INTRODUCTION
Acute generalized exanthematous pustulosis (AGEP) is a rare type of pustular cutaneous drug reaction. It is mostly drug induced with an incidence of around 1-5 per million population per year.1,2 All ages can be affected, and women are more prone to this reaction. Clinically, AGEP is characterized by high fever and the appearance of numerous small sterile non-follicular pustules on an often edematous and diffuse erythematous base which begins on the face or major intertriginous zones.2,3AGEP should be differentiated from other skin diseases with pustular eruption, such as impetigo, pemphigus foliaceus, staphylococcal scalded skin syndrome, subcorneal pustular dermatosis, and generalized pustular psoriasis (GPP).4 AGEP and GPP are difficult to distinguish due to the similar clinical presentation and initial clinical symptoms. Histopathological examination in AGEP instead of GPP in-volves the presence of eosinophils in pustules or dermis, necrotic keratinocytes, dermal infiltrates with numerous neutrophils and dilated but not tortuous blood vessels, whereas GPP also shows psoriasiform epidermis.5 Even though differentiation of AGEP from GPP may be difficult, histopathological analysis and some clinical features may be helpful.4 We report a case of AGEP which, due to steroid-resistance, was confused with GPP and eventually was successfully treated with methotrexate.
CASE REPORT
A 62-year-old woman visited the emergency department with generalized erythematous pustular eruption, generalized edema, and high fever for approximately five days. The patient had a history of taking propyphenazone one week before admission. Pustular lesions began appearing on the trunk on the second day after drug use and by the day of admission to our unit, had spread to all body regions. Neither the patient nor her family had a history of psoriasis. The patient was obese (body weight 90 kg, height 160 cm, BMI 35 kg/m2) and was using no other medication.
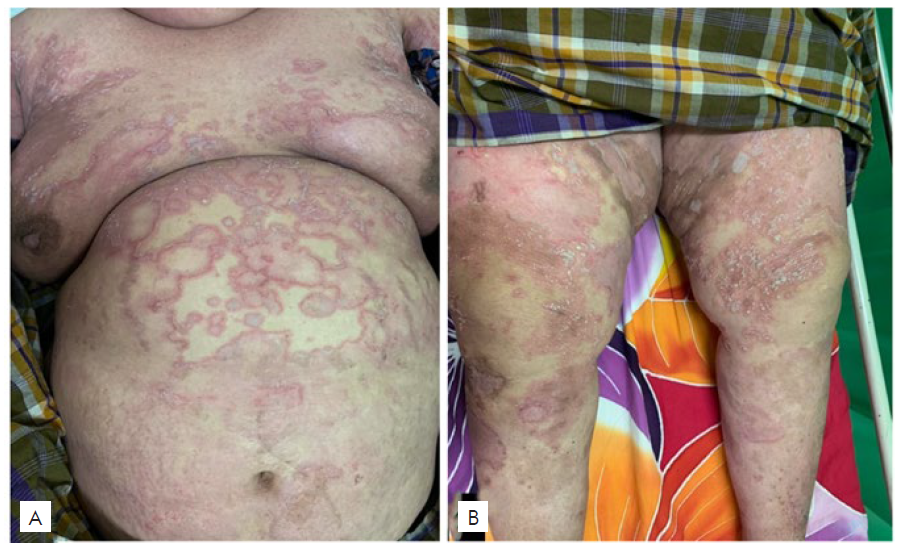
Clinical examination revealed high body temperature (38.50C) and generalized non-follicular pustules with scaly erythematous base on her entire body (Fig. 1), but mostly on the trunk and large axillary, inguinal and sub-mammary body folds. The face was spared. Laboratory tests revealed leukocytosis (18.9x103/uL) with neutrophilia (81%) and elevated erythrocyte sedimentation rate (40 mm/hour). Liver and kidney function tests were normal. Histopathological examination revealed subcorneal spongiform pustule with neutrophils in the epidermis and perivascular inflammatory cell infiltration with neutrophils and some eosinophils in the dermis (Fig. 2). The diagnosis of AGEP triggered by the NSAID propyphe-nazone was established and treatment started with intravenous methylprednisolone 125 mg twice daily, topical desoxymethasone, and topical emollients. Fever and skin lesions improved, but new pustular lesions kept occurring as soon as the steroid dose was reduced. After six days, the patient was given methotrexate (7.5 mg/week) and the steroid dose was slowly tapered. Pustular lesions and erythematous scaly patches improved within six weeks (Fig. 3). After 10 weeks of MTX administration lesions completely resolved, leaving only hyperpigmented macules. No recurrence occurred during the next six months of follow-up.
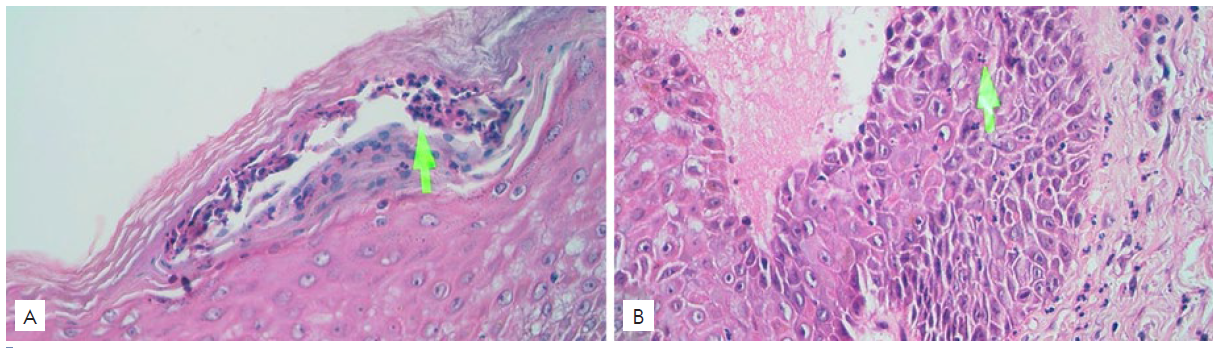
Figura 2 Histopathological examination revealed subcorneal spongiform pustule (A) and perivascular inflammatory cell infiltration in the dermis (B). (H&E, x40).
DISCUSSION
AGEP is a pustular eruption with acute onset that is rare, severe, and has a typical clinical picture.6 Mucocutaneous features consist of tens to hundreds of small, sterile, non-follicular pustules within an erythematous basis with or without minimal mucous membrane involvement and are usually pruritic. Distribution includes trunk and intertriginous areas, as in our patient. Leukocytosis with high neutrophil counts and fever is also a characteristic sign of AGEP.7
AGEP is a sterile neutrophilic inflammatory response associated with activated T-cells in a so-called type IVd hypersensitivity.8 After exposure to the causative agent, activated specific CD4 and CD8 T cells migrate into the dermis and epidermis. Drug-specific CD8 T cells use the mechanism of perforin/granzyme B and Fas ligand to induce apoptosis of keratinocytes, which causes tissue damage. In the early stages of AGEP, vesicles are rich in drug-specific CD4 T cells which release a number of powerful neutrophilic cytokines and lead to neutrophil chemotaxis into vesicles and cause transformation of vesicles into sterile pustules.9 Drug-specific T cells in AGEP patients produce chemokines, namely CXCL8/IL-8, which is significantly involved in the chemotaxis of neutrophils and pustule formation. High levels of IL-17, IL-22, and granulocyte-macrophage colony-stimulating factor (GM-CSF) also play a significant role in neutrophilic activity in AGEP.10
AGEP must be distinguished from various skin diseases that have a pustular eruption, such as impetigo, pemphigus foliaceus, staphylococcal blistering skin syndrome, veiled pustular skin syndrome, and especially generalized pustular psoriasis (GPP). Although diffe-rentiating AGEP from GPP is quite difficult, it may be distinguished by histopathological analysis and some clinical features.4 Generalized pustular psoriasis (GPP) is one of the typical types of psoriasis with an average incidence of age of the 4th decade, but there a number of reports in children and adolescents. Typical features include fever and other systemic symptoms such as malaise, arthralgia, anorexia, and diarrhea which are then followed by sterile acute eruption, sub-corneal pustules with an erythematous skin base with 2-3 mm diameter. Nevertheless AGEP and GPP can co-exist and GPP can even predis-pose to AGEP, as both diseases may be associated with a mutation in IL36R, favoring neutrophilic inflammation.11,12
AGEP is associated with drugs as a cause in more than 90% of cases, most commonly associated with antibiotics, antifungals, diltiazem and antimalarials and less frequently by dapsone, antiepileptic, NSAID, and even corticosteroids.13 Paramex® (propyphenazone), a non-acidic pyrazole NSAID with potent analgesic activity and minimal anti-inflammatory activity,14 has not apparently been described as a cause of AGEP.
AGEP usually has a good prognosis and most cases do not require management other than stopping the causative drug and supportive care,15 but some few cases (<5%) can be life-threatening. Our case did not show rapid remission despite systemic steroid treatment and methotrexate (7.5 mg/week) was used with resolution within six weeks. The mechanism of action of methotrexate correlates with the pathophysiology of AGEP which is a neutrophilic inflammatory response associated with T cells. Methotrexate is generally known as an antimetabolite that inhibits dihydrofolate reductase, an enzyme responsible for the conversion of folic acid to tetrahydrofolic acid in active cell division. It is an anti-inflammatory and immunosuppressive agent by inhibiting lymphocytes and there is another effect, the reduction of neutrophil release.16 Feketeova et al showed a successful treatment of rheumatoid arthritis by MTX which was likely caused by early and considerable inhibition of neutrophil chemotaxis.17
To our knowledge, no cases of AGEP treated with methotrexa-te have been previously reported. Two previously reported cases of steroid-resistant AGEP showed clinical improvement after the administration of dapsone with a dose of 50 mg/day4 and cyclosporine 4 mg/kgBW/day18, respectively. Thus, our report shows that MTX can also be considered as a treatment option in steroid-resistant AGEP.
CONCLUSION
This case presents a generalized pustular eruption initially diagnosed as AGEP which, due to the unexpected clinical journey, later became difficult to distinguish from GPP. However, generalized pustular eruption accompanied by sudden fever, leukocytosis with neutrophilia, a history of new medication, subcorneal spongiform pustule with neutrophils in the epidermis and perivascular inflammatory cell infiltration with neutrophils and some eosinophils in the dermis, and no history of psoriasis favored the diagnosis as AGEP. As the skin lesion worsened after corticosteroid dose reduction, the pa-tient was given methotrexate (7.5 mg/week) and showed significant reduction in pustular lesions and scales within six weeks.