A 74-year-old farmer presented to the emergency room with complaints of low back pain. Previously diagnosed with spondylodiscitis of unknown etiology, the patient experienced no improvement with empirical antibiotic therapy. The low back pain persisted for over a year, worsening in the last eight months. Within the last six months, a fistula with drainage to the right flank developed, accompanied by the onset of fever a week prior to hospital admission. Recent imaging revealed significant L5-S1 involvement by spondylodiscitis, along with paravertebral and muscular collections in the right psoas, iliac, and gluteus regions, featuring fistulous tracts to the skin. Incidentally, CT scans uncovered a fusiform aneurysm of the abdominal aorta extending to the right iliac artery, with associated mural thrombosis (Figure 1-2). Bacterial, fungal, and mycobacterial blood cultures remained negative. Positive seroagglutination tests for brucellosis prompted the initiation of gentamicin (14 days), doxycycline, and rifampicin, forming a 3-month therapeutic plan with the latter two antimicrobials. Despite the surgical staff's evaluation opting against surgery, the combined antimicrobial therapy resulted in a significant improvement in the infectious condition, prompting scheduled follow-up appointments. This case presents a rare case of spondylitis in a patient with brucellosis, underscoring the importance of investigating brucellosis in cases of prolonged spondylodiscitis resistant to conventional antibiotic therapy. It also emphasizes the need for heightened suspicion, detailed epidemiological investigation, and specific serological tests to establish the etiological diagnosis of brucellosis.

Figure 1: (A-B) axial and sagittal sections of contrast-enhanced CT showing a collection with capsular enhancement with heterogeneous content (pointed by the arrows), anterior to the vertebral bodies of the sacrum, with extension into the spinal canal, associated with erosion of the vertebral body of L5 and, notably, of S1. (C-D) gadolinium-enhanced T1 sequences showing extension of the collection to the right psoas muscle and erosions, sequestration and bone abscess in the vertebral body of S1 (pointed by the arrows).
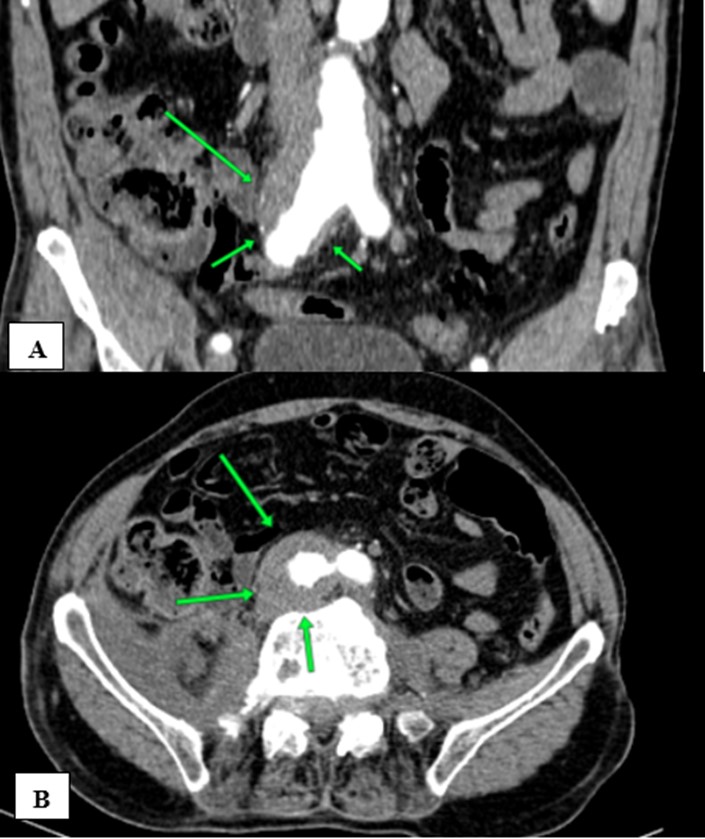
Figure 2: (A-B) axial and coronal contrast-enhanced CT, in the arterial phase, showing as additional finding a fusiform abdominal aorta aneurysm with extension to the right iliac artery.
Radiology assumes a pivotal role in diagnosing brucellosis. While lacking pathognomonic radiographic features, imaging tests can reveal highly suggestive manifestations, including bone erosions, especially in the vertebrae, osteomyelitis, abscess collections, and joint changes. The confluence of clinical, epidemiological, and radiological findings is essential for a definitive diagnosis.1 Literature indicates that the formation of abdominal aneurysms can be a complication of brucellosis infection. In very rare cases, there is an unusual and potentially fatal combination of Brucella infection with spondylodiscitis and abdominal aneurysms. In this case, the absence of signs of aneurysm infection on imaging tests, such as densification of peri-aneurysmal fat, irregularity and thickening of the aortic wall, and peri-aortic soft tissue mass, coupled with no changes in aneurysm configuration post-antibiotic therapy, led to considering it an incidental finding with Brucella spondylodiscitis, rather than a complication of the infection.2 However, we underline the rare possibility of association between these findings.3,4
In the discussed case, radiological exams revealed severe spondylodiscitis at L5-S1, accompanied by paravertebral and muscular collections in the psoas, iliac, and gluteal regions with fistulous tracts extending to the skin. Additionally, computed tomography identified a fusiform aneurysm in the abdominal aorta, extending to the right iliac artery with mural thrombosis. These findings emphasize the pivotal role of radiology in accurate diagnosis.















