Introduction
Surgical residency is a challenging time in the life of a physician. The need to provide adequate training without compromising patient care is a fine balance between risk and responsibility, especially when dealing with complex specialties like Vascular Surgery, where most procedures are life or limb-threatening. For this reason, Vascular Surgery residency programs must be able to provide access to a wide range of patients, procedures and technology and, in order to achieve excellent patient care, training is demanding. Moreover, with current technological advances and scientific progress, most surgeons need to be proficient in understanding and following scientific research and ideally, also engage in scientific work. Therefore, most training programs now demand not only demonstration of clinical and surgical skills but also academic and scientific training.1 All of this leads to highly complex schedule where the resident must balance the demanding requirements of the residency program, with his own personal life regarding family commitments, hobbies and outside interests. An inability to achieve a correct balance has led to high degrees of stress, burnout and ultimately inability to adequately complete the residency programs.2,3 Furthermore, with the current advances in Vascular Surgery and sub specialization, it is difficult for any Department to provide adequate training in all areas of Vascular Surgery.
Our aim was to understand the current satisfaction rates regarding the Vascular Surgery residency program in Portugal and comprehend the current limitations and areas to improve. Therefore, we conducted a National Survey study targeting Vascular Surgery residents in Portugal to answer these questions.
Methods
A survey study was conducted between April and June 2021 targeting Angiology and Vascular Surgery Residents in Portugal. Residents were contacted by e-mail from the National Portuguese Society of Angiology and Vascular Surgery (SPACV) to answer the survey. The survey was anonymized, and all residents from the 1st to 6th year of residency were invited to participate. During this period, two e-mails were sent with one-month interval and additional personal contacts were made to promote enrollment. There were no age, nationality or sex restrictions regarding participation, with the only requirement being enrolled as a resident in an Angiology and Vascular Surgery Program in Portugal.
Currently, in Portugal, the residency program comprises both Angiology and Vascular Surgery specialties and is a 6-year training program. The program consists of 56 months of Angiology and Vascular Surgery (with the possibility to enroll in a Fellowship in another institution for up to 6 months), 12 months of General Surgery training (usually performed in the first year); 2 months of Intensive Medicine training and 2 months of Cardio-thoracic Surgery training. Each year residents are evaluated in their departments and in the final year they must finish their certification by passing a National Board Exam. Since the survey was completely anonymized, with no way to trace back the answers to the participants, no ethical approval was requested.
The survey was carried out using the Google® Forms platform and using Portuguese language. The concept and design of the survey was developed by the SPACV (Sociedade Portuguesa de Angiologia e Cirurgia Vascular), more specifically by the Resident and Academic Committees of the Society. Questions were developed with two main objectives, the first being to analyze the satisfaction rates with the current residency program and the second to understand current limitations and possible areas that would be optimal to provide/have access to more training.
Table 1 Survey answers regarding the Residency Program, focusing on training limitations.
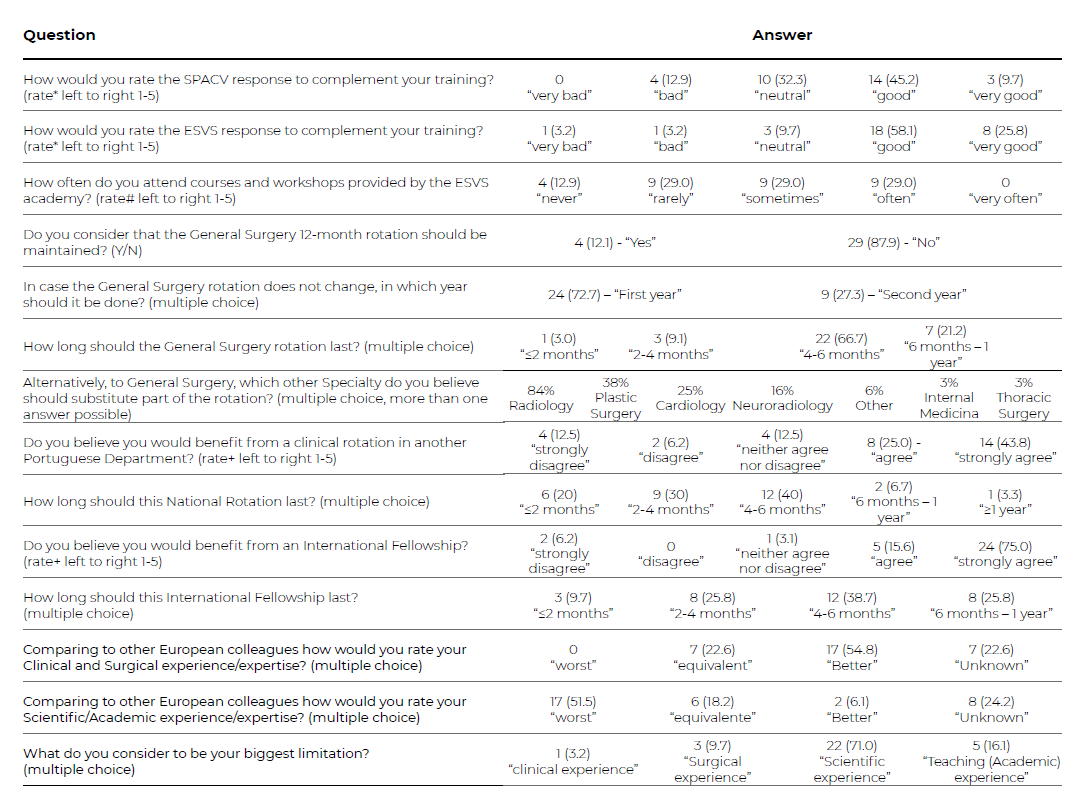
*Rating answers: 1 - “very bad”; 2- “bad”; 3 - “neutral”; 4 - “good” and 5- “very good”.
# Rating answers: 1 - “never”; 2- “rarely”; 3 - “sometimes”; 4 - “often” and 5- “very often”.
+ Rating answers: 1 - “strongly disagree”; 2- “disagree”; 3 - “neither agree nor disagree”; 4 - “agree” and 5- “strongly agree”. Abbreviations: Y-Yes; N-No; SPACV- Sociedade Portuguesa de Angiologia e Ciurgia Vascular (Portuguese Society of Angiology and Vascular Surgery); ESVS - European Society of Vascular Surgery.
Table 2 Survey answers regarding the Residency Program, focusing on personal satisfaction.
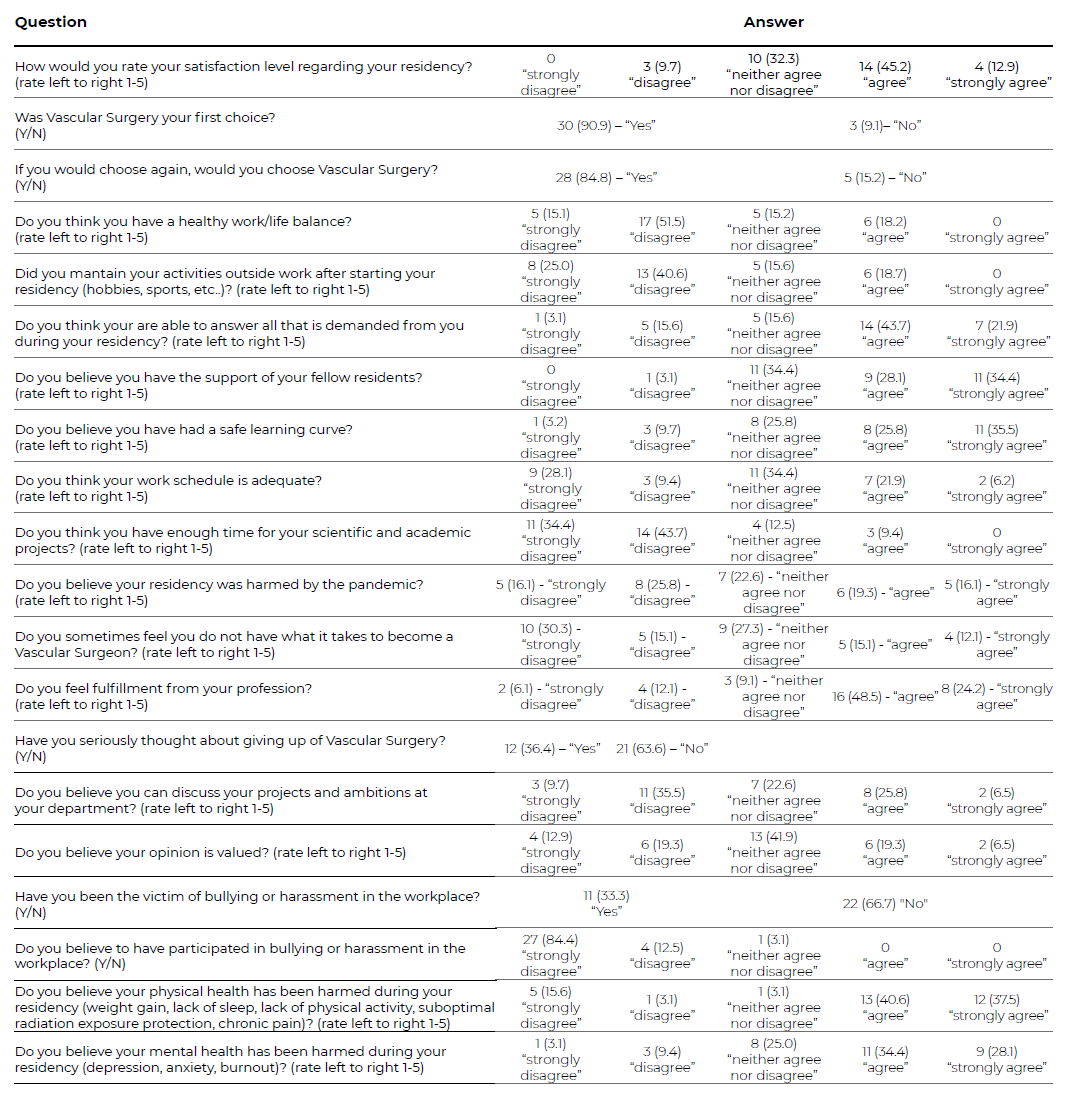
Abbreviations: Y-Yes; N-No;
All specific questions of the survey are detailed in supplementary data 1. Regarding the residency program and perceived training limitations, residents were queried on the availability of training resources; organization of the residency program; clinical, surgical and scientific experience; competitiveness of their experience compared to other European countries; experienced surgical training limitations and experienced scientific and academic training limitations. Regarding personal satisfaction with the residency program, residents were queried on overall satisfaction rates; work/life balance; peer support; personal insecurities regarding training; adequacy of work schedules and demands; fulfillment; burnout; bullying or harassment at work and physical and mental health.
Questions were multiple choice options, “Yes” or “No”, or asked to rank using a Likert-type scale ranging from 1to5, being 1 the lowest (worse) rank to 5 the highest (best) rank - supplement data 1. For comparison between younger and older residents, two groups were created: 1-3 years of residency vs 4-6 years of residency.
Statistical analysis was performed using STATA software, version 16.1 (StataCorp, 4905 Lakeway Dr, College Station, TX 77845, USA), for Mac. Continuous variables are presented as median (interquartile range). Categorical variables were presented as frequency (percentage). Mann-Whitney test was used when comparing continuous variables and Chi2 or Fisher’s exact test to compare categorical variables. All analyses were considered statistically significant if a two-tailed p-value < 0.05 was observed. For analysis purposes younger residents (year 1-3) were compared to older residents (year 4-6).
Results
Overall, 33 out of 51 invited residents participated in the survey (response rate of 65%). Out of the 33 residents, 5 (15%) residents were in the 1st year, 4 (12%) in the 2nd, 5 (15%) in the 3rd, 6 (18%) in the 4th, 6 (18%) in the 5th and 7 (21%) in the 6th. Nineteen residents were male (58%).
The survey results are detailed in Tables 1 and 2 and Figures 1-6.
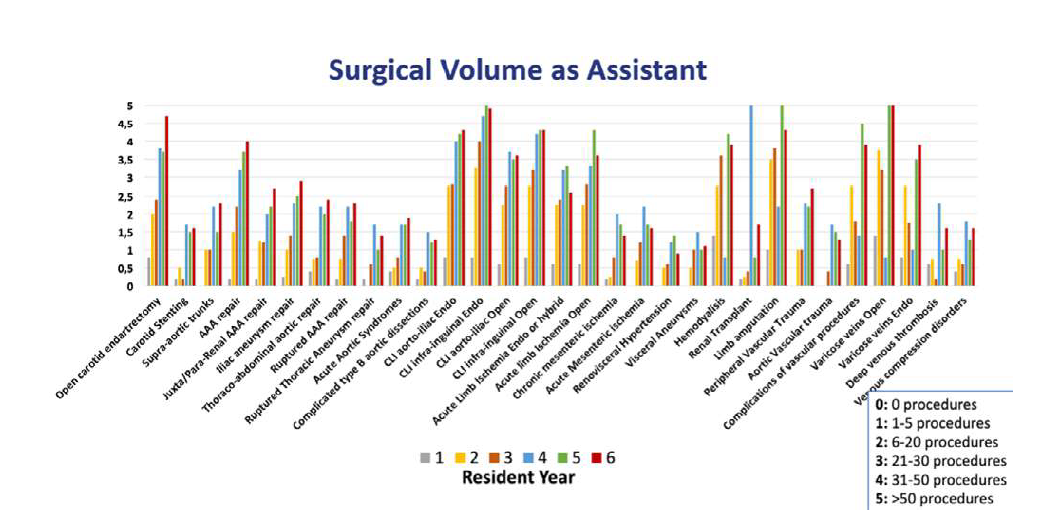
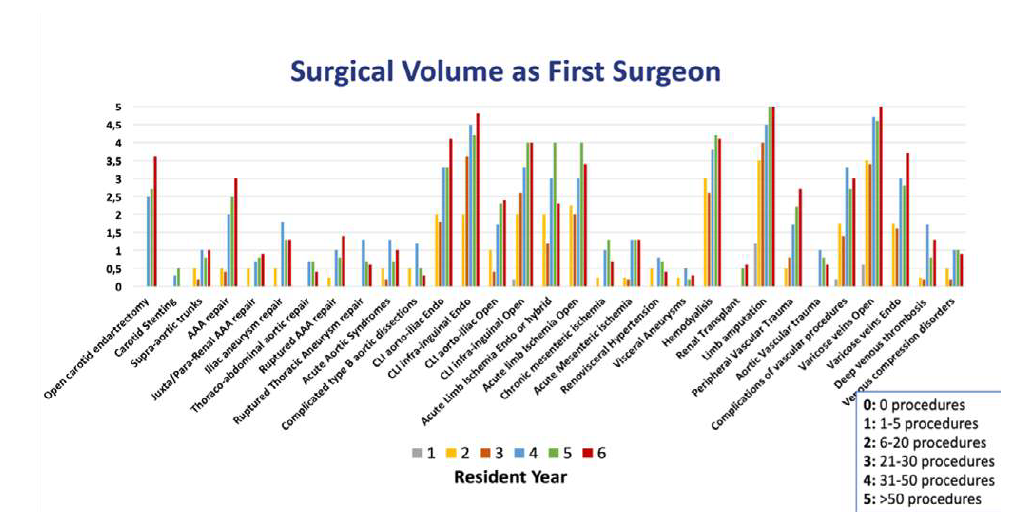
Regarding surgical experience as an assistant and first surgeon a tendency towards growing experience in the more advanced residency years is seen as expected (Figure 1 and 2)
Y axis is ranked from 0-5 (0: no surgeries; 1; 1-5 procedures; 2; 6-20 procedures; 3: 21-30 procedures; 4: 31-50 procedures; 5: > 50 procedures). Each column represents each individual year by surgery group.
Y axis is ranked from 0-5 (0: no surgeries; 1; 1-5 procedures; 2; 6-20 procedures; 3: 21-30 procedures; 4: 31-50 procedures; 5: > 50 procedures). Each column represents each individual year by surgery group.
Regarding the technique of revascularization of the lower limbs, especially regarding aorto-iliac revascularizations there is a higher current experience with endovascular repair compared to open. Exceptions to this are seen in the carotid surgery area and acute limb ischemia, where open repair is still more prevalent. Most of the residents felt that their surgical and clinical experience was equivalent (23%) or better (55%) when compared to other European colleagues.
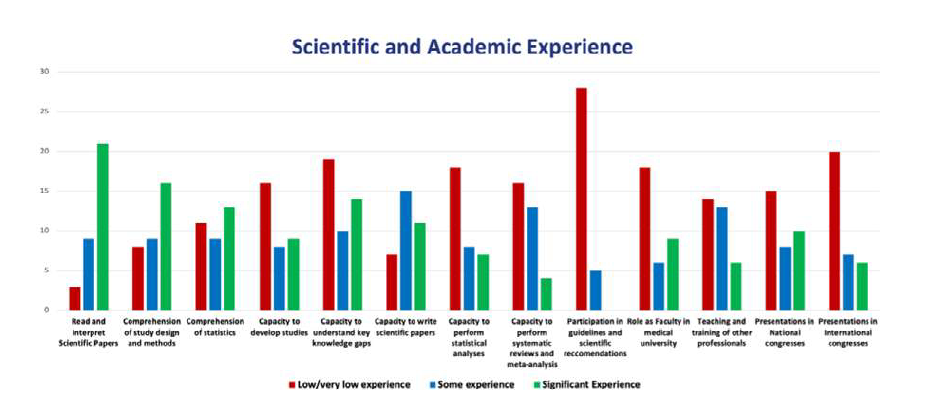
Regarding scientific and academic experience, main limitations/lack of experience were reported in participation in guidelines/scientific recommendations, presentations in international meetings, teaching and training of other professionals, ability to perform statistical analysis and systematic review and meta-analysis (Figure 3).
Y axis is representing the number of answers. Possible answers were: Low/very low experience; Some experience or Significant experience.
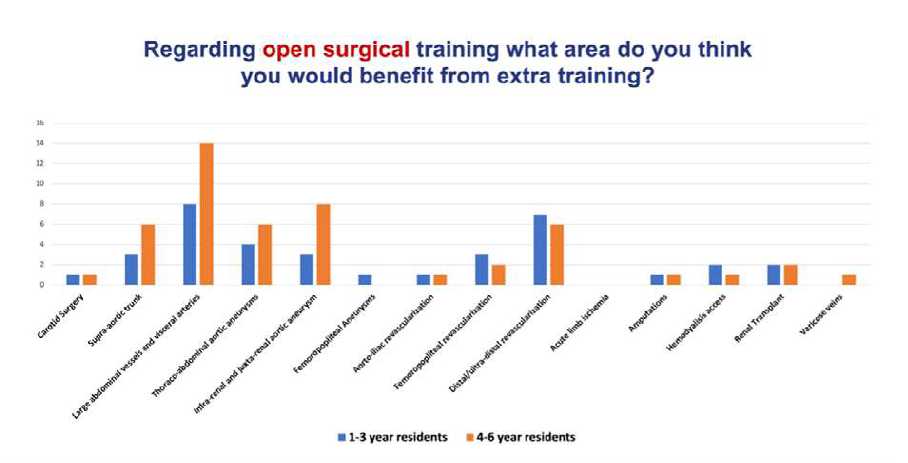
When asked where additional open surgical training would be beneficial, most residents answered large abdominal vessels and visceral arteries, infra-renal and juxta-renal abdominal aortic aneurysms (AAA) and distal/ultradistal revascularization (Figure 4).
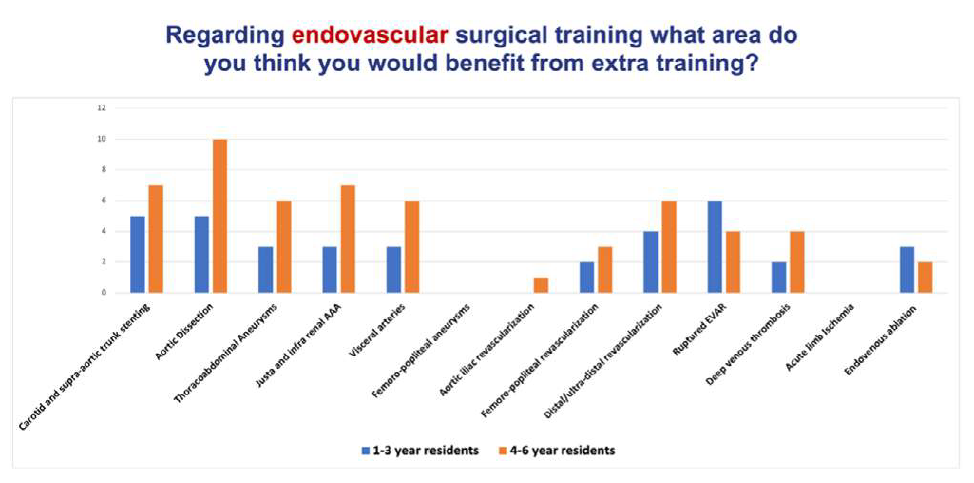
Regarding endovascular surgery, most residents answered aortic dissection, carotid and supra-aortic stenting and ruptured AAA (Figure 5).
Y axis is representing the number of answers. Possible answers were 3 out of all represented in the x axis. Younger residents are represented in blue and older residents in orange.
Y axis is representing the number of answers. Possible answers were 3 out of all represented in the x axis. Younger residents are represented in blue and older residents in orange.
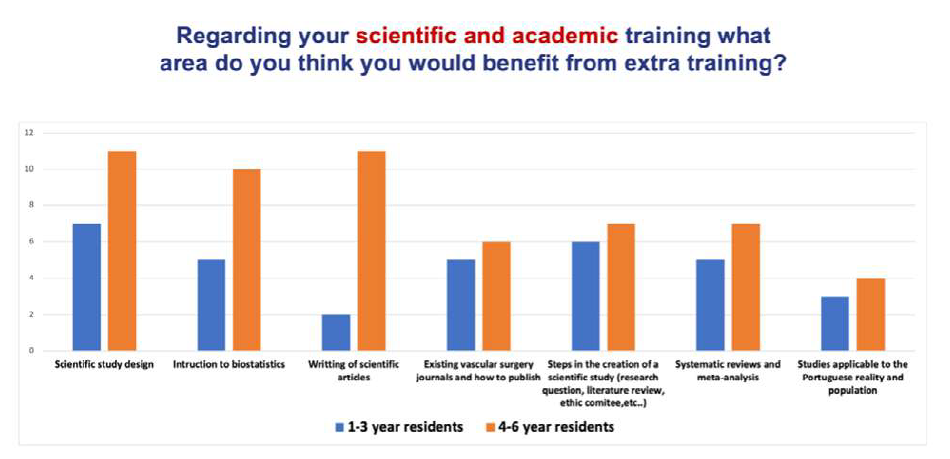
When asked where additional scientific and academic training, older residents (4-6 years) answered scientific study design, statistics and writing of scientific papers, while younger residents answered scientific study design and steps in the creation of scientific studies (eg. development of a research question, literature review, dealing with ethic committees), Figure 6.
Y axis is representing the number of answers. Possible answers were 3 out of all represented in the x axis. Younger residents are represented in blue and older residents in orange.
When comparing the survey answers between younger and older residents, no significant differences were observed in most answers - (Table 3).
However, differences were found regarding the opinion of surgical/clinical experience compared to other European colleagues, with older residents considering having a better experience (79% versus 17%, p=0.004), while, regarding scientific experience, older residents considered having worse expertise (68% versus 29%, p=00.18).
Additionally, when asked if the resident has ever contemplated quitting the residency program or if he has been victim of bullying or harassment, older residents answered “yes” more often than younger residents (53% versus 14%, p=0.024 and 47% versus 14%, p=0.046, respectively).
Table 3 Comparing younger residents to older residents survey responses.
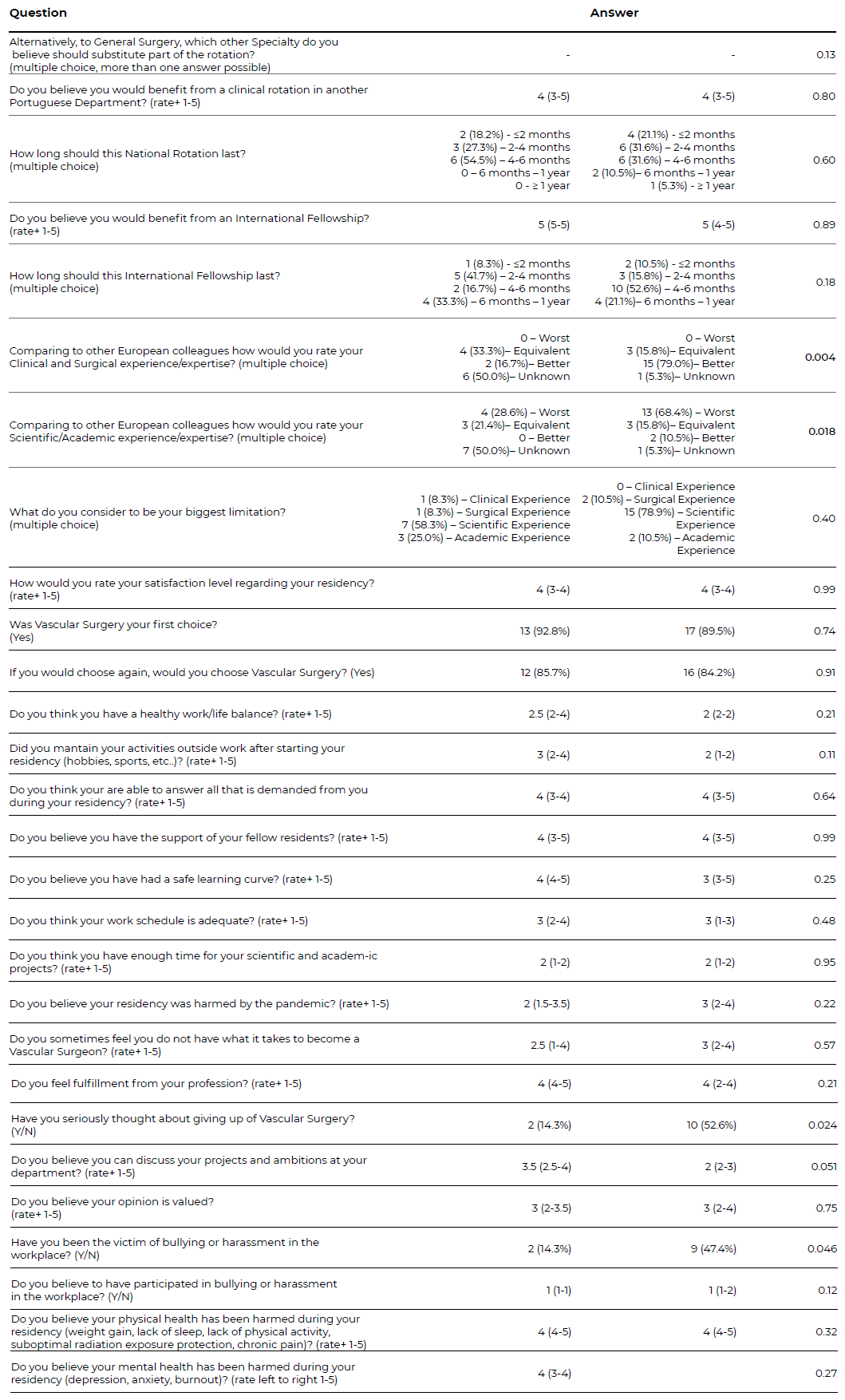
Rating answers are represented as median rate (interquartile range). *Rating answers: 1 - “very bad”; 2- “bad”; 3 - “neutral”; 4 - “good” and 5- “very good”. # Rating answers: 1 - “never”; 2- “rarely”; 3 - “sometimes”; 4 - “often” and 5- “very often”. + Rating answers: 1 - “strongly disagree”; 2- “disagree”; 3 - “neither agree nor disagree”; 4 - “agree” and 5- “strongly agree”. Abbreviations: IQR- interquartile range; Y-Yes; N-No; SPACV- Sociedade Portuguesa de Angiologia e Ciurgia Vascular (Portuguese Society of Angiology and Vascular Surgery); ESVS - European Society of Vascular Surgery.
Discussion
In this study, the authors surveyed vascular residents to gather their perspectives on their training programs and educational concerns. The questionnaire was designed specifically for trainees, as their insights would be most valuable for improving the training programs. The survey included questions with two main objectives: to assess resident satisfaction with the current residency program and to identify limitations and areas for improvement in training. The study had good representation across all residency years, with a reasonable 65% response rate.
Over the past 40 years, Vascular Surgery has undergone significant changes, with an increase in endovascular procedures becoming the initial treatment option for many vascular diseases.4 However, the shift towards endovascular procedures has led to limitations in open surgical training, particularly in aorto-iliac revascularizations, where residents have more experience with endovascular than open repair (Fig. 1 and 2). Trainees identified large abdominal vessels, visceral arteries, infra-renal and juxta-renal AAA, and distal/ultradistal revascularization as areas where additional open surgical training would be beneficial (Fig. 5). The declining number of surgeons with expertise in open aortic repair is a growing concern. In Denmark a National Needs Assessment to Identify Technical Procedures in Vascular Surgery for Simulation Based Training reported the same training limitations.4 Procedure volume in Vascular surgery training trends from 2001-2007 in the USA was reported by Schanzer et al, who described an escalating endovascular procedure volume (increased by 422%) which was not mirrored by an increase in open surgery.5 The number of open aortic procedures decreased by 17.1%, specifically, open aortic aneurysm procedures decreased by 21.8% and open mesenteric or renal procedures decreased by 13%. However, aorto bifemoral bypass due to peripheral artery disease increased by 3.2%, which may have to do with the growing prevalence of atherosclerosis and peripheral artery disease. Infrainguinal bypass procedures remained relatively constant and the number of carotid endarterectomy procedures performed did not change significantly.5 Also in the USA (United States of America), Smith et al studied the Medicare data, and found that the total open aortic repair (OAR) volume among training programs decreased by 38%. In 2014, 25% of programs performed fewer than 10 OARs annually.6
The rapid advances in vascular surgical technology over the last two decades have changed the way that residents are being trained, with a focus on digital technology, simulation, and virtual reality.4,7,8 Evidence suggests that endovascular simulations can improve performance, but their impact on patient outcomes is yet to be proven. Also, the development of simulation-based programs often evolves based on available resources and equipment, reflecting convenience rather than a systematic educational plan.4
Changes in the practice of Vascular Surgery have also led to questions about the utility of general surgery training.9) Although specialties started from a common branch, they are currently quite distant with different preferred minimally invasive approaches (endovascular vs laparoscopy/robotic). Trainees in this study suggested that the General Surgery 12-month rotation should be shortened, and the majority agreed that Radiology should be included in the rotation instead. Aurshina et al reported that the most popular training program sought by vascular trainees in the USA is a 3-year General Surgery followed by 3 years Vascular Surgery program instead of the traditional 5 years General surgery followed 2 years Vascular Surgery. In the latter half of the decade, more vascular trainees preferred the 0 years General Surgery with 5 years Vascular Surgery training paradigm than the prior half of the decade (20% vs. 7%, p=0.0004).9 In Europe, Vascular Surgery training programs vary widely between countries, with some having a mono specialty program and others having a subspecialty model, most after a full general surgery residency program, with full training being between 4 years in Russia to 10 years in Switzerland.10 Considering as Vascular Surgery has evolved, seems evident that the trend tends to be in favor of a more dedicated specialized training, with a higher focus on endovascular procedures, which may have consequences in open surgery experience.
Regarding scientific and academic experience, main limitations/lack of experience were reported in participation in guidelines/scientific recommendations, presentations in international meetings, teaching and training of other professionals, ability to perform statistical analysis and systematic review and meta-analysis (Fig. 3). The difficulty in having time dedicated to scientific activity during the residency is also reported in other studies.8Calligaro et al reported that one-third of programs designated time devoted to research, whereas the others expected fellows to find time on their own.11 Overall, Portuguese vascular trainees rated their clinical/surgical experience as better than their European colleagues, but their academic experience as worse, with scientific experience being the biggest limitation (Table 1).
Regarding personal satisfaction level during residency, most trainees in this study reported a level between 3-4, citing an unhealthy work-life balance and inadequate work schedule. Older residents were more likely to have considered quitting the program, primarily due to burnout and lack of personal time or experienced bullying or harrassment (Table 2). This may be related to the increase in demand and responsibility in the later stages of residency and the struggles to deal with this increase in expectations. These trends should be recognized by those in leading positions in order to address and prevent physician burnout and eliminate the risk of harassment Ours results are in accordance with a national US survey which found that 32% vascular surgery trainees reported having been bullied. However, they didn't find any clearly identified factors predictive of who will experience bullying. The most common perpetrator was direct superior surgeon and the most common barriers to report bullying were fear of loss of support from their supervisor, loss of reputation and effect on career choices. The most common reasons identified for why bullying might occur in vascular training programs were high stress environments and learned behavior from others. Unfortunately, 53% reported no knowledge of institution-specific policies to address bullying in their program.12 Similar alarming data were reported in a Greek study, with 50% of surgical trainees experiencing verbal abuse, 38% threatening behaviour, 20% sexual harassment, and only 15% of institutions reporting official support mechanisms.13 The growing evidence of bullying and undermining in training demands recognition and change. Additionally, in our survey residents felt they could not discuss their projects and ambitions within their departments and their opinions were undervalued. However, they generally agreed that they had the support of their colleagues and were able to meet the demands of their residency (Table 2). A national US survey found that vascular surgery trainees' satisfaction was more dependent on the perception of their workplace peers than integrated residents.1 Trainees reported also physical and mental health issues during their residency, with burnout being associated with higher levels of depression and perceived stress and lower levels of social support and self-efficacy. Janko et al demonstrated the relationship of modifiable work-life balance factors with burnout. The addition of programmatic social events, limiting work hour violations, and formal mentoring programs may decrease levels of burnout.2) According to Calligaro et al, lifestyle concerns are the most important reasons why medical students do not choose Vascular Surgery as a career.14
When asked about the impact of COVID-19 on residency, the answers were not consensual. Despite this, in Portugal, the impact of the COVID 19 pandemic on the functioning of the different Angiology and Vascular Surgery services was undeniable, with several articles published on the subject15)-(28. In northern Italy, an online cross-sectional survey reported also that the impact of COVID-19 on residency was not uniformly perceived by the trainees, with some reporting improved clinical or research competencies while others experienced decreased surgical activities.29 With particular regards to Vascular Surgery, in Southern Regions of the Italian, Martelli et al reported a significant increase in admissions for urgent revascularization for symptomatic carotid stenosis, as well as for revascularization or major amputations for chronic limb-threatening ischemia.30
Finally, trainees considered that the European Society for Vascular Surgery (ESVS) was more effective in addressing their residency concerns compared to the Portuguese Society of Angiology and Vascular Surgery (SPACV), despite both scientific societies received generally positive feedback. However, despite recognizing their benefit and need, most residents reported to having a low participation in these training initiatives perhaps due to lack of time or permission to enroll in these activities (Table 1).
This study has some limitations. The main limitation is the fact that Portugal has a small number of residents limiting our analysis. Additionally, seeing as only 65% participated in the survey, residents who did not respond may have significantly influenced the outcomes reported, generating bias. Also, in spite of being anonymized, the fact that the number of residents/year is low (median of 5.5 residents per year) may have influenced residents response with fear of being honest regarding satisfaction rates. Moreover, the questionnaire was not previously validated or used, it was developed specifically for this study, so definitive conclusions from the responses need further studies and validation. However, seeing as this is the first study conducted in Portuguese Vascular Surgery residents, it brings new lights to current residency limitations and resident’s needs.
One of the main areas we believe is important to address in giving more opportunities for residents to participate and enroll in training activities provided by the ESVS and SPACV, this may be accomplished by a bigger incentive from each department making it part of the training schedule. Also, seeing the growing need of academic training and knowledge in Vascular Surgery, a better balance between surgical training and academic demands needs to be worked on, perhaps with protected dedicated time for research and academia, also considering that residents need personal time for their family and outside work commitments. This will lower the degrees of burnout, stress and ultimately will increase satisfaction, motivation and productivity. Residents’ personal health and wellbeing should be a major concern for training programs and should not be put on hold during the residency time.
Additionally, seeing as expertise in open surgery is a growing limitation, recognized across countries, strategies should be made to address this. Simulation, specialized training programs, resident rotation among departments/teams are all strategies that may improve and address current limitations.
Conclusion
The findings from this study provide insight into the perceptions of the trainees regarding current training limitations and satisfaction rates with the residency program. Key areas such as diminishing experience in open surgery, lack of experience in scientific research, unhealthy work-life balance and current opinion on the need to change general surgery common training duration have been identified. These findings may provide a base for improvement and development strategies in the residency programs in Portugal.