Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Portuguese Journal of Nephrology & Hypertension
Print version ISSN 0872-0169
Port J Nephrol Hypert vol.30 no.1 Lisboa Mar. 2016
MINI-REVIEW
Takotsubo cardiomyopathy in patients undergoing haemodialysis – mini review apropos of a case
Cardiomiopatia Takotsubo em pacientes de hemodiálise – mini revisão a propósito de um caso
João Carlos Sousa Torres, Rita Lorena Birne, Tiago Assis Pereira, Henrique Silva Sousa, Antónia Calenga, Patrícia Branco, Maria Augusta Gaspar, José Diogo Barata
Hospital de Santa Cruz, Carnaxide, Lisboa, Portugal.
ABSTRACT
Takotsubo cardiomyopathy is an uncommon clinical entity that mimics acute coronary syndrome (ACS) and may be underdiagnosed among haemodialysis (HD) patients. This topic is, therefore, reviewed based on a clinical case of a 68-year-old woman undergoing haemodialysis. Usually, Takotsubo cardiomyopathy presents itself as an acute myocardial infarction. However unlike ACS, neither a coronary obstructive disease is found nor do cardiac biomarkers correlate with the extensive wall motions defects (apical and midventricular kinesis dysfunction along with basal hypermotility). This defect translates into a jarshaped appearance in ventriculography, and therefore its Takotsubo name (octopus trap, in Japanese tako means octopus and tsubo means jar). So far, data available from animal models and its resemblance with pheochromocytoma-induced cardiomyopathy suggests that an adrenergic surge might be an underlying mechanism. The overlapping clinical features of takotsubo cardiomyopathy and ACS, the high prevalence of cardiovascular risk factors and the already superimposed cardiovascular disease in chronic kidney disease make it difficult to diagnose among these patients.
Key-Words: Apical balooning syndrome; haemodialysis; stress cardiomyopathy; sympathetic nervous system; takotsubo cardiomyopathy
RESUMO
A cardiomiopatia takotsubo (CT) e uma entidade que mimetiza clinicamente a sindroma coronaria aguda (SCA) e que poderá ser subdiagnosticada na população hemodialisada. Este tema e revisto com base no caso de uma doente de 68 anos. Habitualmente a CT apresenta -se como um enfarte agudo do miocardio.
No entanto, ao contrario da SCA, nao sao detectadas lesões coronárias obstrutivas nem existe uma correlação entre os defeitos de motilidade cardíaca (disfunção cinética apical e hipermotilidade basal) e a ligeira elevação dos marcadores de necrose miocardica. Na ventriculografia este defeito apresenta-se como uma imagem de jarro, dai o nome Takotsubo (armadilha de polvos, da tradução do japonês em que tako significa polvo e tsubo jarro). Ate a data, com base nos dados provenientes de modelos animais e a semelhança da lesao cardiaca induzida pelo feocromocitoma, parece que o mecanismo fisiopatologico e decorrente de uma descarga adrenergica aguda. Trata -se de uma entidade difícil de diagnosticar no doente renal crónico, dificuldade que advém da semelhança clinica entre a CT e a SCA, elevada prevalência de factores de risco cardiovascular e pesada morbilidade cardiovascular nesta população.
Palavras-Chave: Cardiomiopatia de stress; cardiomiopatia takotsubo; hemodiálise; sindroma de balonização apical; sistema nervoso simpático.
BACKGROUND
Takotsubo cardiomyopathy (TC), first described in 1991, was named after its resemblance with the Japanese octopus trap in ventriculography1(1).
Reflecting the relationship between cardiac dysfunction and stressful triggers2 (physical and psychological) it is also called apical ballooning syndrome, broken heart syndrome or stress cardiomyopathy.
Only ten years after its first description and following the published Japanese series by Tsuchihashi et al. has it been recognized as an independent nosological disease3.
Although TC mimics acute coronary syndrome (ACS), some important differences need to be accounted for, such as the absence of obstructive coronary artery disease, the usual full recovery with medical care and its low recurrence rate (below 10%)4.
In a 2008 study, takotsubo cardiomyopathy was recognized in 6,837 among 33,506,402 patients from the Nationwide US Inpatient Sample, an incidence of 0.02%. The overall frequency of TC was calculated to be 5.2 per 100,000 for women and 0.6 per 100000 for men5. On the haemodialysis (HD) population, data on takotsubo cardiomyopathy is truly scarce. Through a research in PubMed NCBI database we were able to identify only eight cases of patients undergoing chronic Haemodialysis6-10, two on peritoneal dialysis11,12 and only one on continuous venovenous haemodiafiltration13.
The rarity of published cases may result from underdiagnosis, because if a complete cardiological evaluation is not performed the diagnosis may go unnoticed.
CASE SUMMARY
A 67-year-old Caucasian woman was admitted to the Emergency Department with progressive dyspnea over the last 24 hours.
Her medical history was significant for long–term hypertension, dislipidaemia and chronic kidney disease due to proliferative membranous glomerulonephritis type I, on regular haemodialysis for 5 years.
Prescribed medication included bisoprolol 2.5 mg qd, rilmenidine 1 mg bid, minoxidil 5 mg bid and losartan 50 mg qd. No reports on ischaemic heart disease, smoking, alcoholism or drug abuse were known.
On admission she presented with cachexia (body mass index of 16 m2/kg), was hypertensive (blood pressure 220/130 mmHg) and with cold and sweaty extremities. On thoracic auscultation, bibasal crepitations and tachycardic regular heart sounds were detected. Physical exam was otherwise unremarkable.
Chest radiography showed reticulointerstitial infiltrates and right pleural effusion. Laboratories were remarkable for a slight increase in troponin I (0.84μg/L) and lactates (4.6 mmol/L).
Altogether it was interpreted as an acute pulmonary oedema, and the marginal rise of troponin as a consequence of fluid overload. The patient underwent HD for 240 minutes and begun to improve clinically. However, after 210 minutes, she felt an intensive retrosternal pain for which coronary syndrome evaluation was undertaken. Despite the 6.7% weight loss (2.5Kg) during dialysis session, she remained hypertensive by the end of the treatment (187/132mmHg).
The electrocardiogram (ECG) showed tachycardic sinusal rhythm (106bpm), left axis deviation (-50°), a new onset right bundle branch block (RBBB), T wave inversion on limb leads (dI, dII, dIII avF) and V4 -V6 precordial leads.
Troponin I levels increased steadily, maxing out at 3.53 μg/L 24h after admission. A coronariogram showed a coronary diffuse calcification and an anterior descendent artery (30%), circumflex artery (50%) and right dominant (70%) coronary stenosis (Fig. 1). Nevertheless the coronary blood flow was not compromised (TIMI score of 3). The ventriculography revealed the typical apical ballooning image of the left ventricle (LV), which resulted from the middle and apical segments hypokinesis (Fig. 2). These findings were confirmed by transthoracic echocardiography (Fig. 3).
Antihypertensive medication was intensified, particularly the beta-blocker bisoprolol (5mg qd) was incremented, and isosorbide dinitrate (5mg bid) and irbesartan (150mg qd) were added.
From the first day onwards troponin I levels decreased linearly to 0.27 uL/L by the tenth day. By the fourth day, regional wall motion abnormalities (RWMA) improved slightly on echocardiogram and by the tenth, both T waves and RBBB reversed.
The patient was discharged after ten days and, despite the clinical improvement, she was referred to psychiatric consultation. She was diagnosed a reactive depression following recent family conflicts for which she was medicated with escitalopram 10mg qd.
Over the next six months she remained clinically stable, with no reports of thoracic pain. The elective re-evaluation echocardiography documented a complete reversal of the RWMA, reinforcing the hypothesis of takotsubo cardiomyopathy.
In order to strengthen the diagnosis, intracranial lesions and pheochromocytoma were ruled out. Two days after the patient admission a brain-CT scan did not detect solid lesions, thrombosis or haemorrhage and, three months earlier, in the course of the hypertension evaluation, a 123I-MIBG scintigraphy scan also ruled out pheochromocytoma.
MINI REVIEW
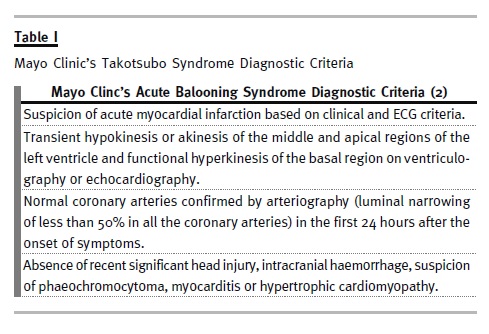
Several criteria have been proposed to diagnose TC. The most widely accepted diagnostic criteria are those of the Mayo Clinic2 (see Table 1), although several other diagnostic criteria have been also proposed such as the Abe and Kondo, Prasad, Kawai, and Segovia Cubero criteria2. However, there is still controversy over its validation as definitive takotsubo cardiomyopathy criteria2. Despite the differences among these classifications, all the patients share one common pattern – the absence of coronary artery obstructive lesions directly related to the RWMA.
Ibanez et al.14 studied the anterior left descendent coronary artery by intravascular ultrasound and found that all TC patients had instable plaques.
This could provide an explanation for its pathophysiology as a spontaneous plaque rupture and transient occlusion might be followed by an early reperfusion, precipitating myocardial stunning and RWMA. However, recent studies failed to prove this hypothesis15,16.
Abnormal catecholamine dynamics related to emotional distress seems to play a major role in the pathogenesis of takotsubo cardiomyopathy17. The massive release of hormones could induce myocardial stunning, direct cardiomyocyte injury and vasoconstriction through an increase in intracellular calcium via AMPc2. Pheochromocytoma, thyrotoxicosis and subarachnoid haemorrhage may mimic takotsubo cardiomyopathy, and all these conditions show an acute catecholamine increase. The consistent observation of this association in these distinct settings reinforces this theory.
One study showed that on hospital day 1 or 2, plasma levels of catecholamines (i.e., epinephrine, norepinephrine, and dopamine) among patients with TC were 2 to 3 times the values among patients with Killip class III myocardial infarction and 7 to 34 times published normal values18. Additionally, epinephrine (injection), post -emotional trauma and catecholamine-induced stress in animal models successfully reproduce the disease19. These findings thus suggest that a direct catecholamine toxicity might be a possible mechanism for the pathogenesis of takotsubo cardiomyopathy.
Despite the higher sympathetic nerve density in the basal regions it is the apical area that seems more vulnerable to mechanical dysfunction, which could be explained by the highest concentration of β adrenergic receptors in the apex. At low to moderate levels, epinephrine induces an inotropic positive response. At higher levels this positive effect is lost and a negative response overcomes since β2 adrenoreceptors converts the stimulatory Gs pathway to Gi (inhibitory), a mechanism known as stimulus trafficking20. At physiological levels norepinephrine exerts an inotropic and lusitropic effect on ventricular cardiomyocytes through a β2 -adrenoreceptor (β2AR) and β1-adrenoreceptor (β1AR) activation of Gs protein family. Thereafter, AMPc concentration increases and activates protein kinase A (PKA) and begins an activation of downstream intracellular targets resulting in a gain of the contractile response. However, at higher norepinephrine levels, a PKA –mediated β2AR phosphorylation, due to intense β2AR and β1AR stimulation, deviates the G stimulatory (Gs) protein intracellular activation to an inhibitory response resulting in loss of myocardial contractile response. It is thought that it would protect the cardiomyocytes from the pro-apoptotic effects of β1AR Gs stimuli. Since this myocardial responsiveness is more pronounced in the apex it would justify its ballooning.
Another hypothesis is the aborted myocardial infarction. However, this theory has few followers since blockage of one coronary vessel would hardly explain the multivessel affected area. Only a, very unlikely, simultaneous blockage of three epicardial coronary vessels would explain the apical and midventricular dysfunction. Besides, the extent of the RWMA does not correlate with the modest increase in the cardiac enzymes17. Another clue against an obstructive coronary aetiology is given by microscopy findings, which show contraction bands of necrosis, neutrophil infiltration and fibrosis, findings that differ from those of ischaemic origin21. The multivessel catecholaminergic spasm is a plausible explanation, as a quick recovery and good prognosis is usually observed.
The takotsubo cardiomyopathy is also related to a mechanism known as neurogenic myocardial stunning17. In the animal model brain stimulation (intracranial haemorrhage or stellated ganglia stimulation) induces ECG and myocardial motility abnormalities similar to takotsubo cardiomyopathy21.
Moreover, cardiac sympathectomy after brain death seems to prevent organ damage22. Neuronal reuptake (uptake -1), which might be impaired in these cases, is one important mechanism to cleanse the myocardial catecholamine neuronal bath. This vulnerability along the aminergic overload would then induce heart damage. This neuronal dysfunction might be related to the trigger which varies according to the literature. An emotional event is reported in 30 to 100% as opposed to the few 3% identified in ACS.
We do not know the role of oestrogens but it seems that they also play a protective role in TC since the typical patient is a postmenopausal Caucasian woman, 60 to 69 years old23,24. Lower levels of these hormones can increase angina pectoris episodes due to microvascular dysfunction25.
The clinical presentation of TC is very similar to that of ACS or even pulmonary embolism. The most common symptom is precordial pain (58.8%), followed by dyspnoea (30.0%)24. As for electrocardiographic changes, ST segment and T wave abnormalities are the most common. They have an incidence rate of 60% and 39.6% respectively, followed by prolonged QTc interval, which might be a predisposing factor for fatal cardiac arrhythmias24. RBBB and left bundle branch block have also been reported.
These findings may change through the evaluation, revealing the dynamic and transient features of this entity, as observed in our case.
Despite the previous features, the cornerstone of TC is the typical jar -like image of the left ventricle in ventriculography or the matching changes on echocardiogram without a correspondent coronary disease. On echocardiography, the apical and midventricular hypo, dys or akinesis and basal segments hypermotility are the most common findings, and the last one can hamper the prognosis by means of left ventricular outflow obstruction tract (LVOTO).
As previously shown, there are few cases of TC among the CKD population, despite the widely known high prevalence of CKD -associated sympathetic overactivity. In CKD, this overactivity has been directly demonstrated by muscle sympathetic nerve activity recordings26. Patients undergoing renal replacement therapy also show a similar pattern, although there is only indirect evidence for sympathetic overactivity in this setting: higher heart rate, blood pressure variability monitoring and changes in barorreflex function27. Indeed, it is believed that renal sympathetic nerve activation contributes to the pathogenesis of hypertension. The Proof -of -Concept came from several trials that tried to lower blood pressure in treatment-resistant hypertension through catheter-based renal denervation. Despite these theoretical considerations and background, there are very few published reports on TC among HD patients. However, it is of critical importance to distinguish between TC and ACS, because both treatment and prognosis are clearly distinct.
The TC outcome is usually good and the recurrence rate is low, although some complications may be anticipated. Cardiogenic shock due to LVOTO may worsen the prognosis, and is usually observed among patients with prior normal heart function. Apical thrombosis, ventricular arrhythmias and apical ventricular rupture are other complications that require an early diagnosis and timely approach. These complications account for an hospital mortality between 0% and 8%3,28-30.
There is no specific treatments for left ventricular failure in the setting of TC because cardiac function is normalized within a few weeks17. The focus of the treatment, besides LVOTO management, is mainly preventive and symptomatic. Current recommendations include modulation of heart innervation with cardioselective β2 -blockers, such as metoprolol or bisoprolol. Some authors rather use a β and β blocker simultaneously, as β-blockers alone can prolong the QT interval and leave unopposed the potentially adverse effects of high local concentrations of catecholamines at β-adrenoceptors17.
The use of intravenous inotropes should be reserved to unstable patients without significant outflow obstruction. The presence of LVOTO, even to a mild degree, contraindicates its use because of the risk of acute severe outflow obstruction and cardiogenic shock. The use of other intravascular devices, such as intra -aortic balloon pump, is to be evaluated individually.
Regarding takotsubo cardiomyopathy treatment, there is no place for thrombolytic therapy. Anticoagulation to prevent apical thrombosis is also debatable in spite of the existence of a procoagulant state within the ventricles (turbulent blood flow and stasis within the ventricles and increased activation of platelet β2-receptors). Despite this concern no recommendation has yet been made17.
CONCLUSION
Takotsubo cardiomyopathy is a rare clinical condition frequently precipitated by a stressful event, which affects mainly post-menopausal women. Unlike ACS, the prognosis is usually good. Early identification can prevent erroneous approaches and iatrogenic complications, such as the use of fibrinolytic therapy or the inadvertent use of inotropes.Despite being a clinical entity in which the proposed pathophysiological mechanism – sympathetic overdrive – is very common in CKD patients, it is infrequently reported in haemodialysis patients. It is not known whether TC is underdiagnosed in this population or whether, in fact, these patients may develop some protective mechanisms due to chronic sympathetic stimulation. Therefore, additional research in the CKD population is required to increase the understanding of the relative risk of takotsubo cardiomyopathy in this population.
References
1. Dote K, Sato H, Tateishi H, Uchida T, Ishihara M. [Myocardial stunning due to simultaneous multivessel coronary spasms: a review of 5 cases]. J Cardiol 1991;21(2):203–214. [ Links ]
2. Castillo Rivera AM, Ruiz -Bailen M, Rucabado Aguilar L. Takotsubo cardiomyopathy–a clinical review. Med Sci Monit 2011;17(6):RA135–147. [ Links ]
3. Tsuchihashi K, Ueshima K, Uchida T, et al. Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction. Angina Pectoris -Myocardial Infarction Investigations in Japan. J Am Coll Cardiol 2001;38(1):11–8. [ Links ]
4. Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako -Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J 2008;155(3):408–417. [ Links ]
5. Deshmukh A, Kumar G, Pant S, Rihal C, Murugiah K, Mehta JL. Prevalence of takotsubo cardiomyopathy in the United States. Am Heart J 2012;164(1):66–71. [ Links ]
6. Muratsu J, Morishima A, Ueda H, Hiraoka H, Sakaguchi K. Takotsubo cardiomyopathy in two patients without any cardiac symptom on maintenance hemodialysis. Case Rep Nephrol 2013;2013:640976. [ Links ]
7. Takemoto F, Chihara N, Sawa N, et al. Takotsubo cardiomyopathy in a patient undergoing hemodialysis. Kidney Int 2009;76(4):467. [ Links ]
8. Kusaba T, Sasaki H, Sakurada T, et al. [Takotsubo cardiomyopathy thought to be induced by MRSA meningitis and cervical epidural abscess in a maintenance-hemodialysis patient: case report]. Nihon Jinzo Gakkai Shi 2004;46(4):371–376. [ Links ]
9. Fukui M, Mori Y, Tsujimoto S, et al. Takotsubo cardiomyopathy in a maintenance hemodialysis patient. Ther Apher Dial. 2006;10(1):94–100. [ Links ]
10. Shin MJ, Rhee H, Kim IY, et al. Clinical features of patients with stress -induced cardiomyopathy associated with renal dysfunction: 7 case series in single center. BMC Nephrol 2013;14:213. [ Links ]
11. Musone D, Nicosia V, DAlessandro R, et al. [Acute heart failure secondary to takotsubo cardiomyopathy in a patient on peritoneal dialysis with residual renal function loss]. G Ital Nefrol 2012;29(4):467–772. [ Links ]
12. Hassan S, Hassan F, Hassan D, Hassan S, Hassan K. Takotsubo cardiomyopathy associated with peritonitis in peritoneal dialysis patient. Ren Fail 2011;33(9):904–907. [ Links ]
13. Fearnley RA, Gatward JJ, Gattas DJ. Iatrogenic hypercalcaemia including takotsubo cardiomyopathy in regional citrate anticoagulation for continuous venovenous haemodialysis. Anaesth Intensive Care 2014;42(4):520–521. [ Links ]
14. Ibanez B, Navarro F, Cordoba M, M -Alberca P, Farre J. Tako -tsubo transient left ventricular apical ballooning: is intravascular ultrasound the key to resolve the enigma? Heart 2005;91(1):102–104. [ Links ]
15. Haghi D, Roehm S, Hamm K, et al. Takotsubo cardiomyopathy is not due to plaque rupture: an intravascular ultrasound study. Clin Cardiol 2010;33(5):307–310. [ Links ]
16. Hoyt J, Lerman A, Lennon RJ, Rihal CS, Prasad A. Left anterior descending artery length and coronary atherosclerosis in apical ballooning syndrome (Takotsubo/stress induced cardiomyopathy). Int J Cardiol 2010;145(1):112–115. [ Links ]
17. Akashi YJ, Goldstein DS, Barbaro G, Ueyama T. Takotsubo cardiomyopathy: a new form of acute, reversible heart failure. Circulation 2008;118(25):2754–2762. [ Links ]
18. Wittstein IS, Thiemann DR, Lima JAC, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med 2005;352(6):539–548. [ Links ]
19. Suzuki H, Matsumoto Y, Kaneta T, et al. Evidence for brain activation in patients with takotsubo cardiomyopathy. Circ J 2014;78(1):256–258. [ Links ]
20. Lyon AR, Rees PS, Prasad S, Poole -Wilson PA, Harding SE. Stress (Takotsubo) cardiomyopathy–a novel pathophysiological hypothesis to explain catecholamine-induced acute myocardial stunning. Nat Clin Pract Cardiovasc Med 2008;5(1):22–29. [ Links ]
21. Shams Y -S. Insights into the pathogenesis of takotsubo syndrome, which with persuasive reasons should be regarded as an acute cardiac sympathetic disease entity. ISRN Cardiol 2012;2012:e593735. [ Links ]
22. Novitzky D, Wicomb WN, Cooper DK, Rose AG, Reichart B. Prevention of myocardial injury during brain death by total cardiac sympathectomy in the Chacma baboon. Ann Thorac Surg 1986;41(5):520–524. [ Links ]
23. Bellandi B, Salvadori C, Parodi G, et al. [Epidemiology of Tako -tsubo cardiomyopathy: the Tuscany Registry for Tako-tsubo Cardiomyopathy ]. G Ital Cardiol (Rome) 2012;13(1):59–66. [ Links ]
24. Sanchez -Jimenez EF. Initial clinical presentation of Takotsubo cardiomyopathy with-a focus on electrocardiographic changes: A literature review of cases. World J Cardiol 2013;5(7):228–241. [ Links ]
25. Eshtehardi P, Koestner SC, Adorjan P, et al. Transient apical ballooning syndrome–clinical characteristics, ballooning pattern, and long -term follow -up in a Swiss population. Int J Cardiol 2009;135(3):370–375. [ Links ]
26. Rubinger D, Backenroth R, Sapoznikov D. Sympathetic activation and baroreflex function during intradialytic hypertensive episodes. PLoS One 2012;7(5):e36943. [ Links ]
27. Rubinger D, Backenroth R, Sapoznikov D. Sympathetic nervous system function and dysfunction in chronic hemodialysis patients. Semin Dial 2013;26(3):333–343. [ Links ]
28. Kurisu S, Sato H, Kawagoe T, et al. Tako-tsubo -like left ventricular dysfunction with ST-segment elevation: a novel cardiac syndrome mimicking acute myocardial infarction. Am Heart J 2002;143(3):448–455. [ Links ]
29. Desmet WJ, Adriaenssens BF, Dens JA. Apical ballooning of the left ventricle: first series in white patients. Heart 2003;89(9):1027–1031. [ Links ]
30. Brinjikji W, El-Sayed AM, Salka S. In-hospital mortality among patients with takotsubo cardiomyopathy: a study of the National Inpatient Sample 2008 to 2009. Am Heart J 2012;164(2):215–221. [ Links ]
Joao Carlos Sousa Torres
Hospital de Santa Cruz
Avenida Prof. Reinaldo dos Santos
2790 -134 Carnaxide, Portugal
Tel.: (351) 917546609
Email: joaosousatorres@gmail.com
Conflicts of Interest: None declared.
Received for publication: 26/10/2015
Accepted in revised form: 13/12/2015














