Introduction
A bowel elimination stoma is the exteriorization of a part of the intestine through the abdominal wall, constructed from intestine’s mucosal lining, to create an artificial outlet for the fecal contents. Colostomies and ileostomies are named based on the part of the intestine that is brought to the skin's surface. (Di Gesaro, 2012).
The indication for the construction of a stoma occurs in several pathologies, namely oncological diseases, inflammatory bowel disease, neurological problems, urological disease, traumatic injury, and diverticulitis (Rivet, 2019).
Colorectal cancer is the most likely diagnosis for constructing a bowel elimination stoma (Silva et al., 2020). In 10% of cases, this results in a permanent stoma (Vonk-Klaassen et al., 2016), and in the case of temporary stomas, these remain for two to four months (Kuryba et al., 2016).
Building a stoma can have positive repercussions, such as reduced symptoms and improved quality of life. According to Cengiz et al. (2020), stoma care has a largely negative impact on physical, psychological, and social aspects of people's lives. This poses a potential threat to all aspects of their lives. It is not just about managing stoma care but also incorporating it into their daily routines, as highlighted by Sousa et al. (2015). The adaptation to the presence of a stoma involves apprehension and suffering, causing changes in the body, image, self-esteem, confidence, and autonomy, causing changes in social relationships, in the way of dressing, eating, sexuality, and work (Ayaz-Alkaya, 2019; O’Connor, 2005).
Having a stoma can be challenging, and many people who have undergone stoma construction experience various complications over the course of their lives. These complications can make it harder for the person to take care of their stoma, and can lead to psychosocial issues, increased morbidity, and higher healthcare costs (Colwell et al., 2018; Sung et al., 2010), lower perceived quality of life, social isolation, prolonged hospital stays, increased use of primary health care (Parmar et al., 2011) and more follow-up appointments (Whiteley and Sinclair, 2010).
The peristomal skin complications are dermatitis, erythema, ulcer, and granuloma. Stoma complications are malposition (requiring at least one accessory to maintain effluent collection for 24 hours), retraction (stoma lumen below skin level), mucocutaneous dehiscence, necrosis, peristomal hernia, prolapse, stenosis, stoma mucositis, fistula, hemorrhage, and ischemia.
There are several factors associated with the development of stoma and peristomal skin complications, namely clinical and treatment factors, of which the position and location of the stoma and the lack of preoperative marking of the stoma site are the factors most often mentioned in the literature (Pinto et al., 2017).
The experience of this event is influenced by various factors, including one's ability to care for their stoma. (Simmons et al., 2007), the development of complications associated with the stoma (Pittman et al., 2009), and psychological support and social support from family and significant others (Piwonka and Merino, 1999).
Patients who receive stoma site marking and perioperative education from a nurse experience less anxiety (Millan et al., 2010), have significantly better quality of life, better confidence and independence in stoma care, and lower rates of postoperative complications regardless of stoma type (Person et al., 2012).
Stoma site marking is a crucial nursing intervention that should be performed on all patients who are scheduled to have a stoma or undergo unplanned abdominal surgery with a risk of complications that may require a stoma. This is due to the significance of stoma site marking in ensuring the well-being of the patients. From the conceptual point of view, stoma marking emerges as an intervention that promotes awareness of the transition to life with a stoma, allowing patients first to perceive their likely new condition. Thus, stoma marking emerges as a preventive intervention that promotes a healthy transition to the new condition (Soares-Pinto et al., 2022).
Marking the stoma site preoperatively increases the likelihood of patient independence in stoma self-care, is associated with fewer persistent leaks and greater durability of the collecting systems, and earlier resumption of activities of daily living (Salvadalena et al., 2015).
In Portugal, stoma therapy nurses are the most suitable professionals to perform the marking of the stoma site since it is a competence acquired in their training process and developed in the clinical context ( Directorate General of Health, 2017). However, these providers are not always available, especially in emergency situations, and it is essential to train other nurses capable of marking the stoma site (Salvadalena et al., 2015).
Currently, in a hospital in the northern region of Portugal, a nurse’s appointment rate at the stoma site is 100% concerning scheduled surgery. The marking is performed by a stoma care nurse, who usually has a weekly daytime schedule. In this health institution, only six nurses have differentiated training to perform stoma marking: four in the surgical inpatient services and two in the medical department. Regarding the construction of the stoma in the context of unscheduled surgery, the rate of stoma marking is residual, and there is no concrete data to characterize the situation. There is no formalized procedure for marking the stoma site in emergencies. The evidence points to the importance and impact of stoma marking, which a stoma care nurse should preferably perform, but in their absence, it should be performed by someone with the knowledge to do so (Salvadalena et al., 2015; Zwiep et al., 2022).
Therefore, and aware of the importance of the implementation of quality systems, as assumed by organizations such as the World Health Organization and the International Council of Nurses, and the Portuguese OE, it is urgent to implement strategies for continuous quality improvement of nursing care in this area, based on the methodology for continuous quality improvement in nursing care proposed by the Portuguese OE. The implementation of these projects has already led to evidence-based practices and positive changes within nursing teams (Oliveira et al., 2023).
Thus, acknowledging the importance and need for the systematization of stoma site marking practice in patients undergoing unscheduled abdominal surgery, the project’s main objective is to increase by 50% the marking rate of intestinal elimination stomas in patients undergoing emergency surgery, by December 31, 2024.
The objective responds to the Portuguese Nursing Care Quality Standards, precisely the standard concerning the organization of nursing care: “In the permanent search for excellence in professional practice, the nurse contributes to the maximum effectiveness in the organization of nursing care" (Ordem dos Enfermeiros, 2001, p. 14).
1. Methods
This best practice implementation project will use the cycle PDCA, P (plan), D (do), C (check) and A (act/adjust), developed by Shewhart and later expanded into quality control by Dr Deming in the United States (Qiu and Du, 2021) and reported according to SQUIRE (Ogrinc et al., 2016). The PDCA is cyclical process is followed in this approach for improving nursing practice. It involves four phases, which are assessment, planning, implementing interventions, and re-assessment. The process begins by identifying the problem, followed by understanding the problem and its causes, and defining specific objectives. Next, an intervention is defined, planned, and implemented. Finally, results are verified, corrective measures are proposed, and the team is standardized and trained..
Nursing units and teams in Portugal are dedicated to implementing a methodology of continuous quality improvement in nursing care. Critical analysis and review of clinical practices are integrated into the training and unit meetings. Any issues or problems are considered as opportunities to improve the practice. The first assumption for the development and implementation of the Portuguese OE framework for quality improvement projects is that the resolution of this problem or need experienced by patients is within the scope of nurses' competencies to solve or respond to.
Context
This project will be developed with the nursing teams from the Emergency Department and the Colorectal Surgical Unit from a hospital in the northern region of Portugal, considering that it is the unit that receives patients from the Emergency Department submited to unplanned surgery.
Phase one - Identify the problem
Based on a problem identified in this specific context of the nurses' clinical practice - the Colorectal Surgical Unit - the nursing team felt the need to find strategies to solve it in the context of their clinical practice. During 2022, the team conducted brainstorming and discussions to address the issue. They defined the project's main objective and organized a group to develop and implement it. This group is composed of the four stoma care nurses from the Colorectal Surgical Unit who are responsible for coordinating and operationalizing the following phases during the next two years (2023 and 2024).
Phase two - Understand the problem and the causes and define the specific objectives
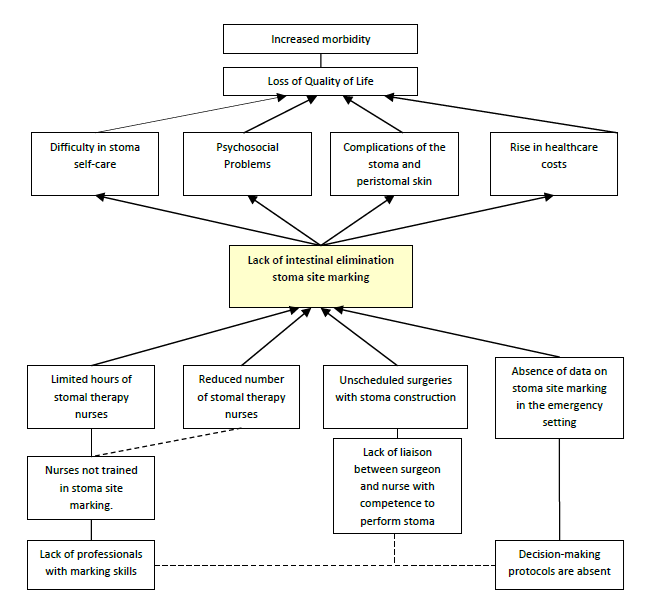
After identifying problems and brainstorming with the nursing team, a Problem Tree (Figure 1) was created to determine priority intervention areas. This problem tree served as guidance to define specific objectives: 1) identify training needs on stoma site marking for nurses in colorectal surgery and emergency department by June 30, 2023; 2) develop training for nurses in colorectal surgery and emergency department in response to identified needs by the end of 2023; 3) develop decision-making algorithm for stoma site marking by December 2023; implement algorithm from April 1, 2024; 4) evaluate correct stoma site marking (audit) quarterly by December 31, 2024.
Phase three - Define, plan and implement the intervention
Starting from the objectives defined in the previous phase, the working group designed a set of interventions in response to each of these objectives (Table 1). As part of the intervention planning process, it's important to have a communication plan. Strategic communication is crucial in ensuring that communication aligns with the organization's goals. Communication planning helps in identifying strategies, forecasting, and predicting the possible stakeholder behavior in response to the organization's decisions. In this way, the communication plan goes beyond the disclosure of the project and the results obtained, being transversal to all of its stages.
During the project's development, various forms of communication will be utilized based on the hierarchy, assertiveness, and effectiveness of the receiver. In particular, the communication plan has strategic interventions and contemplates the diffusion through the internal communication channels of the hospital, aiming at communicating with all the medical and nursing teams. Chronologically, the communication plan begins after project approval: 1) Communication channel - creation of an email address and microsite with relevant information about the development of the project; 2) Meeting plans - scheduling of meetings and key activities of the project; 3) Invitations - official invitation to the recipients to participate in activities; 4) Schedules - contacts via email and indirect communication through the hospital’s communication channels; 5) Logo - creation of an image for the project; 6) Sharing of the project in scientific events (project and/or results) and publication of a scientific article (project and/or results).
Establishing appropriate communication channels and identifying key stakeholders is crucial for successful communication. The relevant aspects to be integrated in the internal and external communication plan involve the services surrounding the project and the rest of the institution.
Clear communication is essential to implement several activities, including identifying training needs, and disseminating training and the nurse's decision support procedure. Raising awareness about the importance of correct stoma marking during unscheduled surgeries will be a key focus of this initiative. The results will be disseminated to involve professionals from different services.
Table 1 Design and planning of interventions.
| Specific objective | Strategy | Target | Methods Used to Measure Compliance with the objective |
|---|---|---|---|
| Identify training needs | Identification of training needs on stoma site marking in articulation with the nurse managers of the services involved in the project | Colorectal Surgery Service Nurses and nurses from the Emergency Department | Questionnaire applied to all nurses |
| Develop training activities | Training program for correct stoma site marking, with theoretical training and simulation of stoma site marking on a mannequin | At least 25% of nurses from each team (to ensure that in each shift a nurse with training is present) | Questionnaire applied to nurses participating in the training program and practice assessment |
| Develop decision-making algorithm | Development of a procedure with a decision algorithm for stoma site marking, based on the best available evidence and appropriate to the context of clinical practice | Nursing staff from both services and surgical medical team | Algorithm approved by the nurse managers and clinical directors of the services |
| Audit | Checking that the stoma site is marked correctly in patients undergoing unscheduled surgery | Patients with stoma resulting of unscheduled surgery | Documentation in the patients' clinical file and checklist for stoma site marking verification (to be developed based on the decision-making process algorithm) |
Phase four - Verify the results, propose improvement measures, standardize and train the team
In this phase, the proportion of patients with correct stoma marking proposed for unscheduled surgery will be the indicator to assess the success of the intervention. Other indicators will also be considered for the identification of corrective measures: the success of training, the proportion of trained nurses per shift, and the rate of compliance with the decision-making algorithm. The quarterly evaluation will allow for timely corrective measures and close project monitoring.
To guarantee consistency in patient care, specialized nurses with recognized expertise in stomal therapy will provide and evaluate training for optimal professional preparation. During the implementation phase of the decision-making algorithm, on weekday shifts, the stomal therapist nurses of the working group will accompany the nurses integrated in the project in the stoma appointment, both in the emergency department and in the inpatient unit, in a mentoring format.
The institution's document management software should have procedures and decision algorithms readily available and easily accessible to ensure efficient information retrieval. The decision-making algorithms used in these services will remind healthcare professionals to identify patients who require stoma marking.
2. Results
It is expected to increase by 50% the rate of preoperative marking of intestinal elimination stomas in clients undergoing emergency surgeries until December 31, 2024.
Improving the quality of nursing care is crucial, particularly when it comes to caring for patients with a stoma. Trained nurses who properly mark stomas can significantly reduce the occurrence of stoma and peri-stoma skin-related complications, leading to increased confidence and independence in self-care, faster recovery, and an earlier return to daily activities. Promoting awareness of the transition to life with a stoma can be anticipated through preoperative stoma marking and is associated with a more fluid and positive adaptation to this condition. The benefits of self-care include reducing health costs by preventing complications and promoting autonomy, thereby reducing hospital readmissions and primary health care contacts.
Conclusion
A high level of engagement with quality improvement projects is expected from nurses to ensure the success of such projects. Success depends not only on the drivers of the project, but above all, on their ability to involve everyone during all phases. Continuous quality improvement should be understood as teamwork, whose main objective is to provide the best nursing care, supported by the best evidence, within a philosophy that nursing practice should follow the evolution of knowledge. Results from this project may offer new strategies to cope with management shortcoming in health systems in this domain.
Currently, nursing and health care exposes individuals to a significant turnover of care providers. Ensuring equity in quality of care, care standardization and care systematization emerge as an ethical and deontological duty of the nursing profession.
The successful implementation of this project can improve the quality of life of people with stoma and increase satisfaction with health care. In addition, the results of this work may reinforce the importance of its replication in other clinical settings, contributing to the improvement of the quality of care for people with stoma.