A 24-year-old female presented with an asymptomatic anterior midline neck mass, which developed over the last 6 months. Past medical history was irrelevant. Physical examination revealed a painless, moveable, hard mass.
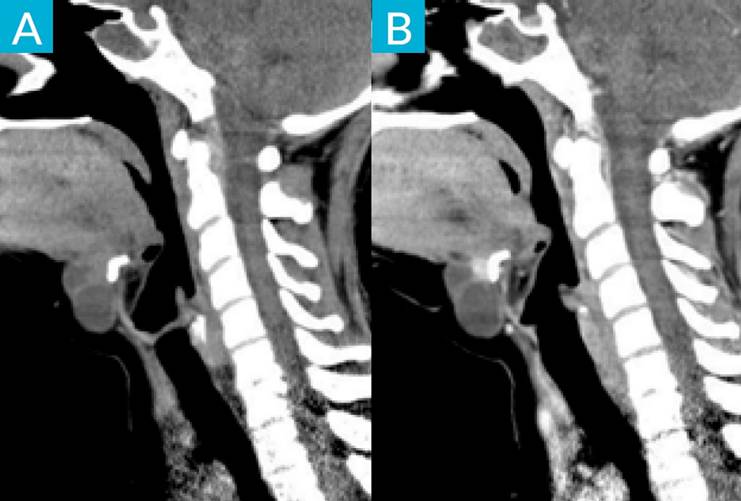
Cervical ultrasound demonstrated a 4 x 3 cm mainly cystic lesion, consistent with a thyroglossal duct cyst (TGDC), presenting focal solid areas with microcalcifications. Contrast-enhanced computed tomography (CE-CT) showed the lesion located in front of the hyoid bone, with upward extension into oral cavity, and revealed an enhancing mural nodule. These characteristics raised suspicion of malignancy, specifically for papillary carcinoma due to the presence of microcalcifications. A fine needle aspiration biopsy (FNAB) was performed, which revealed cancerous cells, consistent with TGDC papillary carcinoma.
There was no evidence of lymphadenopathy or thyroid nodules. The patient was treated surgically with a Sistrunk procedure, and the diagnosis was confirmed by histopathological examination. At 6-month follow-up, there was no evidence of tumour recurrence.
TGDC is the most frequent congenital midline lesion of the neck.1 It may contain ectopic thyroid tissue with potential to develop malignancy.2 TGDC carcinoma is a very rare lesion (less than 1%), and the most common histologic type is papillary carcinoma (80%-95%).3
They commonly present as an asymptomatic neck mass, and it should be suspected when the lesion is hard or fixed.3,4) They are more frequent in females from third to sixth decade, as seen in our case.1
Cervical ultrasound and CE-CT are fundamental to characterize and adequately stage these lesions. Carcinoma should be considered in TDGC that have a mural nodule or microcalcifications, which correspond to the psammoma bodies seen histologically in papillary carcinomas.5 FNAB is an important tool to evaluate suspicious lesions but has a low sensitivity.4 The diagnosis of TGDC carcinoma can be confirmed in the post-operative histopathological examination.1
The mainstay of treatment is the Sistrunk procedure, which consists of excision of TGDC, the central portion of hyoid bone and a core of tissue around thyroglossal tract to open into the oral cavity at the foramen cecum. Thyroidectomy and neck dissection should be considered, depending on risk stratification and if there is concurred malignancy.1,4
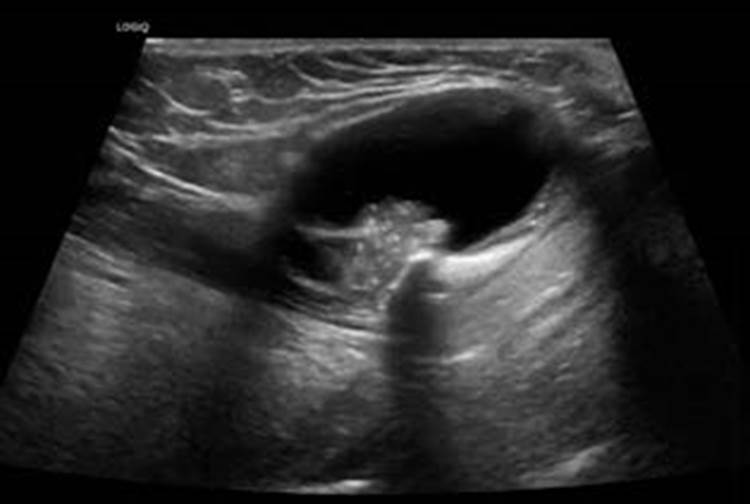
Figure 1: Thyroglossal duct cyst papillary carcinoma. A cervical ultrasound scan shows a cystic lobulated lesion, located anterior to the hyoid bone, with a hyperechoic solid lesion with microcalcifications inside