A 70-year-old man presented to the dermatology department with a slowly growing, asymptomatic, indurated 10 × 8 cm plaque, with a central white area and erythematous borders, of the right dorsal area (Fig. 1). Seventeen years earlier, the patient had developed a primary cutaneous follicle center lymphoma of the same region and had undergone treatment with 25 sessions of radiotherapy, with a complete response and no recurrence. Before this, no significant atrophy or radiodermatitis was noted.
Histopathology from a punch biopsy revealed no epidermal changes, a marked thickening of collagen fibers, with a dense, mainly perivascular and periadnexal, lymphohistiocytic infiltrate of the reticular dermis and hypodermis (Fig. 2). Perieccrine fat substitution by fibrosis was also present. These findings supported the diagnosis of radiation-induced morphea (RIM). The patient started topical betamethasone with gradual improvement over the next few months.
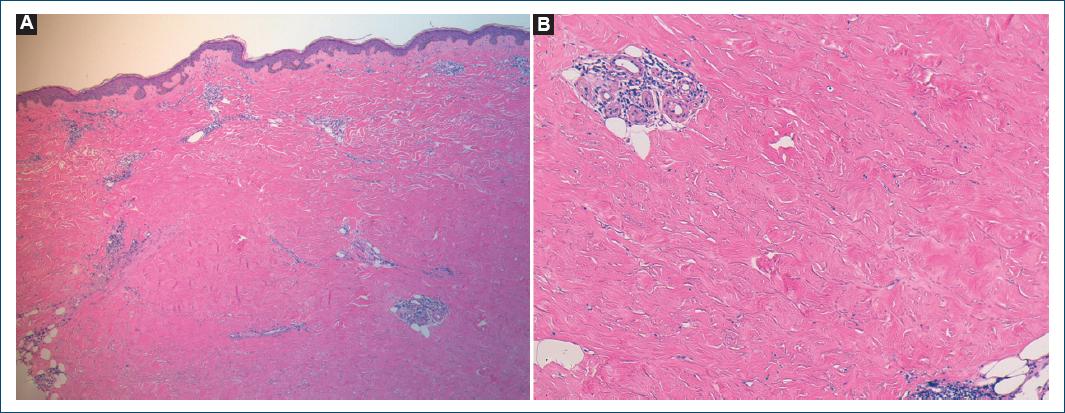
Figure 2 Punch biopsy revealing marked thickening of collagen fibers and a dense dermal perivascular and periadnexal lymphohistiocytic infiltrate (A: H and E, ×40; B: H and E, ×100).
RIM is a rare entity most commonly associated with radiotherapy following breast cancer1. Most cases develop in the months following treatment, but a latent period of several years has been described2,3.
The precise pathophysiological mechanisms leading to RIM have not been established, but increased transforming growth factor-b signaling is thought to be a key element in inducing extracellular matrix deposition and extensive fibrosis2.
Differential diagnosis is vast and includes chronic radiation dermatitis, radiation recall dermatitis, and tumor recurrence, making skin biopsy an important step in these patients' evaluation.
Treatment is difficult and includes potent and superpotent topical corticosteroids, topical calcineurin inhibitors, oral methotrexate, oral corticosteroids, and phototherapy.















