Introduction
Scabies is a neglected tropical cutaneous disease that affects people of all ages1. Children, adolescents, and elderly individuals are the most frequently affected age groups with no gender predilection2,3. However, children are more likely than other age groups to have scabies2. The pervasiveness of scabies in children is approximated to be 5-10%, with the highest predominance in children under 2 years old4.
Poor hygiene, poverty, homelessness, overcrowding, lack of access to medical care, immunodeficiency, indiscriminate sexual activity, and demographic forces (including wars and migration) are significant risk factors for scabies infection2,5,6. Several family members may be infested at the same time, as scabies mites are transmitted by direct and indirect transmission1.
The most prevalent regions of scabies infections are the tropical and subtropical areas, such as Latin America, the Pacific islands, South-east Asia, sub-Saharan Africa, and Northern and Central Australia7-9.
Etiology
Animal mites can be found in six genera: Chorioptes, Cnemidocoptes, Notoedres, Psoroptes, Otodectes, and Sarcoptes, with just the last, addressed in this article6. Sarcoptes scabiei causes scabies in humans, livestock, and wild animals6.
The scabies mite (S. scabiei var. hominis) is an obligate human parasite that belongs to the Sarcoptidae family which is a member of the class Arachnida in the subclass Acari of the order Astigmata2. It is white-brown in color and lives in linear burrows that are dug into the stratum corneum and can be seen by the naked eye as a speck, and skilled dermatologists may be able to notice it using dermoscopy2,3.
The female mite has a size of approximately 0.4 × 0.3 mm while the male is about two-thirds of the female size10,11. The adult mite has four pairs of legs contrasted with the larva which has three pairs of legs10. At the beginning of the scabies mite life cycle, which takes about 14-21 days, the fertilized female burrows into the stratum corneum at a rate of 0.5-5 mm/day and lay 2-4 eggs each day that hatch after 48-72 h into larvae and create new burrows2,5,10. The larvae take approximately 10-14 days to reach adulthood10,11. The life range of a female mite is 4-6 weeks, during which it lays about 40-50 eggs10. Adult male mites may enter the burrows in search of food and unfertilized female mites for mating and die shortly after mating2,3.
The average burden in classical scabies is around 10-20 mites, and between 50 and 250 mites can be found in infants and the elderly3. However, thousands to millions of mites are carried by crusted scabies patients3.
The scabies mites are resistant to soap and alcohol and they either reinfest the host at a different location or infect another human host2. In normal room conditions (21°C and 40-80% relative humidity), scabies mites can survive outside the human body for 24-36 h, but this period can be increased with lower temperatures and higher humidity2; during this time, they remain able to invade5. However, as the amount of time spent away from the host increases, the ability to invade a new host decreases10.
Scabies mites cannot jump or fly and they are less contagious the longer they are separated from their host2. The minimum necessary time for skin-to-skin transmission is 5 min10. Scabies symptoms typically begin 3-6 weeks after the primary infestation and 1-3 days after a reinfestation due to an immediate or delayed (type IV) hypersensitivity reaction to the mites’ products (feces, eggs, and dead parasites)12.
Variants of clinical scabies
Classic scabies
Classic scabies is typically characterized as an intensive cutaneous rash with generalized pruritus that worsens at night6,13. The classic signs include burrows and papules6.
The burrow is a short, 1-10 mm long, serpiginous gray line found on the hands and feet, especially the interdigital spaces, and wrists13. Burrows are rarely visualized to the naked eye, and lesions are often misdiagnosed as excoriated or impetiginized skin13. The papule is usually small and erythematous, often excoriated or covered with a tiny blood clot6.
The erythematous papular rash is generally symmetrical, with a tendency to affect the anterior axillary folds, periumbilical skin, elbows, volar surface of wrists, interdigital spaces, beltline, thighs, buttocks, ankles, areola area in women, penis, and scrotum in men13. The scalp, face, and neck areas are usually spared in adults, but infants and immunocompromised patients may be affected13.
Crusted scabies
Crusted scabies, also known as Norwegian scabies, manifests as hyperkeratotic plaques that contain high numbers of mites14. It often occurs in patients who are immunosuppressed, such as those infected with HIV or after solid organ transplantation14.
Clinically, lesions present as thick, gray, scaly, hyperkeratotic, and crusted plaques that are diffusely distributed and typically cover the hands, elbows, feet, knees, nail beds, trunk, scalp, and in some cases the entire body13,14. In addition, crusted scabies has little to no pruritus6. It is extremely contagious, and if no precautions are taken, outbreaks can occur among family members and patients in hospital wards15.
Nodular scabies
Nodular scabies is an uncommon variant of scabies that is characterized by persistent itchy nodules that can persist even after treatment of the primary infestation16. These nodules are violaceous, pruritic, and between 2 and 20 mm in size13,14. The appearance of nodular scabies is the result of a hypersensitivity response to scabies mites and other products of the infection16. Nodular scabies occurs most commonly on the thighs, axillae, glans, and scrotum13.
Bullous scabies
It is a rare clinical variant that usually presents in the elderly13. It manifests as tense vesicles/bullae, which occur most commonly on the arms, legs, and trunk; they may also be generalized14. Less frequently, they appear on the genitals, buttocks, inguinal folds, thighs, neck, and feet14. Bullous scabies often occurs in patients with pruritic dermatosis who have been previously treated with systemic and/or topical corticosteroids14.
Nail scabies
Nail scabies is an abnormal clinical presentation17. It is often misdiagnosed and can be the initial presentation of scabies13. It affects certain populations such as infants, immunocompromised individuals, and the elderly18.
It may affect multiple fingernails and/or toenails and manifests as nail plate dystrophy, which remains even after successful treatment13.
Scabies incognito
This variant of infestation appears after application of the topical corticosteroid13. The corticosteroid alters the distinctive symptoms and lesions of the scabies infestation14.
Diagnostic methods of scabies
Under ordinary conditions, the diagnosis of scabies can be easily made on the basis of the clinical distribution, the presence of skin lesions, and the patient’s medical history19. However, in certain circumstances, such as patients receiving steroid medications for a prolonged time or those with weakened immune systems, scabies may manifest with an atypical clinical pattern19. In addition, it can be difficult to diagnose scabies in infants or the elderly because their clinical features may differ from those of normal adults19. Therefore, an accurate diagnosis of scabies infection is essential for patient treatment19.
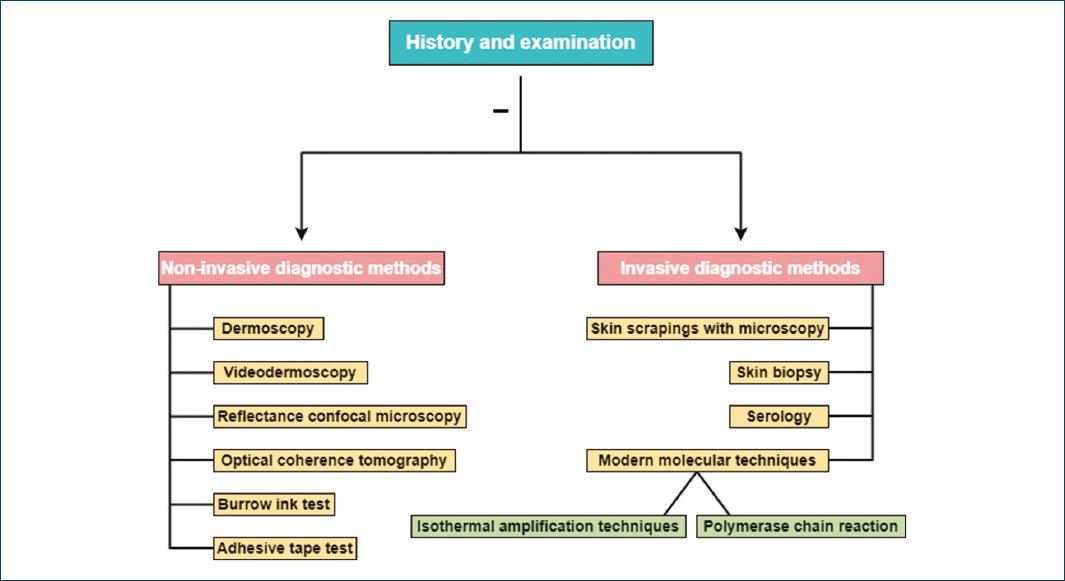
The diagnostic procedure of scabies can be divided into two phases: the presumptive diagnosis (history and physical examination) and the definitive diagnosis (investigations)20.
History and examination
Medical history, physical examination, and history of concomitant infections in family members and close contacts play an important role in the diagnosis of scabies21.
Based on the history of nocturnal itching and the typical distribution of skin lesions, a preliminary diagnosis can be made21.
Dermoscopy
Dermoscopy is an accurate method of diagnosing scabies when performed by a trained physician20. It is a painless procedure that can lead to better patient compliance19. Finding small, dark, and triangular structures at one of the ends of the burrows indicates the existence of the mites20.
However, darker skin phototypes, hairy areas, and complications caused by scratching (such as excoriations, crusts, bleeding, or microscopic dirt particles) make it difficult to identify the scabies mite with dermoscopy1. In crusted scabies, dermoscopy shows multiple burrows and a hyperkeratotic appearance1. Anyhow, the main limitation of dermoscopy is low specificity because of lower magnification10. Other limitations include low sensitivity in mild disease and operator dependence10.
Videodermoscopy
Videodermoscopy is a quick, non-invasive diagnostic method with 100% specificity and greater sensitivity than skin scraping1,10. Since it does not make the patient uncomfortable, it can be used in patients who are non-cooperative10. In addition, it takes less time and reduces the chance of cross-infections10.
Reflectance confocal microscopy (RCM)
Through RCM, the burrows can be seen as linear segments in the middle of the surrounding epidermis that appear as a “honeycomb” pattern1,10. In addition, eggs, feces, larvae, and mites can be seen10. RCM is non-invasive and can be used to study the biological behavior of the mite, as it also shows the movement and peristalsis of the mite10.
Lack of availability and high equipment costs are the limitations of RCM10. Furthermore, the high time requirement is another limitation10.
Optical coherence tomography (OCT)
OCT is comparable to ultrasonography but has a higher resolution and allows visualization of the most important parts of the skin1,10. Mites, burrows, and eggs can be observed and examined10. With the ability to detect the mite both vertically and horizontally, OCT can quickly and precisely diagnose scabies in vivo1.
Burrow ink test (BIT)
BIT is helpful for detecting the scabies mite’s burrows1. A positive BIT results when the ink follows the mite burrow and forms a distinctive, dark, zigzagged line that is easily visible to the naked eye22. If one does not have access to a microscope, dermoscopy, or skin biopsy equipment, this test can be helpful22. However, this method provides only a partial diagnosis and is unable to distinguish between old and new lesions1.
Adhesive tape test (ATT)
In outbreaks in nursing homes and other large accommodations, the ATT is a quick and effective procedure23. This technique is not recommended for people with fragile skin23.
Microscopic examination
Microscopic examination of the mites, eggs, or feces from scales obtained by skin scraping or from the skin biopsy confirms the diagnosis of scabies1.
Skin scrapings at the end of burrows can be used to detect mites, eggs, or feces microscopically23. Although the microscopic examination is inexpensive, a negative result does not rule out infestation, as conventional infection contains only 10-15 mites24.
Skin biopsy is considered one of the most accurate methods for diagnosing scabies1. However, skin biopsy is used only to confirm atypical presentations and is not considered part of the standard examination for the diagnosis of scabies1.
In addition to the previous diagnostic methods, other methods such as modern molecular techniques and serology can help in diagnosing scabies, although standardized laboratory tests for the detection of scabies are not currently available1.
The following diagram summarizes the currently available diagnostic procedures for scabies (Fig. 1)1.
Differential diagnoses of scabies variants
The differential diagnosis of scabies is broad and includes various skin disorders2. Physicians may use objective evidence to confirm the diagnosis of scabies or subjective observations to meet the criteria for a clinical diagnosis or a suspected diagnosis of scabies when a patient presents with classic symptoms such as itching that worsens at night and lesions suggestive of mite infestation, such as burrows located on the flexor areas25.
When patients present with atypical symptoms of scabies, physicians may not suspect that it is a mite-associated dermatosis25. Therefore, it can be difficult to make a definitive diagnosis of scabies surrepticius (non-classical scabies), especially when the clinical history and morphologic features of the lesions suggest another disease or the lesions are infected with a bacterial or viral infection25.
In patients with chronic or progressive skin problems, the possibility of scabies should be considered and further diagnostic testing should be performed, especially if the skin is itchy and unresponsive to therapeutic measures25.
Clinicians should consider the differential diagnoses that may mimic classic scabies, including insect bites, infections (such as tinea corporis, body lice, impetigo, folliculitis, and viral exanthems), drug eruption, and inflammatory or immune-mediated dermatologic conditions (such as papular urticaria and pityriasis rosea)2,5,10,26.
Insect bites such as fleas, mosquitoes, midges, and bedbugs are commonly found on exposed skin as red, itchy, and clustered papules26,27. Papular urticaria manifests as pruritic red and edematous grouped papules/papulovesicles representing hypersensitivity to insect bites27,28. The lesions generally prefer the extensor sides of the extremities, although the trunk is also often affected28.
Folliculitis is identified by erythematous papules and pustules that are asymptomatic, pruritic, or mildly painful, and located around the hair shaft29. Although any area that has hair can be affected, folliculitis often affects only the face, scalp, thighs, armpits, and groin29.
Dermatitis such as eczema, contact dermatitis, and atopic dermatitis is considered also as differential diagnoses of classic scabies26,27. Atopic dermatitis manifests as dry, scaly, erythematous, and itchy skin plaques, which commonly affect the face, neck, elbows, and knee extensors of infants, later including the flexures27.
Gianotti-Crosti syndrome (GCS) is sometimes mistaken for scabies because of the high percentage of acral papules28. The extensor sides of the limbs, buttocks, and cheeks all have a symmetrical distribution of papules28. In contrast to scabies, GCS is almost never as itchy as scabies; mite burrows and excoriations are a regular occurrence in scabies but are the absolute exception in GCS28.
Other diseases characterized by extensive scaling, such as psoriasis, Darier’s disease, drug eruption, lichen planus, palmoplantar keratoderma, and seborrheic dermatitis are potential differential diagnoses for crusted scabies14,15,26.
Scabies masquerading as an adverse drug reaction has rarely been described25. In any patient with a suspected drug eruption who develops pruritic dermatosis after discontinuation of the drug and presents with clinical lesions resembling crusted scabies, the physicians should be aware of the possibility of drug eruption-like scabies (scabies surrepticius)25.
In a patient with persistent nodular rash, nodular scabies must be investigated as part of the differential diagnosis16. Nodular scabies might imitate a solitary cutaneous mastocytoma as it can give a positive Darier sign2. Nodular scabies may be mistakenly diagnosed as Langerhans cell histiocytosis, non-Langerhans cell histiocytosis, insect bites, lymphoma, or urticaria pigmentosa14,30.
In case of blistering is present (bullous scabies), other skin disorders should take into account as differential diagnoses include bullous pemphigoid, bullous impetigo, acquired epidermolysis bullosa, arthropod bite reaction, pemphigus, and dermatitis herpetiformis2,5.
The lesions in pemphigoid scabies resemble bullous pemphigoid clinically, histologically, and on immunofluorescent findings13,14. Subepidermal blisters and eosinophilic dermal inflammation can be seen under a microscope with a potential presence of mites in bullous scabies14.
The diagnosis of nail scabies is frequently mistaken with onychomycosis, nail psoriasis, traumatic nails, and nail dystrophy17. However, nail scabies has been documented in the literature in association with periungual scaling and crusting, distal onycholysis, longitudinal nail splitting, subungual hyperkeratotic deposits, and nail plate deformity/hypertrophy17.
Infants and young children under 2 years of age are particularly susceptible to scabies30. Infants may have diagnostic concerns due to low suspicion of scabies, eczematous changes, and inappropriate therapy, particularly topical steroids30. It is important to distinguish infantile scabies from other entities that present similarly in this age group such as infantile acropustulosis, papular urticaria, and atopic dermatitis10. Many studies have highlighted the possibility that scabies in infants may resemble other skin diseases, such as bullous pemphigoid, Langerhans cell histiocytosis, adverse drug reactions, lymphomatoid papulosis, lupus erythematosus, psoriasis, or an allergic reaction to an insect bite30. In addition, infantile seborrheic dermatitis, which manifests as scaly and greasy plaques on the face and scalp, has a similar appearance to scabies27.
The differential diagnoses of scabies based on each variant are summarized in the following table (Table 1)2,5,10,14,15,17,26,31.
Table 1 The differential diagnoses of scabies variant
| Scabies variants | Differential diagnoses |
|---|---|
| Classic scabies | − Atopic dermatitis − Contact dermatitis − Seborrheic dermatitis − Folliculitis − Papular urticaria − Tinea corporis − Impetigo − Body lice − Insect bites − Drug eruption − Varicella − Pityriasis rosea − Infantile acropustulosis − Gianotti-crosti syndrome − Psoriasis − Cutaneous mastocytosis − Langerhans cell histiocytosis |
| Crusted scabies | − Seborrheic dermatitis − Psoriasis − Palmoplantar keratoderma − Darier’s disease − Drug eruption − Lichen planus |
| Bullous scabies | − Bullous pemphigoid − Bullous impetigo − Acquired epidermolysis bullosa − Arthropod bite reaction − Pemphigus − Dermatitis herpetiformis |
| Nodular scabies | − Solitary cutaneous mastocytoma − Langerhans cell histiocytosis − Non-langerhans cell histiocytosis − Insect bites − Lymphoma − Urticaria pigmentosa |
| Nail scabies | − Psoriasis − Onychomycosis − Traumatic nails |
Complications of scabies
The secondary medical, psychosocial, and economic factors that are related to the burden of disease must be taken into account when estimating the true global burden of scabies32. In the context of the impact of the disease, morbidity associated with scabies is commonly underestimated22.
Severe rubbing or scratching prompts changes such as bleeding, crusting, or excoriations and can lead to secondary bacterial skin infections10,14,15.
Secondary infections and impetiginization, most commonly caused by Group A Streptococcus (GAS) and Staphylococcus aureus (S. aureus), are the most common complications associated with scabies10,33. Staphylococcal and streptococcal growth is promoted by the ability of the scabies mite to disrupt the human complement system by blocking all complement initiation pathways, resulting in decreased neutrophil activity34. These bacteria can also be isolated from skin tunnels, and feces indicate that mites may be contributing to the bacteria’s distribution35.
S. aureus can also lead to superficial acute impetiginization, abscesses, ecthyma, cellulitis, paronychia, staphyloderma, erysipelas, and furunculosis8,34. However, it can also progress to endocarditis, osteomyelitis, and bacterial sepsis, which can be life-threatening8. Whereas, local skin and soft-tissue infections, such as superficial pyoderma, skin abscesses, and cellulitis, as well as more severe necrotizing fasciitis, can be caused by GAS8.
Impetigo is a common complication of scabies itching, especially in children and patients who live in overcrowded conditions36. Impetigo that is caused by Streptococcus pyogens can lead to toxin-mediated diseases such as scarlet fever, rheumatic fever, streptococcal toxic shock syndrome, and post-streptococcal glomerulonephritis10. S. pyogens infection of the skin may also cause reactive arthritis-synovitis, necrotizing fasciitis, and pediatric autoimmune neuropsychiatric disorder2.
Infectious complications seem to be more severe in crusted scabies36. This may be caused by the patient’s comorbidities, such as immunosuppression, as well as deeper excoriations that result in invasive infections and severe sepsis, which lead to a high risk of mortality36,37. Furthermore, crusted scabies cases may develop generalized lymphadenopathy and eosinophilia3,20.
Crusted scabies can also cause malodor as a secondary bacterial infections2. Colonization of the burrow by S. aureus can lead to erythroderma, septicemia, and superinfection with S. pyogenes, which causes glomerulonephritis and rheumatic fever38.
In addition, scabies herpeticum may occur when crusted scabies is superinfected in association with herpes simplex2.
Systemic complications such as bacteremia, acute post-streptococcal glomerulonephritis, streptococcal and staphylococcal sepsis, acute rheumatic fever, and rheumatic heart disease can be associated with a high risk of mortality4,33. Patients with a previous history of scabies are more likely, according to some studies, to develop bullous pemphigoid and chronic kidney disease39.
Renal damage without symptoms can occur in scabies patients40. The morbidity and mortality associated with chronic renal disease are important late complications of scabies32.
Scabies patients suffer from a deteriorated quality of life that is linked directly to their itchiness34. Up to 90% of scabies patients have sleep disturbances caused by itching36. Sleep disturbances may be associated with tiredness, reduced productivity, and reduced ability to concentrate2. After eradicating the scabies mite, post-scabetic pruritus can be stubborn and debilitating, and it may last for a long period2.
Scabies can cause psychosocial complications such as low work attendance, social stigmatization, and feelings of shame36. In addition, it can cause loss of performance at school, school absenteeism, fatigue, and lack of concentration or memory in infants36.
Scabies can cause a significant financial burden, particularly on patients with severe systemic complications2. Rarely, scabies patients may develop generalized urticaria2.
In rare cases, scabies can have unusual complications such as cutaneous vasculitis, vascular purpura, and glomerulonephritis, which may occasionally foreshadow the original disease41.
Scabies patients also have a higher risk of pernicious anemia, intellectual disability, and bipolar disorder, according to some studies2.
The complications of scabies are demonstrated in the following table (Table 2)2-4,8,10,33,34,36,37,39,42.
Table 2 Scabies complications
| Secondary to skin infection | Secondary to itching/scratching | Psychosocial | Other | |
|---|---|---|---|---|
| Cutaneous | Systemic | |||
| − Superficial acute impetiginization − Superficial pyoderma − Abscesses − Ecthyma − Cellulitis − Paronychia − Furunculosis − Erysipelas − Staphyloderma − Scabies herpeticum − Bullous impetigo − Malodor |
− Endocarditis − Osteomyelitis − Bacterial sepsis − Pernicious anemia − Acute post-streptococcal glomerulonephritis − Acute rheumatic fever − Scarlet fever − Rheumatic heart disease − Streptococcal toxic shock syndrome − Chronic kidney disease − Reactive arthritis-synovitis − Necrotizing fasciitis − Pediatric autoimmune neuropsychiatric disorder − Lymphadenopathy − Eosinophilia |
− Bleeding − Crusting − Excoriations − Sleep disturbances − Tiredness − Reduced productivity − Reduced ability to concentrate − Increased risk and severity of skin conditions (such as psoriasis and atopic dermatitis) |
− Low work attendance − Social stigmatization − Feelings of shame − Loss of performance at school − School absenteeism − Fatigue − Lack of concentration or memory in infants − Intellectual disability − Bipolar disorder |
− Significant financial burden − Generalized urticaria |