Introduction
Pregnancy is a completely new and different period in a woman’s life leading to physical and psychological changes. Physiological changes occur in pregnancy to nurture the developing fetus and prepare the mother for labor and delivery. These changes begin after conception and affect virtually every organ in the body1.
At a psychological and relational level, pregnancy is a process of adapting to the new parental role, leading to changes in the woman’s perception of herself. With regard to heterosexual conjugality, it is known that the couple, who until then constituted only as a man and a woman, become, through parenting, the constitution of father and mother - which comes to change profoundly their individual dynamics and the marital relationship2-4. These physical and psychological arguments are further complicated by the fear of hurting the fetus during sexual intercourse or by induction of premature birth - the two most common grounds of abstinence from sexual intercourse during pregnancy4-5.
Pregnancy and postpartum-period represent a critical phase for the onset or worsening of sexual problems, as desire, interest and sexual activity tend to decrease during this period causing suffering for the pregnant woman and her partner4-109.
The main goals of our study were to evaluate the general knowledge of our population regarding the possible complications arising from sexual intercourse during pregnancy, to evaluate the impact of pregnancy on the couple’s sexuality, to evaluate the factors that may condition this impact and to assess the influence of sexuality on obstetric outcomes.
Materials and Methods
The observational, cross-sectional and descriptive study was conducted between March 2021- April 2022. Data were collected through a structured questionnaire administered to women hospitalized in the Obstetrics service of Unidade Local de Saúde do Alto Minho (ULSAM). The questionnaire was distributed and filled out within the first 48 hours after delivery. The collected data encompassed the epidemiological characterization of participants, including age, education, parity, contraception, and sexuality before pregnancy. Specific questions were posed to assess changes in sexual experiences during pregnancy, participants’ knowledge about the possible impact of sexual intercourse on a healthy pregnancy or pregnancy complications, and the sources of such information. Additionally, information was gathered regarding obstetric complications, mode of delivery, and newborn weight (Adnexa 1).
Approximately 6 months after delivery, a follow-up phone questionnaire was done to evaluate the resumption of sexual intercourse and identify any main difficulties encountered.
All data collected were entered into a database using the Statistical Package for the Social Sciences (SPSS) software, which was also employed for statistical analysis. Statistical significance was assumed for p-values <0.05, with a confidence interval of 95%.
Results
Our sample includes 97 women. The age range was 21 to 43 years, mean of 32.3 years (Standard Deviation SD 5.1). In respect of level of education: 36.7% have academic education; 51% have secondary education and only 7% have primary education. The majority of participants (79%) were employed.
Regarding the gynecological history, half of the women were primiparous. Additionally, approximately 31% of the participants reported having experienced at least one previous abortion, highlighting the relevance of reproductive health experiences in the study population.
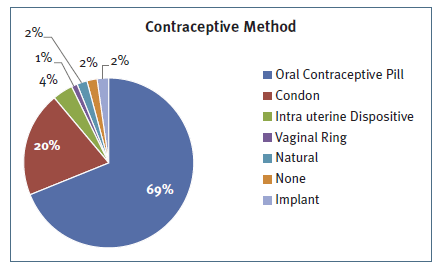
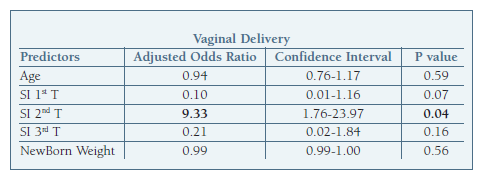
The most used contraceptive method previous to pregnancy was the oral contraceptive followed by the male condom (Figure 1).
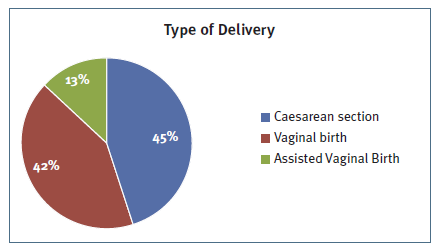
58% of the participants had a vaginal delivery (Figure 2) and the majority of women, 80%, had a term delivery (>37 weeks of gestation).
Four women reported suspension of sexual intercourse once pregnancy was confirmed, with three of them expressing concerns about potential harm to the baby.
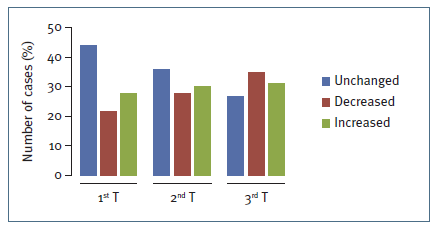
During the first trimester, approximately 44% of participants reported that their sexual desire remained unchanged. However, as pregnancy progressed into the second and third trimesters, a significant shift in sexual desire was observed. Specifically, 58% of women revealed changes in sexual desire during the second trimester, with 30% experiencing an increase and 28% a decrease. The third trimester demonstrated the most pronounced decline in sexual desire, with 35% of responders reporting diminished interest. (Figure 3)
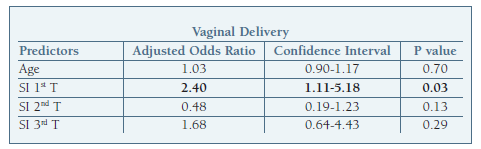
Using the paired-samples T test, we can conclude that in relation to the frequency of sexual activity, there is a statistically significant decrease in all trimesters and in post-partum compared to the frequency of sexual intercourse (SI) prior to pregnancy (M = 2.41 SD = 1.05). The most marked decrease was in the third trimester (M = 1.51 SD = 1.05) p <0.001 (Table I). Interestingly, a history of previous miscarriage did not have a significant impact on the frequency of sexual activity during any trimester of pregnancy.
Table I Frequency of sexual intercourse per week prior to pregnancy, first, second and third trimesters and post-partum.
On average, vaginal penetration was suspended at 34-35 weeks of gestation.
57% of respondents stated that the main source of information related to sexuality during pregnancy were health professionals and 33% the internet. 19% admitted that they had little openness with their doctor to discuss issues related to this topic.
Only one woman revealed to be dissatisfied with her sex life during pregnancy, because she wanted to have more sex drive.
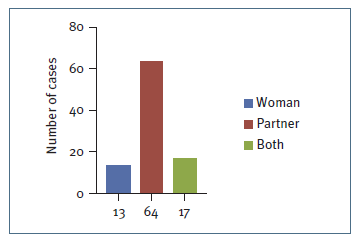
In 64% of cases it is the partner who shows more initiative for SI (Figure 4).
None of the respondents think that their partner’s sexual desire increased during pregnancy, with 19% saying it decreased either due to physical changes or fear of harming the fetus.
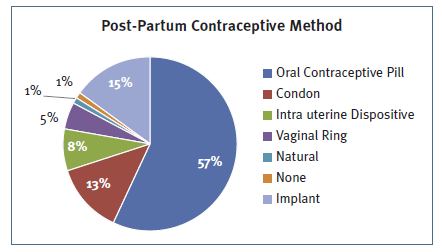
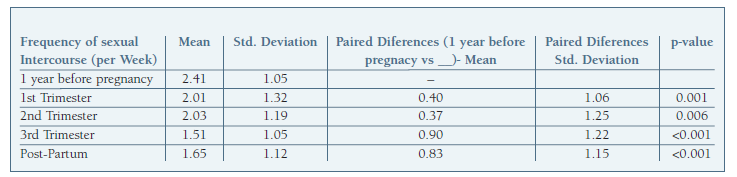
There is a significant association between the frequency of SI per week in the 2nd trimester and the type of delivery. Women who had a vaginal delivery had an average of 2.16 SI per week (SD 1.28) compared to 1.78 SI per week in the caesarian group (SD 1.05) p = 0.04. Using binary logistic regression, the frequency of SI per week in the 2nd trimester continues to be associated with a higher probability of vaginal delivery about 9 times higher (OR 9.33, CI 1.76- 23.97, p = 0.04) (Table II). This difference does not occur in either first or third trimester. In the other hand, there is a significant association between the frequency of SI per week in the 1st trimester and the risk of pre-term delivery (OR 2.40, CI 1.11- 5.18, p = 0.03) (Table III).
On average sexual intercourse is resumed 10 weeks after delivery. The type of delivery (vaginal or cesarean) does not influence the time of resumption of intercourse but on the other hand appears to influence the frequency of sexual intercourse. At 6 months post-partum the frequency of SI per week in the cesarean delivery group was 2.2 (SD 1.3) SI per week compared to 1.3 (SD 0.9) SI per week in the vaginal delivery group, with statistic significance p=0.02.
For most women, post gestational sexuality is at first problematic. Only 25% of the women report having no sexual problems postpartum. The main problems reported in our study were dyspareunia (41%), loss of sexual desire (25%) and vaginal dryness (9%).
Six months post-partum the contraceptive method of election remains the oral contraceptive pill, but more women decided to use long acting contraceptives (Figure 5).
Discussion
Our results are in general consistent with the literature. In our population perception of female sexual interest in the majority of women is unchanged in the first trimester, and decreases in the third trimester. In the 2nd trimester it is variable. Also in the literature4,6,8 female sexual desire in pregnancy is unchanged or slightly decreased in the first trimester and decreases sharply at the end of the third trimester, but altogether it is remarkably variable, especially in the second trimester.
Several studies have suggested a relationship between the woman’s age and sexual desire and frequency of SI during pregnancy6-7. Although we didn´t find any correlation between the sexual desire and activity and the woman’s age. In some papers, an association between previous abortions and frequency of SI is mentioned7, but this was not proven in our sample.
In the majority of couples the men show more sexual initiative before, during, and after pregnancy than the women6,9. This is consistent with our paper that in 64% of cases is the partner who shows more initiative for SI.
In our study there is a statistically significant decline in the frequency of sexual activity per week in all trimesters and post-partum, particularly in the third. Sydow et al6 concluded that coital activity decreases slightly in the first trimester or remains constant, declines sharply in the third trimester and is reduced in most couples 1 year after birth. Several other studies have shown a progressive decrease in frequency of sexual activity throughout pregnancy3-4,7-8,9.
In ULSAM the mean gestational age of last coitus was 34 weeks of gestation similar to what the literature reports, about 1 month before delivery6. Our study showed a lower percentage of sexual abstinence (4.1%) compared to (10%) in Sydow et al6.
In the majority of studies including a 2007 Portuguese investigation7 continued sexual activity did not correlate with the risk of small for gestational age or pre-term delivery. However in our sample, the frequency of sexual intercourse in the first trimester is significantly associated with pre-term delivery.
Health professionals played a crucial role as a source of information related to sexuality during pregnancy, as reported by 57% of respondents in our study. The percentage is somewhat higher than that in other studies (21-29%)7,9, suggesting that healthcare providers play a significant role in addressing sexual health concerns during pregnancy3. Sydow et al. reported that 68% of young mothers did not recall their gynecologists discussing sexuality during pregnancy6.
An interesting finding is the association between the frequency of SI during the 2nd trimester and the likelihood of a vaginal delivery (OR 9.33, CI 1.76- 23.97, p = 0.04). This result suggests a potential link between sexual activity and the mode of delivery.
Regarding post gestational sexuality, our study found that resumption of intercourse occurred, on average, at 10 weeks postpartum, which is longer than the average in Europe and the USA (between six and eight weeks). Additionally, most women (75%) reported experiencing difficulties, consistent with literature where postpartum sexual problems are common. In Sydow et al6 only 14% of the women and 12% of the men report having no sexual problems postpartum.
Dyspareunia emerged as the major problem reported by women in our sample, which is consistent with findings from other studies8.
The choice of the contraceptive method is also interesting pre and post pregnancy. The oral contraceptive pill was the preferred method both before and after pregnancy, with a slight decrease in the post-partum (pre: 69% post: 57%). The main difference is that women after pregnancy favored longer-duration contraceptives, for example: previous pregnancy only 2% used subcutaneous implant and 4% intra-uterine device comparing to 15% and 8% after pregnancy, respectively. Condom usage also decreased in the post-partum period (pre: 20%, post 13%).
Conclusion
Most studies report a progressive decline in the frequency sexual activity and sexual desire throughout pregnancy, with a sharply decrease in the third trimester.
While more than half of the respondents in our study relied on health professionals as their primary source of information for sexual issues during pregnancy, it is concerning that 16% admitted to having limited openness with their doctors in discussing their doubts. To promote the psychological and physical well-being of pregnant women and couples, it is crucial for healthcare professionals in the perinatal field to engage in open and supportive discussions about sexual health. Healthcare professionals can assist by offering greater education and support to pregnant couples and new parents regarding sexuality, and adequately informing them about the common fluctuations in sexual activity, interest, desire, and responsiveness over the course of the pregnancy and following childbirthd.
We acknowledge some limitations of our study. First we used a questionnaire that is not validated. Second we focused on a limited time period which may not truly represent the entire pregnancy. Finally, there is a limitation of the retrospective nature of data collection.
Nevertheless, we were able to associate important aspects of sexuality during pregnancy. Our study reveals an interesting association between the number of weekly sexual intercourse (SI) during the second trimester and the likelihood of a vaginal delivery. For each increase in the frequency of SI in the second trimester, there is a nine-fold greater probability of a vaginal delivery, with no significant difference in the risk of preterm delivery. However, in the first trimester, for each increase in the number of weekly SI, there is a two-fold greater probability of preterm delivery.
These interesting results suggest that sexual activity during pregnancy might have implications for the mode and timing of delivery, but further investigations with larger participant cohorts are needed to establish more statistically robust conclusions.
In conclusion, our study contributes valuable insights into the sexual experiences of pregnant women and the importance of addressing sexual concerns during pregnancy. The findings emphasize the crucial role of health professionals in offering support and guidance, ultimately promoting the overall well-being of expectant women and couples.
Declaration of interest statement
The authors have no financial interests or benefits associated with the prepared research.
Author contributions
All authors contributed to the concept and study design. SPS, AMM, MRT and LCS contributed to analysis and interpretation of data. SPS was responsible for the article draft. SC, FD and PP supervised the team research and revised the article critically. All authors approved the final article as submitted and agreed to be accountable for all aspects of the work.