Case Presentation
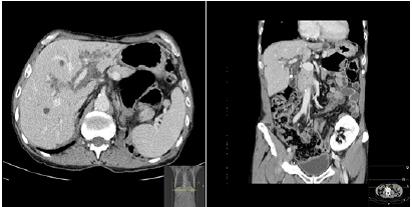
A 68-year-old patient with a history of chronic kidney disease and kidney transplantation due to autosomal dominant polycystic kidney disease (ADPKD) was referred to a Gastroenterology consultation for the evaluation of bile duct dilatation detected in abdominal ultrasound. Laboratory results did not reveal significant changes on liver tests. Abdominal computed tomography (CT) was initially performed followed by magnetic resonance imaging (MRI). The CT scan (figure 1) showed the liver with normal morphology and dimensions, with regular contours and homogeneous density. Multiple dispersed hepatobiliary cysts were identified, the largest measuring around 36 mm in segment II. Linear hypodensity was observed involving the hepatic hilum and intrahepatic portal branches, an aspect that may correspond to biliary duct dilation or peri- biliary cysts in the context of known ADPKD. Cholangio- RM was suggested for better characterization.
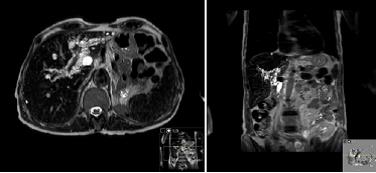
The MRI (figure 2) clarified the CT findings, showing countless millimeter-sized cysts (with hypointense signal on T1-weighted sequences and hyperintense signal on T2- weighted sequences, without contrast-enhancement) in the peri-portal topography, without communication with the biliary tract. These findings indicate the diagnosis of peribiliary cysts.
Discussion
Nakanuma et al. in 1984, described for the first time an autopsy series that showed multiple peribiliary cysts at the hepatic hilum and around the larger portal tracts.1 These cysts were adjacent to, but not communicating with, the biliary tree and resulted histologically from dilation of the periductal glands.2
Several studies listed several etiologies for peribiliary cysts. Most arise in the context of chronic liver disease, more commonly in cirrhotic patients, and are likely associated with disorders of the intrahepatic circulation, most likely of the portal venous system.3 Additionally, it is reported that peribiliary cysts occur more frequently in patients with alcoholic liver cirrhosis than in other causes of cirrhosis.4 A minority is associated with polycystic liver disease, with special predilection for patients with concomitant autosomal dominant polycystic kidney disease.5
With the improvement and greater availability of imaging techniques, the diagnosis of peribiliary cysts has increased.6 The familiarization of radiologists with this diagnosis is crucial. On the one hand, the growth of these cysts can result in extrinsic compression of the biliary tract, and subsequently obstructive jaundice.7 On the other hand, a wrong diagnosis leads to excessive request for additional tests and, eventually, unnecessary invasive procedures.8
Ultrasound typically shows the presence of multiple anechoic cystic lesions adjacent to the central intrahepatic bile ducts and the right and left branches of the portal vein. However, in some cases, only anechoic tubular lesions are identified in the same topography, a finding that simulates dilatation of the bile ducts.9,10
Computed Tomography reveals the presence of multiple cysts or hypointense linear/tubular areas without contrast enhancement, parallel to and on both sides of the portal vein branches. These findings should not be misinterpreted as bile duct ectasia.9,10
In MRI, multiple clustered of small fluid-filled cavities are observed in peri-portal topography, with hypointense signal on T1-weighted sequences and hyperintense signal on T2-weighted sequences, without communication with biliary ducts. There is no restriction on DWI sequences.9,10The differential diagnosis of peribiliary cysts include: biliary duct dilatation, primary sclerosing cholangitis, Caroli’s disease, bile duct hamartomas and periportal edema.11 With this case, we systematized the clinical setting and imaging findings that favor this entity in order to preventing misdiagnosis, unnecessary diagnostic investigations and interventions with great morbidity.