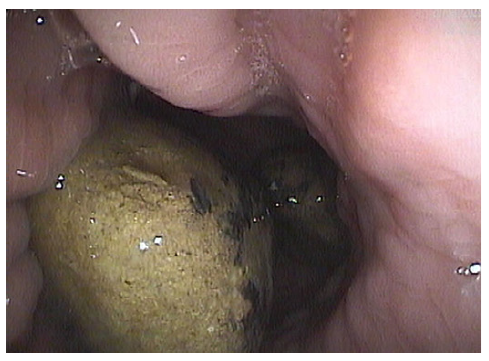
An 80-year-old woman with iron-deficiency anaemia underwent an outpatient upper gastrointestinal endoscopy, presenting two large petrified bodies with 60 mm and 90 mm length in the gastric lumen, associated with a 12 mm ulcer in the incisura (Fig. 1). Past medical history was relevant for type 2 diabetes mellitus and ruled out previous gastric surgeries.
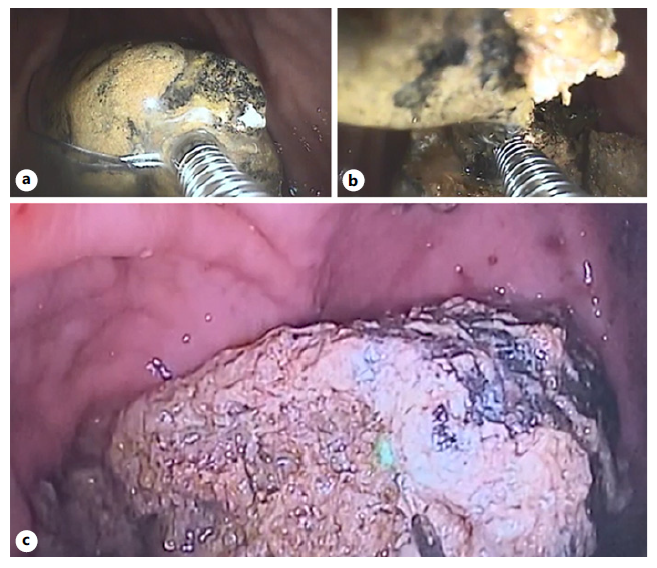
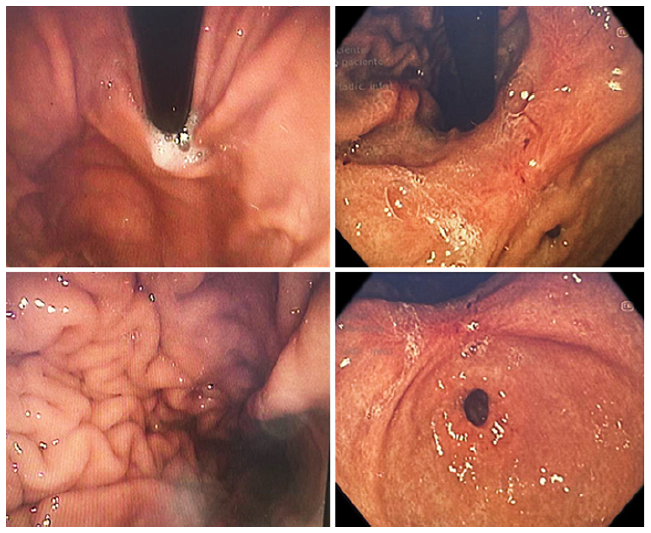
The patient was referred to our hospital and although liver tests and abdominal ultrasound were normal, she performed a magnetic resonance cholangiopancreatography that excluded a cholecystogastric fistula or any fistulous tract between the biliary tree and the stomach. In spite of being asymptomatic, considering the advanced age and high surgery risk, endoscopic extraction was scheduled. A double-channel gastroscope was used for the procedure, which was performed in two sessions (online suppl. video 1; for all online suppl. material, see https://doi.org/10.1159/000533931). Endoscopic re-assessment confirmed the presence of two bulky, hard, and rounded stones with smooth surface impossible to be removed directly using standard retrieval devices. The60mmstone wasfragmentedfromthe periphery using the LithoCrush V™ mechanical lithotriptor (Fig. 2a, b), and all fragments were extracted with a RothNet® during approximately 30 min. However, the 90 mm stone was too thick and round and could not be grasped with any of the available commercially baskets. Fulguration using bipolar and argon plasma coagulation probes at high potencies (120 W) was unsuccessful, with rapid loss of the endoscopic field of view due to smoke. Thus, laser lithotripsy was programed for a second intervention after 3 weeks. Using Auriga™ XL holmium laser and LightTrail™ fibre (600 μm; 120 W) from Boston Scientific, usually applied in urologic surgery, the stone was dissolved, producing smaller fragments that could be further fragmented with the lithotriptor basket and safely removed (Fig. 2c). The procedure was performed in na outpatient setting, under deep sedation and has taken almost 3 h. No associated complications were observed and the patient was further discharged. Pathological analysis was suggestive of phytobezoar. Low-fibre diet was recommended and proton-pump inhibitor prescribed for ulcer healing. One month later, the control endoscopy presented no residual stones or mucosa ulceration (Fig. 3).
Gastric bezoars are foreign bodies resulting from accumulation of undigested material, most commonly vegetable fibres, being rarely associated with severe gastrointestinal complications. Treatment includes chemical dissolution with agents like CocaCola® or acetylcysteine, prokinetics, endoscopic removal, and surgery. Endoscopic therapy involves fragmenting the bezoar using different mechanisms, most commonly forceps, snares, baskets, and argon plasma coagulation [1]. Although endoscopic treatment is not standardized, a minority of cases managed using laser lithotripsy were reported [2-5]. The authors describe a unique case of two giant gastric bezoars successfully treated through laser and mechanic lithotripsy.