A full-term female newborn was born by eutocic deliver, after an uneventful pregnancy. Apgar score 10/10. Right after birth, an occipital swelling was noted, without other findings. Two hours later, the dimensions of the scalp collection had increased significantly, with the edema extending to temporal and periorbital regions (Fig. 1). At admission in intensive care, she was pale, hypotonic, however vital signs and capillary refill time were normal. Head circumference (HC) was 37.5 cm (99th percentile). At admission she presented: hemoglobin 14.4 g/dL, normal platelet count, mild metabolic acidosis (pH 7.313, HCO3- 21.3 mmol/L, base excess of (-)5 and lactate 7.9 mmol/L) and normal coagulation parameters (prothrombin time was 24.9 sec, international normalized ratio of 1.8 and activated partial thromboplastin clotting time was 45.9 sec). A 10 mL/kg bolus of 0.9% saline was administered. At day 2, hemoglobin dropped to 10.1 g/dL, without clinical repercussion, and a transfusion of red blood cells was administered. Maximum HC was 39 cm. Cranial ultrasound excluded intraventricular hemorrhage and cranial tomography confirmed an extensive subgaleal hemorrhage (SGH) (Fig. 2). Phototherapy was required from day 3 to 5 (maximum bilirubin level was 17.76 mg/dL). The newborn was discharged at day 6, with a stable hemoglobin level (17.9 g/dL) and decreasing HC (37.5 cm). Coagulopathy was excluded in follow-up (normal levels of von Willebrand factor and factor VIII procoagulant activity).
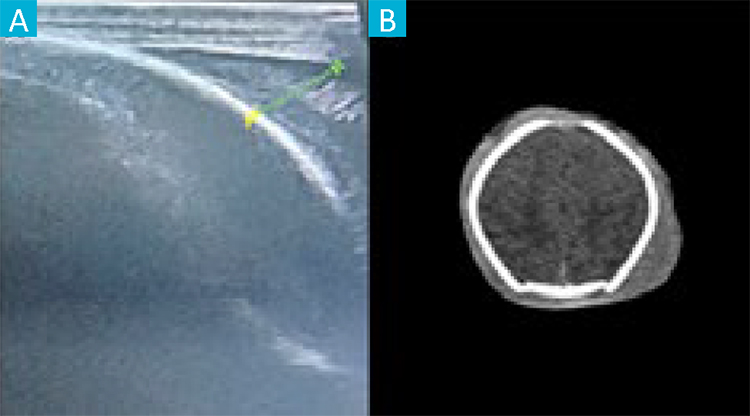
Figure 2: Ultrasound demonstrating the left side of the subgaleal hemorrhage, with 11.10 mm (A). Cranial tomography performed at 24 hours of life, showing an extensive hemorrhage (B).
SGH is a rare and potentially lethal condition in newborns, due to the rupture of emissary veins, causing accumulation of blood between the epicranial aponeurosis and the periosteum.1-3 It should be considered in the presence of diffuse fluctuant swelling, that extends widely and crosses suture lines.2-4 SGH is more frequently associated with vacuum/ forceps assisted delivery, but may also occur spontaneously, with an incidence of approximately 0.4/1000 spontaneous births.1-3 Massive blood loss into that space may lead to acute anemia, hypotension, acidosis and eventually, hypovolemic shock.1,3 Early detection and close monitoring, with prompt administration of fluids and/or blood products are mandatory.3 Imaging study corroborates the diagnosis. After stabilization, the etiological investigation should proceed to discard the possibility of coagulopathy.2
















