAQ-SV was applied by asking the participant about the physical activity level in the week before the diagnosis of COVID-19. This instrument assesses the domains and intensity of physical activity, including walking and sitting time, that people perform as part of their everyday lives. The IPAQ-SV conceptualizes the categories as follows: (a) sedentary: does not perform any physical activity for a minimum of 10 continuous minutes during the week; (b) insufficiently active: practices physical activities for a minimum of 10 continuous minutes per week, but not enough to be classified as active. (c) Active: meets the following recommendations: (i) vigorous physical activity: ≥ 3 days/week and ≥ 20 min/session; (ii) moderate activity or walking: ≥ 5 days/week and ≥ 30 min/session; (iii) any added activity: ≥ 5 days/week and ≥ 150 min/week. (d) Very active: meets the following recommendations: (i) vigorous activity: ≥ 5 days/week and ≥ 30 min/session; (ii) vigorous activity: ≥ 3 days/week and ≥ 20 min/session + moderate activity and/or walking ≥ 5 days/week and ≥ 30 min/session. For comparison purposes, in this study, participants were grouped into two groups: sedentary (sedentary and insufficiently active) and active (active and very active) (Ramos et al., 2022).
To ensure that all responses were correctly answered and noted down, the researcher read what was noted down and asked the participant if it was correct.
Statistical analysis
The results were double-checked to reduce possible coding errors and coded by two independent researchers. Non-parametric procedures were adopted because variables were non-normal distributed (after verification using the Kolmogorov-Smirnov test). Results are presented as absolute (n) and relative (%) frequencies for categorical variables. The total quality of life score (quantitative variable) is presented as median and percentiles 25th and 75th. Comparisons between pre-diagnosis and post-recovery and total quality of life scores were performed with the Wilcoxon test for paired samples. To verify the effect size of the impact of the COVID-19 infection on the participants’ quality of life, we adopted Cohen's d (1988) reference values (d< 0.1 = negligible; 0.1≤ d< 0.3 = small; 0.3≤ d< 0.5 = medium; d≥ 0.5= large). The Quade's ANCOVA test (Natarajan et al., 2012) verified the influence of COVID-19 signals, symptoms, and clinical outcomes on the quality of life, controlling for confounding variables age (18 a 59 or ≥ 60 years old), sex (male or female), BMI (≤ 24.9 kg/m2 or ≥ 25 kg/m2), physical activity level (sedentary or active), and family income (≤ $ 370 or ≥ $ 371). The presentation of results and statistical analysis were prepared considering the total sample. All statistical analysis was performed using SPSS® version 20.0 with a significance level of α= 5%.
RESULTS
A total of 509 people were enrolled in this study. Most of the sample were adults (18 to 59 years old), female, overweight or obese, white skin color, and attended high school, received more than $ 371. Regarding physical activity level, similar frequency was found for sedentary and active (Table 1).
Table 1 Study participants’ absolute and relative values of personal and sociodemographic characteristics. Ribeirão Preto, Brazil. 2022.
| Variables | Total Sample (n= 509) | ||
|---|---|---|---|
| n | % | ||
| Age group | 18 to 59 years | 399 | 78.4 |
| ≥ 60 years | 110 | 21.6 | |
| Sex | Male | 198 | 38.9 |
| Female | 311 | 61.1 | |
| Body Mass Index | Up to 24,9 kg/m2 | 144 | 28.3 |
| ≥ 25 kg/m2 | 365 | 71.7 | |
| Skin Color | White | 301 | 59.1 |
| Black | 48 | 9.4 | |
| Asian | 3 | 0.6 | |
| Pardo Brazilian | 156 | 30.6 | |
| Not declared | 1 | 0.2 | |
| Education Level | Illiterate | 3 | 0.6 |
| Elementary Incomplete | 6 | 1.2 | |
| Elementary Complete | 40 | 7.7 | |
| High School – Incomplete | 42 | 8.1 | |
| High School – Complete | 187 | 35.9 | |
| Higher Education – Incomplete | 40 | 7.7 | |
| Higher Education – Complete | 95 | 18.2 | |
| Graduate – Incomplete | 3 | 0.6 | |
| Graduate – Complete | 20 | 3.8 | |
| Family Income* | ≥ $ 371 | 444 | 85.2 |
| Up to $ 370 | 65 | 12.5 | |
| Physical Activity Level | Sedentary | 251 | 49.3 |
| Active | 258 | 50.7 | |
n: frequency number; ≥: greater than or equal to; $: United States Dollar;
*In 2020, the minimum wage in Brazil was $ 202.
Table 2 shows the absolute and relative frequency of responses for each quality of life questionnaire category in the pre-diagnosis and post-recovery of COVID-19 periods. There is a trend toward reducing responses to questions denoting balance in physical and emotional health and increasing the frequency of responses to questions denoting damage and negative impact on health in the pre-diagnosis and post-recovery COVID-19 periods.
Table 2 Absolute and relative frequency of answers to the six Quality of Life questionnaire categories in the pre-diagnosis and post-recovery COVID-19 periods. Ribeirão Preto, 2022.
| Categories | Questions | Total Sample (n= 509) | |||
|---|---|---|---|---|---|
| Pre-diagnosis | Post-recovery | ||||
| n | % | n | % | ||
| 1 - Functional Capacity | Health does not stand in the way of vigorous activity | 405 | 79.6 | 273 | 53.6 |
| Health makes it a little difficult to perform vigorous activities | 61 | 12.0 | 109 | 21.4 | |
| Health makes it a little difficult to perform moderate activities | 23 | 4.5 | 64 | 12.6 | |
| Health makes it very difficult to perform moderate activities | 16 | 3.1 | 54 | 10.6 | |
| Health makes it a little difficult to shower and dress | 2 | 0.4 | 3 | 0.6 | |
| Health makes it very difficult to shower and dress | 2 | 0.4 | 6 | 1.2 | |
| 2 - Global Limitation | I have no problems at work due to physical and emotional health | 451 | 88.6 | 374 | 73.5 |
| I have limitations at work due to physical health | 39 | 7.7 | 92 | 18.1 | |
| I perform less tasks than I would like due to an emotional problem | 13 | 2.6 | 25 | 4.9 | |
| Limited at work due to physical health and I perform fewer tasks due to emotional problems | 6 | 1.2 | 18 | 3.5 | |
| 3 - Social Aspects | Physical health or emotional problems do not interfere with social activities any of the time | 452 | 88.8 | 386 | 75.8 |
| Physical health or emotional problems interfere with social activities a small part of the time | 34 | 6.7 | 44 | 8.6 | |
| Physical health or emotional problems interfere with social activities some of the time | 14 | 2.8 | 45 | 8.8 | |
| Physical health or emotional problems interfere with social activities most of the time | 7 | 1.4 | 27 | 5.3 | |
| Physical health or emotional problems interfere with social activities all the time | 2 | 0.4 | 7 | 1.4 | |
| 4 - Pain | I have no body pain | 374 | 73.5 | 278 | 54.6 |
| I have pain, but it does not interfere with work | 69 | 13.6 | 78 | 15.3 | |
| I have pain and it interferes a little with work | 32 | 6.3 | 55 | 10.8 | |
| I have pain and it moderately interferes with work | 18 | 3.5 | 45 | 8.8 | |
| I have pain and it interferes a lot with work | 15 | 2.9 | 48 | 9.4 | |
| I have pain and it interferes extremely with work | 1 | 0.2 | 5 | 1.0 | |
| 5 - Mental Health | I never feel nervous, anxious or down | 379 | 74.5 | 314 | 61.7 |
| I feel nervous, anxious, or down a little bit of the time | 62 | 12.2 | 65 | 12.8 | |
| I feel nervous, anxious, or down some of the time | 43 | 8.4 | 77 | 15.1 | |
| I feel nervous, anxious, or down most of the time | 22 | 4.3 | 39 | 7.7 | |
| I feel nervous, anxious, or down all the time | 3 | 0.6 | 14 | 2.8 | |
| 6 - Vitality | I feel very energetic all the time | 158 | 31.0 | 100 | 19.6 |
| I feel very energetic most of the time | 265 | 52.1 | 200 | 39.3 | |
| I feel very energetic some of the time | 67 | 13.2 | 129 | 25.3 | |
| I feel very energetic a small part of the time | 18 | 3.5 | 68 | 13.4 | |
| I never feel very energetic | 1 | 0.2 | 12 | 2.4 | |
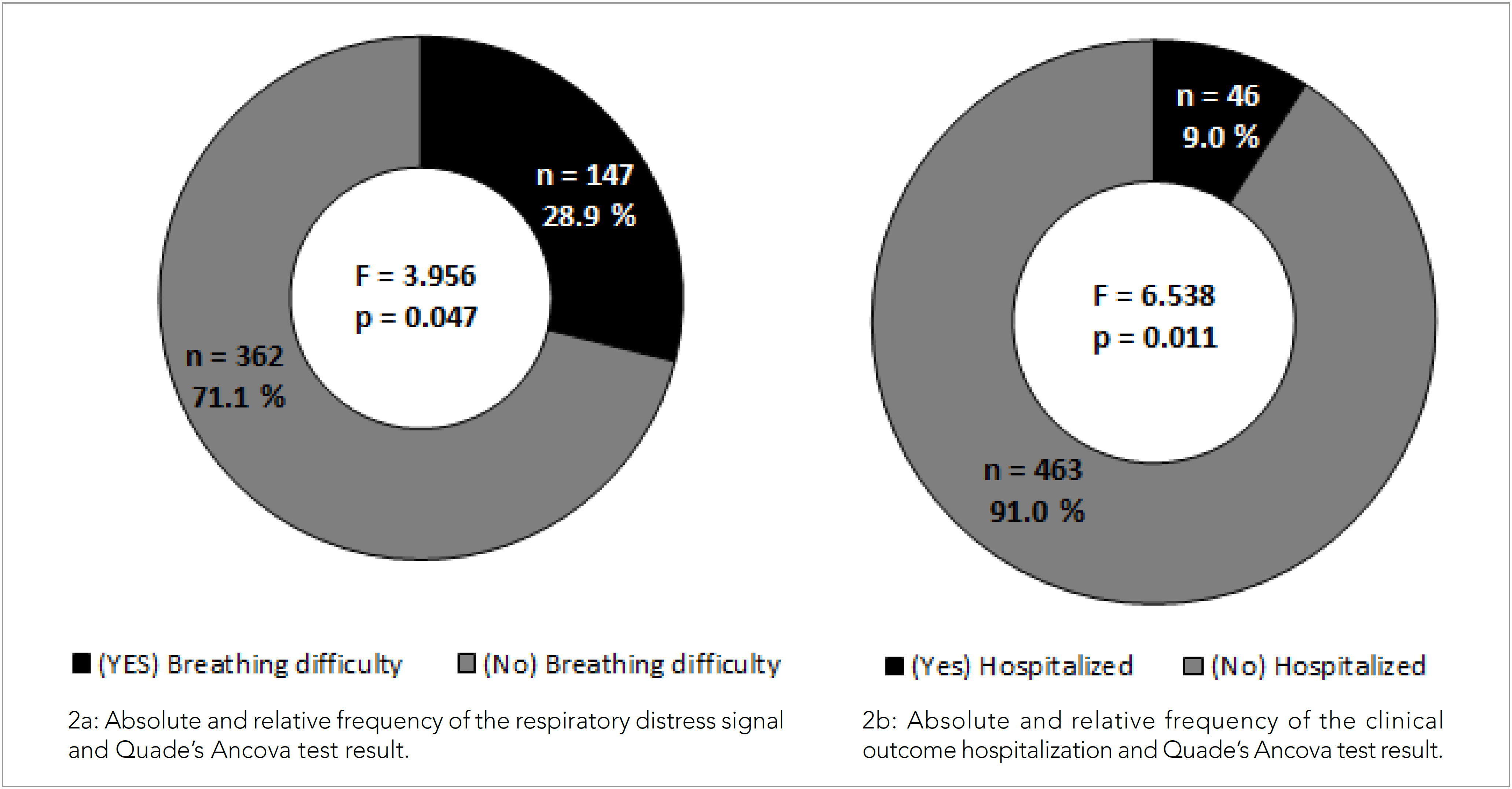
This trend mentioned above is confirmed in Figure 1, where a reduction (2.2 points) in the median value of the total quality of life score was observed in the comparison between the pre-diagnosis (5.6 points) and post-recovery (3.4 points) COVID-19 periods (Z= −19,589; p< 0.001). In addition, the minimum and maximum values (1.0–6.0; 0.0–4.7) and 25th and 75th percentiles (5.0–5.6; 2.5–3.4) were observed in the pre-diagnosis and post-COVID-19 recovery periods, respectively. Additionally, the effect size of the impact of COVID-19 on quality of life was classified as large (d= 0.87).
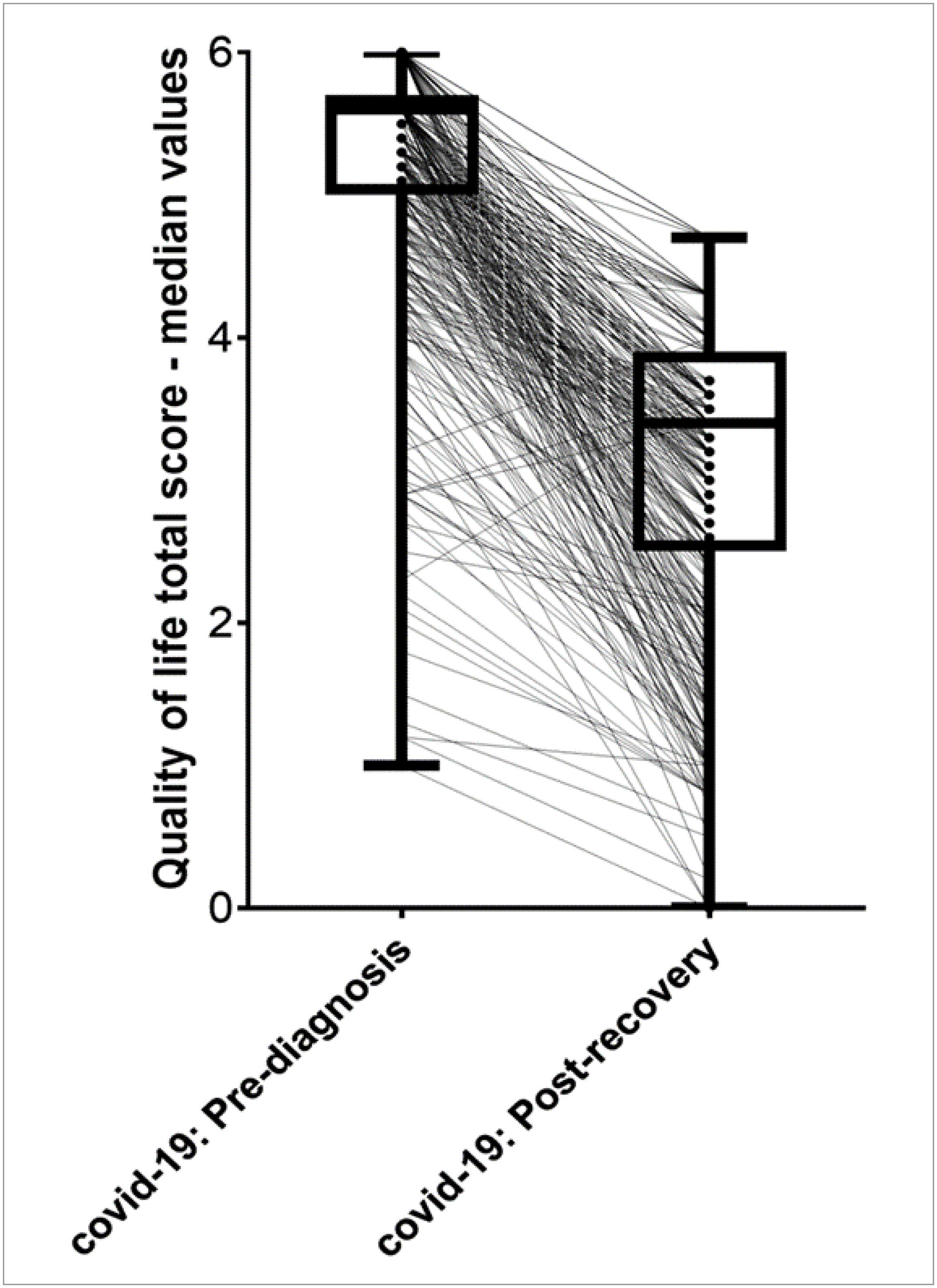
Figure 1 Median values of the total Quality of life score and test of differences in the pre-diagnosis and post-COVID-19 recovery periods. Ribeirão Preto, 2022.
During Quade's ANCOVA test, we verified the influence of COVID-19 signals, symptoms, and clinical outcomes on the quality of life, controlling for age, sex, BMI, physical activity level, and family income. Only signs, symptoms, and clinical outcomes resulting from COVID-19 were presented for those we verified statistical significance. We found that the respiratory distress signal (F= 3,956; [df= 1]; p= 0.047) and the clinical length of hospitalization (≥ 6 days) (F= 6,538; [df= 1]; p= 0.011) had a negative impact on the quality of life of people diagnosed with COVID-19 even after controlling for the variables mentioned above. The absolute and relative frequency of the respiratory distress signal, the clinical outcome of hospitalization, and the result of the Quade's Ancova test of people diagnosed with COVID-19 are present in Figure 2.
DISCUSSION
The study aimed to compare the quality of life on pre-diagnosis and post-recovery of people diagnosed with COVID-19 and examine the impact of its signals, symptoms, and clinical outcomes on quality of life in adults and older adults, considering sex, age groups, nutritional status, physical activity level, and family income as confounding variables. There was a decline in the total quality of life score in the pre-diagnosis and post-COVID-19 recovery periods. Additionally, it was verified that the respiratory distress signal and the clinical length of hospitalization (≥ 6 days) had a negative impact on the quality of life.
In fact, quality of life was impaired with the COVID-19 pandemic, as observed in previous studies (Ferrarello et al., 2023; O’Sullivan et al., 2023). Even after 15 months of recovering from the virus infection, people did not return to their baseline (pre-infection) quality of life (Ferrarello et al., 2023). In addition, people with reduced quality of life had greater severity and prolonged symptoms of COVID-19 infection, besides having a greater likelihood of cardiopulmonary pathogenesis and reduced exercise capacity during submaximal and maximal tests (O’Sullivan et al., 2023). These impacts are speculated to be due to post-acute COVID-19 syndrome, an ongoing symptomatic illness in those recovered from the initial infection by Sars-Cov-2 (Malik et al., 2022). It is suggested that these possible persistent symptoms, such as fatigue, dyspnea, anosmia, sleeping difficulties, chest pain, headache, and cough, may influence the quality of life in post-infection recovery (Malik et al., 2022). In addition, the low quality of life can be explained by the influence exerted on mental health in response to the anxiety generated by the coronavirus pandemic (Ahorsu et al., 2020; Ferreira et al., 2021; Lee, 2020). Therefore, possible speculation of the quality of life impairment of people after recovery is the persistent symptoms after diagnosis of COVID-19.
The number of reduced quality of life responses was visually higher in post-recovery compared to pre-diagnosis for all categories. On the other hand, the number of good responses was visually higher in pre-diagnosis compared to post-recovery for all categories. This indicates the dimensionality of the instrument's items to express the common construct (quality of life) and demonstrates that all items were sensitive to the outbreak. In addition, the number of women was relatively greater than the number of men. This may have occurred due to cultural issues related to sex and the interest in participating in research.
The study's limitations were the reduced sample of the older adult population (n= 112) compared to the adult sample between 18 and 59 years old (n= 397), which could have influenced our findings. However, it is important to highlight that comparisons were age-controlled. Additionally, as it is an observational study, it is not possible to draw inferences about the cause-effect relationship between COVID-19 and quality of life. Also, this study presented a retrospective character; therefore, several factors could influence the response to the questionnaires (i.e. memory, mental status, and illnesses). However, all evaluators were trained to avoid these biases. Finally, our sample refers to a specific group of people, residents of Ribeirão Preto, state of São Paulo, which prevents the results from being expanded to other contexts. The strength of the research was the absence of vaccination bias, as the sample was collected before the population came into contact with the administration of vaccines (January 17, 2021). Furthermore, with the interviews carried out only by the study researchers and not triggered in an electronic form, the sample was always controlled and located in Ribeirão Preto. Another strong point is using the SF-6D Brazil Questionnaire validated in Brazil (Campolina et al., 2011). As this is a telephone survey study, extensive questionnaires could bias the analyses and minimize non-response and withdrawal from the survey (Barriball et al., 1996). Therefore, using a short version questionnaire such as the SF-6D could potentially have reduced possible methodological biases found in more extensive telephone surveys (Silva et al., 2022). The findings of the present study contribute to understanding the quality of life of the population of Ribeirão Preto-SP, considering the impact of COVID-19. This research points out and should serve as an incentive for the search and maintenance of better life habits, for a more active life, and balanced physical and mental health. The prognosis of COVID-19 could be attenuated if more people have possibilities to health care, including access to physical and mental rehabilitation.
The COVID-19 pandemic has negatively impacted every country, some with more chaotic consequences than others. Brazil was one of the countries where the delay in adopting the necessary public health measures to control the pandemic aggravated the spread of the disease (Szwarcwald et al., 2022). Therefore, this study highlights the impairment in the quality of life of individuals after the diagnosis of COVID-19, either due to the association with respiratory distress signal and the clinical length of hospitalization (≥ 6 days) or the coping measures adopted during the pandemic period. For this post-diagnosis scenario to be mitigated, we suggest implementing public policies to encourage the treatment of individuals recovering from COVID-19.
CONCLUSION
COVID-19 infection, especially respiratory distress and hospitalization, negatively impacts the quality of life, even after controlling for age, sex, nutritional status, physical activity level, and family income. Our findings reinforce the importance of proposing treatment strategies for people after a positive diagnosis of COVID-19, including the period after the recovery, to help improve these people's quality of life.