Introduction
Bartholin’s gland cysts and abscesses are the most frequent causes of vulvar masses, with a reported prevalence of 2-3 in 100 women1-5. They account for about 2% of visits to the gynaecologist annually5,6. Its pathophysiology is based on the obstruction of the Bartholin’s gland duct, forming a cyst by the accumulation of fluids1,3. When single or polymicrobial proliferation occurs, most frequently Escherichia coli and Staphylococcus aureus, the obstructed gland gives rise to an abscess1,7,8. Not always abscess are preceded by a cyst, in fact they are three times more frequent than cysts5,9.
Clinical case
We present the case of a 65-year-old woman of Venezuelan nationality, who went to the emergency department of Gynecology with progressive worsening pelvic pain for about two weeks and suspicion of pelvic organ prolapse. As relevant personal history, the patient had a large incisional hernia after gastric bypass surgery, with about 30 years of evolution, morbid obesity (body mass index of 50 Kg/m2), arterial hypertension medicated with losartan and diabetes mellitus controlled and medicated with metformin. About her obstetric and gynaecological history, she was in menopause since 50 years old, had two full-term pregnancies with cesarean delivery and two spontaneous abortions. She wasn’t currently sexually active. According to the her, the last gynaecological evaluation was several years ago.
The patient was hemodynamically stable and apyretic. Genital observation revealed a voluminous right inguino-labial neoformation, approximately 15 centimetres, painful on palpation with inflammatory signs, which obliterated the vagina, which is why the gynecological examination was postponed for a second evaluation (Figure 1). There was also a large incisional abdominal hernia with loss of home with no signs of acute pathology. Blood and urine tests were requested, and analgesic medication was prescribed. Taking into account the findings and considering an inguinal hernia with signs of incarceration as a differential diagnosis, the patient was sent to the general surgery emergency department for evaluation.
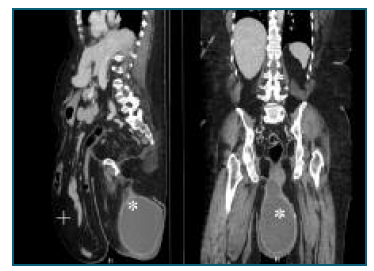
Due to urinary retention, a Foley catheter was placed. Analytical evaluation showed leukocytosis (12000 leukocytes/uL) and a C-reactive protein of 227 mg/L. After the objective examination, an abdominal and pelvic radiography was requested, with no relevant changes and, later, an abdominal and pelvic computed axial tomography (CT scan). CT scan described a cystic formation in the area of the right labia majora measuring about 135x165x213 millimetres, corresponding to a volume of about 2500 cc, compatible with a Bartholin’s gland abcess (Figure 2). After these findings, the patient returned to the emergency department of Gynecology.
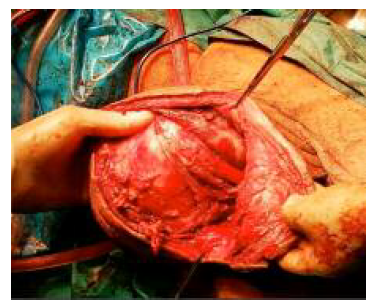
After discussing the case in a multidisciplinary team, the excision of the Bartholin’s gland under general anesthesia was proposed, which the patient accepted. An elliptical incision was then made over the mass, with blunt debridement of the cyst capsule, during which accidental rupture was observed, with drainage of about 1500 cc of purulent content, which was sent to microbiological study. After this, removal of the entire cyst capsule, excision of redundant tissue, review of haemostasis and closure of the surgical wound by layers was made, with a multifilament synthetic absorbable interrupted suture (Vycril ® ), size 0 for the deep layer, a size 2-0 for the skin (Figure 3). The patient remained with a Foley catheter and a Blake 19 catheter in the surgical site (Figure 4). The gynaecological examination showed no other relevant changes.
Intravenous broad-spectrum antibiotic therapy, piperacillin and tazobactam, was prescribed for ten days, and low molecular weight heparin during the entire hospital stay, for thromboembolism prophylaxis. During hospitalization hygiene care of the surgical wound was made with povidone-iodine foam. As intercurrences during hospitalization, she had a poor glycemic control, requiring medication adjustment, and an iron deficiency anemia (haemoglobin 8.7 g/dL), medicated with intravenous iron carboxymaltose. On the fourth postoperative day, she presented spontaneous externalization of the Blake 19 catheter, at which time draining was less than 50 cc of serohematic fluid in 24 hours. The microbiological study of the collected material was positive for anaerobic gram positive cocci and negative for aerobic bacteria.
On the tenth postoperative day, a small pearly area was observed in the middle third of the wound, measuring approximately 10x5 millimetres. Superficial surgical debridement was performed, less than five mm in depth. Due to the good evolution of the surgical wound, and clinical and hemodynamic stability, discharge was decided on the 14th day of hospitalization. Was recommended to keep the surgical wound washed with povidone-iodine and hygiene precautions to be taken were explained. The patient was reassessed two weeks and one month after surgery, with good evolution (Figure 5). She was referred for a general surgery appointment to follow up the incisional hernia, to the family doctor for follow-up of the remaining comorbidities and to the nutritionist.
The anatomopathological study identified a ruptured cavity formation with about 19.5x14.5 centimetres in greatest dimension. The microscopic study identified an epithelial cyst of non-keratinizing squamous epithelium with inflammatory infiltrate and ulceration of the lining, fibrohyaline wall with signs of activity, without signs of malignancy, compatible with the clinical diagnosis of Bartholin’s gland cyst with inflammatory signs.
Two months after the operation, the scar presented with the edges well coapted, with good healing, without inflammatory signs. Although she has limitations, taking into account her incisional hernia and obesity, the patient reports a significant improvement in her quality of life after the resolution of this acute episode.
Discussion
The differential diagnosis of vulvar masses includes Bartholin’s gland cysts and abscesses, inclusion cysts, Gardner’s duct cysts, lipomas, inguinal hernias, sebaceous cysts, and in rare cases, vulvar carcinoma and Bartholin’s gland carcinoma1,2,10. Bartholin’s glands are important for vulvar and vaginal lubrication through the production of mucus, which they release through their ducts that open into the vulvar vestibule1,11. As already mentioned, when they become obstructed, they can lead to the appearance of cysts or abscesses, if proliferation of microorganisms occurs inside, usually opportunistic bacteria1,2,5,8.
These are frequent reasons for visiting health care facilities since in most cases severe pain and vulvar tumefaction are the presenting symptoms, which interferes with the quality of life1,3. Dimensions usually vary between one and three centimetres, being Bartholin’s gland abscesses larger than ten centimetres very rare and few cases are described in the literature, hence the relevance of this case2,9,10. Although the patient reports symptoms with two weeks of evolution, and taking into account the patient’s biotope, there is doubt if the growth to these dimensions was fast or slow, having become painful after microbial colonization and Bartholin’s abscess formation.
The management of Bartholin’s gland cysts/abscesses depends on the size, symptoms, age, and history of recurrence, but there isn’t consensus about the best approach, since evidence for preferring one treatment over another is lacking1,3,5. Usually in small symptomatic cysts, smaller than three centimetres, the recommended approach is expectant management, with warm compresses, sitz baths and analgesics for pain control. If a small abscess is suspected, incision and drainage is the usual approach, with associated pain relief measures3,4,5. Although some authors prescribe antibiotic therapy in all Bartholin’s gland abscesses, with coverage for the main pathological microorganisms, others reserve antibiotic therapy for recurrences or high risk for a complicated infection, such as exuberant inflammatory signs, pregnancy, among others3,8.
Bartholin’s gland abscesses larger than three centimetres, the most frequent approach is incision and drainage with placement of a Wood catheter or marsupialization, associated with antibiotic therapy1,2,3,4. The two approaches appear to be equally effective and have similar recurrence rates, so, some authors prefer Wood Catheter as a first approach, since is easier to perform, and marsupialization if there is a recurrence. The definitive treatment is excision of the gland, a more invasive procedure, so is recommended for recurrences that are refractory to the other approaches3,5,6. Other approaches such as silver nitrate sclerotherapy and alcohol sclerotherapy, are also described, apparently with good results, but more randomized trials are needed to compare the different approaches3.
In this case, given the patient’s dimensions and risk factors, excision of the Bartholin’s gland associated with broad-spectrum antibiotic therapy was decided, in order to reduce the likelihood of recurrence and the risk of infection. A similar approach was taken in the other case reports2,9,10. Also, it’s important to mention that patient age alters the approach, as some authors argue that above 40 years of age, a biopsy should be performed in order to exclude primary carcinoma of the Bartholin’s gland, which, although rare, corresponds to 0.1 to 5% of all vulvar carcinomas5.
Once again, the relevance of this case isn’t due to the rarity of Bartholin’s gland abscesses, but due to the dimensions in which this case presented itself. Therefore, the case description is interesting, because of the pathology itself, but also because of the therapeutic approach and the results obtained.
Authors’ contribution
Carlos Macedo: Conceptualization, Writing - original draft, Writing - review & editing
Rita Gomes: Writing - review & editing
Sara Camara: Writing - review & editing, Resources
Marta Ledo: Writing - review & editing, Resources
Susana Nóbrega : Writing - review & editing, Resources