Introduction
Actively diagnosing community-acquired pneumonia (CAP) is the primary goal of patient assessment in acute cough presenting in the emergency department (ED).1 CAP is characterized by an acute lung infection in individuals who have not been hospitalized recently or regularly visited health care facilities.2 It remains a significant cause of morbidity and mortality, accounting for more than 50 thousand deaths and 1.8 million ED visits annually in the United States. It creates a substantial burden on the healthcare system.3 Bacterial CAP is a common and potentially serious illness, and antibiotic treatment is the cornerstone to reduce morbidity and mortality.4
The Brazilian Thoracic Association, Infectious Diseases Society of America, and American Thoracic Society guidelines recommend an empirically initial antibiotic regimen immediately after diagnosis of CAP.5,6 Disease severity must be assessed through validated instruments such as CURB-65 severity score (mental confusion, urea, respiratory rate, blood pressure, and age ≥ 65 years) or PSI (pneumonia severity index), and low-risk patients are treated on an outpatient basis.7
Making an accurate diagnosis of bacterial CAP remains a challenge. The standard approach of low-risk patients is based on clinical suspicion associated with imaging studies with documentation of pulmonary opacities on chest radiography (CR).5,6,8,9 There is not a combination of symptoms and signs to accurately predict CAP, and there´s immense heterogeneity in CR interpretation.10,11
Etiologic tests and biomarkers do not change prognosis in low-risk patients with possible viral etiology treated with antibiotic therapy, and do not have a worse prognosis.5,12 The result is a heterogeneous patient assessment, possibly delaying antibiotic treatment or inadequate empirical antibiotic prescription, leading to overuse, increased costs, and drug resistance.13
CR is a low-cost examination for pulmonary abnormalities in this clinical setting. Recent studies indicated pneumonia could be visualized on chest CT but not on concurrent CR in some cases. Chest multidetector CT scans, as compared to CR, can markedly modify diagnosis and clinical decisions.14,15,16
Chest CT has become widely available in the last decades, and radiation exposure has substantially decreased due to technological improvements.17,18 It´s possible to perform ultra-low-dose chest computed tomography (ULDCT) with radiation doses like in CR frontal and lateral views (average of 0.10 mSv) and present diagnostic accuracy for lung nodules identical to conventional CT.19,20 Previous studies have not evaluated association of ULDCT with treatment of patients with suspected CAP. Presumably, ULDCT is associated with a more precise CAP diagnosis.
This study sought to understand the feasibility of ULDCT in a group of healthy adult patients presenting in ED with suspected CAP. We measured the number of instances in which it was possible to perform ULDCT for a clinical hypothesis of CAP in a previously healthy person presenting to the ED, and the radiation dose associated with it. Also, we measured the time interval between the ULDCT request and the availability of the radiologist report. The rate of antibiotic use was also registered and this information was correlated with the ULDCT result.
Methods
This study was approved by local institutional review board (71739717.7.0000.0071) and registered at ClinicalTrials.gov, Identifier: NCT04541160. Patients who presented to ED were screened. All enrolled patients provided written informed consent before inclusion, and the eligible ones were assigned to their imaging evaluation to ULDCT.
Between October 2017 and December 2018, we prospectively enrolled 131 consecutive adult patients with suspected CAP based on at least one respiratory symptom (new or increasing cough, expectoration, dyspnea, chest pain) and at least one symptom related to infection (fever ≥ 38°C, chills, sweating, myalgia, mental confusion or headache) and focal auscultatory findings during physical examinations (crackling rales), but for whom no definitive diagnosis was possible by clinical judgment (Imaging studies were not included for that decision). Patients without a defined CAP diagnosis, with a score in at least one clinical part of CURB-65 or PSI (pneumonia severity index) scores were excluded due to high probability of antibiotic prescription. Patients with clinical diagnosis of rhinosinusitis and acute nasopharyngitis were excluded. This study aimed to analyze healthy patients, and other exclusion criteria comprised being pregnant; the presence of different respiratory diseases such as chronic obstructive pulmonary disease, asthma, interstitial lung disease, chronic diseases or chronic airway conditions; diagnosis of congestive heart failure; having a body mass index greater than 35; and inability to hold the breath for 10 seconds.
ULDCT images were acquired with an 80-row CT scanner (Aquilion Prime, Canon Medical, Japan) or a 64-row CT scanner (Somatom Definition AS, Siemens Healthcare, Germany), fixed KV (120) and mA (10) with a slice thickness of 0.5-0.6 mm and rotation time up to 0.35 seconds. Fixed mA was applied based on a Toshiba scanner protocol and adapted to a Siemens scanner.21 Total dose length product (DLP) was recorded, and effective doses were obtained using a conversion factor of 0.014. (Figure I). Interval in minutes between the request and report was registered.
Image Analysis
Workstations equipped with PACS systems (Vue Pacs, Carestream, USA) were used for exam readings. Radiologists should read the ULDCT images within 40 minutes of acquisition. Reports were performed by a general radiologist with at least one year of practice. These reports included an evaluation of findings of tracheobronchitis and signs of lower airway infection or pneumonia (described as: centrilobular micronodules, ground-glass opacities, consolidations, nodules with a halo of ground-glass), as well as the location of these findings. They also reported if there were signs of pleural effusion.
After receiving the report from the first observer, the ED physician reassessed the patient and prescribed antibiotics, if necessary.
In an interval of up to 24 hours, ULDCTs were read a second time by a thoracic radiologist with at least four years of experience. In cases of disagreement, a third physician with more than ten years of experience in thoracic radiology made the definitive decision.
Patients whose images did not show disease were followed after one month, by examining their medical record at our institution and, if no new register was found, they were contacted by phone and asked if they sought medical evaluation or were admitted at any other institution due to the current problem during this time interval.
Statistical Analysis
Continuous variables are described as mean ± SD and categorical variables as relative frequency. Comparison of antibiotic prescribing rate according to tomographic findings was performed using a chi-square test. A p-value < 0.05 was considered statistically significant.
Results
113 patients were included from 131 eligible ones. Eight patients refused to sign the informed consent form, and five were excluded due to technical errors during image acquisition. Two patients exhibited BMIs higher than 35 and did not fulfill the inclusion criteria; three patients could not be reached for follow-ups.
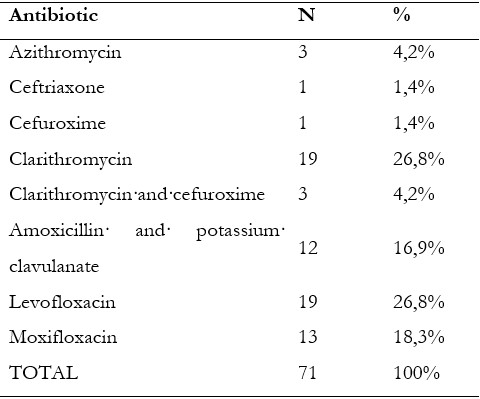
Patients enrolled had a mean age of 43.4 + 12.3 years, 57 (50.4%) were male, and mean BMI was 25.5 + 3.9. Mean CT radiation dose was 0.14 + 0.17 mSV (table I).
Table I: Patients per age, height, gender, weight, body mass index and radiation dose.
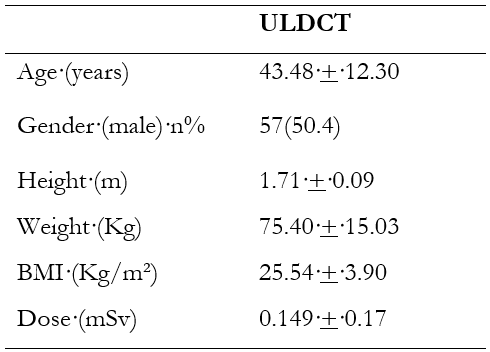
BMI, body mass index; ULDCT, ultra-low dose computed tomography
The interval between request and radiologist’s first report was 43 + 20 minutes.
Forty-four (38.9%) had normal scans (figures 1 and 2), and among patients with any infectious positive finding, 59 (52,2%) had tracheobronchial wall thickening, with or without parenchymal disease, and 42 (37,2%) had parenchymal disease, with or without tracheobronchial wall thickening (Figures 3, 4 and 5).
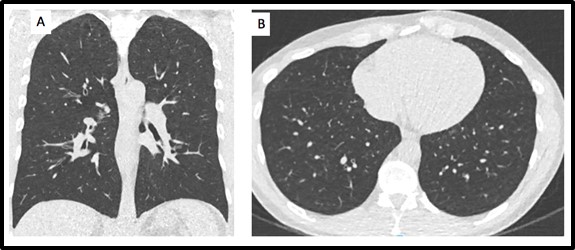
Figure 1: Normal ULDCT of a 42-year-old female, BMI: 22.2, a total of 15.8 DLP (0.22 mSv). A, coronal; B axial. In these images, we can see an ULDCT of a normal chest, demonstrating the good appearance of the images despite the ultra-low dose of radiation.
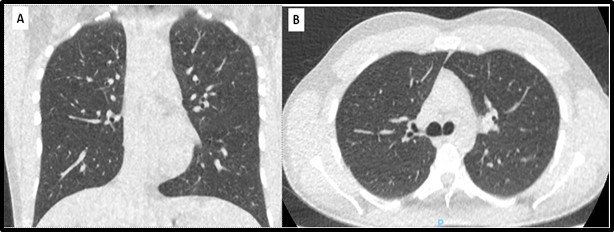
Figure 2: Normal ULDCT of a 26-year-old male, BMI: 20.1, a total of 10.6 DLP (0.15 mSv). A, coronal; B axial. In these images, we can see an ULDCT of a normal chest, demonstrating the good appearance of the images despite the ultra-low dose of radiation.
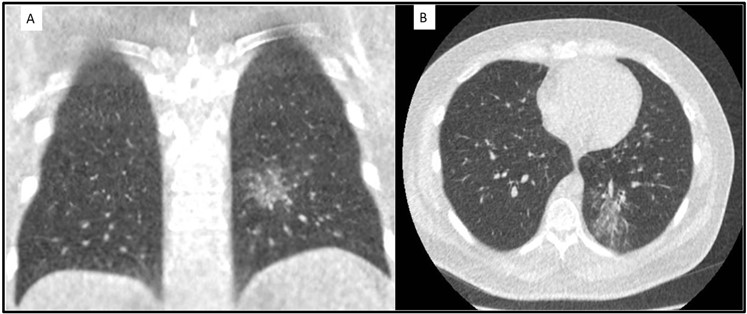
Figure 3: ULDCT of a 39-year-old male, BMI: 31,0, a total of 10.6 DLP (0.15 mSv). A, coronal; B axial. In these images, we can see ground-glass opacities and centrilobular micronodules in the left lower lobe, compatible with a bronchocentric infectious process.
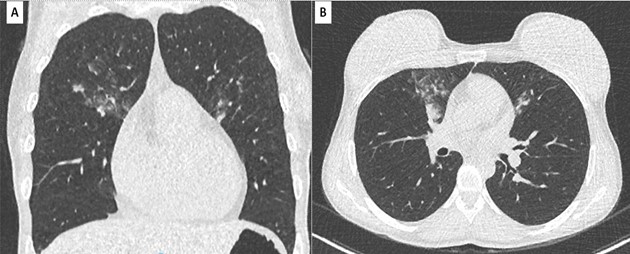
Figure 4: ULDCT of a 40-year-old female, BMI: 20.1, a total of 11.3 DLP (0.16 mSv). A, coronal; B axial. In these images, we can see ground-glass opacities, centrilobular micronodules and small consolidations in middle lobe and lingula, compatible with bronchopneumonia.
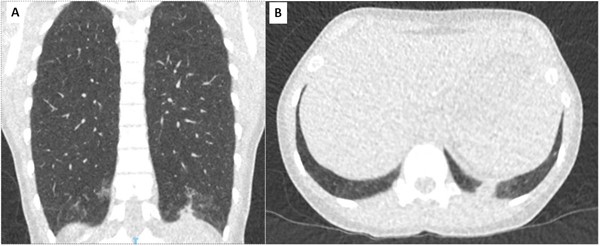
Figure 5: ULDCT of a 40-year-old female, BMI: 20.1, a total of 8,9 DLP (0.12 mSv). A, coronal; B axial. In these images, we can see ground-glass opacities in lower lobes and small consolidation in basal posterior segment of left inferior lobe, compatible with a bronchopneumonia.
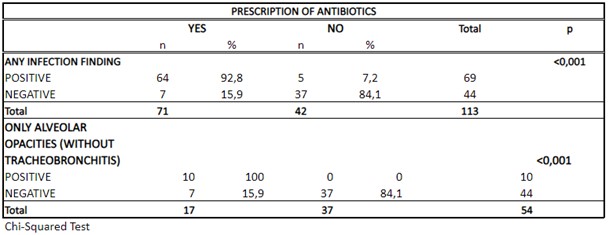
Any tomographic findings suggestive of infection were associated with a greater antibiotic prescription. A total of 71 (62.8%) patients received antibiotics prescriptions.
Table II shows what kind of antibiotics were prescribed.
From 69 patients with any positive infection ULDCT finding, 64 (92.8%) received antibiotic and 5 (7.2%) did not, p<0.001. Five patients of this group did not receive antibiotics for some reason: two for being diagnosed with influenza, and three because they only had bronchial wall thickening and the clinician considered it to be a viral disease and prescribed only symptomatic treatment. Of 44 patients with negative ULDCT, 37 (84.1%) did not received an antibiotic prescription, p<0.001 (table III).
One negative ULDCT patient was admitted to the hospital, because of COPD decompensation, and three of the negative patients sought medical evaluation for a second time and in this second opinion there was no pneumonia diagnosis (this was not statistically significant - p=0.738).
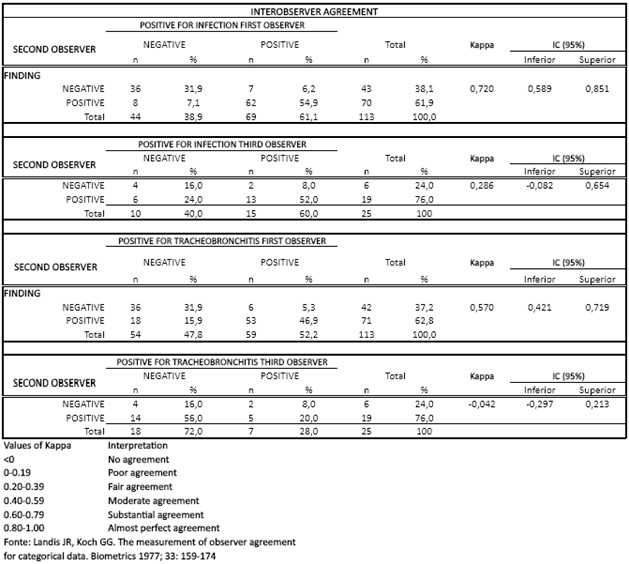
The second observer reviewed all the cases reported by the first observer (total: 113). However, the third observer only reviewed the cases where the second reviewer disagreed with the first (total: 25). Therefore, it is known that the number of cases from the third reviewer were fewer than those of the second. The statistical correlation between the first and second observers was substantial regarding positivity for infection (Kappa 0.720) and Moderate for Tracheobronchitis (Kappa 0.570). However, between the second and third, there was a fair correlation regarding positivity for infection (Kappa 0.286), and there was no agreement for tracheobronchitis (Kappa -0.042). (table IV)
Discussion
This study aimed to assess the practicality of using ULDCT in emergency settings for pneumonia evaluation. ULDCT scans were conducted on 113 patients, with an average time lapse of nearly an hour between scan requisition and the initial report. Notably, normal ULDCT findings were strongly associated with opting for non-antibiotic therapy in 84.1% of cases.
We focused on a cohort of previously healthy patients with genuine clinical uncertainty regarding lower airway infections, where treatment decisions had not yet been finalized. Most patients with acute cough usually present with benign viral infections, often self-limiting and requiring no specific treatment.22 However, diagnosing CAP can be challenging due to its varied clinical presentation and interpretation of CR among ED physicians and radiologists.5,6,23,24 Timely diagnosis is crucial for prompt antimicrobial administration, as delayed treatment can impact prognosis significantly.25 Additionally, distinguishing between influenza and CAP poses another diagnostic challenge.
The American College of Radiology highlights the superior sensitivity and specificity of chest CT over CR in suspected pneumonia cases.26
Our study evaluated ULDCT in patients with acute cough, symptoms, and findings suggestive of CAP in the ED. ULDCT, associated with minimal radiation exposure, provided better lung image resolution compared to CR, thus enhancing diagnostic accuracy.17,18,19,20 Although ULDCT has already been validated for evaluating pulmonary nodules,27,28 and to quantify pulmonary emphysema, diagnosis of pulmonary embolism, and evaluation of acute dyspnea,19,29,30 few studies have evaluated the role of ULDCT in ED.19
In our study, only 15.9% of patients with negative ULDCT results received antibiotics, indicating its high reliability in ruling out pneumonia. Furthermore, findings from Upchurch et al. indicated a lower CAP diagnosis rate after ULDCT evaluation, with no increased complications observed.15
Most treated patients with negative ULDCT exhibited severe cough and intense malaise symptoms or demonstrated high expectations to receive antibiotic therapy. There are guidelines for the use of antibiotic therapy in such clinical scenarios and early diagnosis and appropriate antimicrobial treatment are critical steps in the management of CAP; medical literature has already shown a tendency for ED physicians to overuse antibiotics due to a combination of factors.31 We infer that the ED physician´s decision was made not only including imaging information but also confronted with other factors (i.e., other clinical signs and symptoms, overall medical perception, fear of not treating potentially serious illnesses or not meeting the patient's expectation) since there was not conclusive data regarding the presence of bacterial infection.32
Another study that assessed early multidetector chest CT evaluation of patients suspected of CAP visiting the ED, published by Claessens et al., showed chest low-dose CT scan excluded pneumonia in one-third of the cases in which a parenchymal infiltrate was detected on chest radiograph. In 80% of the cases, it was confirmed during follow-up, performed 28 days after the initial visit. In the same study, 45.5% of patients with no initial antimicrobial therapy were prescribed antibiotics after CT scan results.16 Reclassification was primarily observed in patients not suffering from pneumonia according to the reference diagnosis, thereby suggesting that the potential benefit of low-dose CT would predominantly be in reducing the overdiagnosis of pneumonia.14
Furthermore, it´s already acknowledged that in elderly hospitalized patients with a suspicion of CAP or hospital-acquired pneumonia, low-dose computed tomography alters probability of pneumonia in 45% of cases (probability was upgraded in 15% of cases and downgraded in 30% of cases) with most changes in the intermediate pre-low dose CT probability group, in which more than 80% of them had their probability changed after CT.33
There are some limitations to our study. First, rigorousness of diagnosis of CAP can be questioned since there was not an adjudication committee. Second, confirmation of the causative agent was not pursued, as in our institution many cases of community-acquired pneumonia are treated based on epidemiology, and this distinction is of importance when use of antibiotics is considered. Third, we did not take into account cost-effectiveness of ULDCT, which is more expensive and less available than CR. Fourth, it may not reflect the reality of other imaging centers that may have different resources, which could influence the results. And, regarding the correlation of the observers of the study, a low correlation was noted between the second and third reviewers regarding positivity for infection and there was no agreement regarding tracheobronchitis. In our opinion, this was due to the small number of exams between the second and third reviewers, because the third reviewer only analyzed the cases where the second reviewer disagreed with the first one, and the subjectivity of the analysis of subtle findings of tracheobronchitis.
Conclusion
ULDCT was successfully implemented in a group of healthy adults presenting to ED with suspected CAP. Radiation doses were similar to those described for chest radiography (2-views). Time interval between the ULDCT request and availability of the radiologist report was considered acceptable. Negative exams were associated with a low rate of antibiotic use, reflecting high confidence in results.