Introduction
Light induced amaurosis (LIA) is defined as a transient monocular or binocular visual loss triggered by exposition to bright lights during a certain period that may vary between episodes.1 It has also been linked with retro-orbital pain.2LIA is a rare and frequently unrecognized presentation of symptomatic severe internal carotid artery (ICA) stenosis3) and rare type of ocular ischemic syndrome (OIS).4),(5
The aim of this report is to present a case of light-induced amaurosis and its management.
Case report
We report a case of a 74-year-old Portuguese Caucasian man who presented with a 6-month history of transient monocular blindness of his left eye. He described blurry “white out” episodes when exposed to bright lights in dark environments. The episodes were self-limited, lasted for several minutes and had no other inciting event. His vision was reportedly good between episodes, there were no other focal neurological deficits reported and he had no history of stroke or transient ischemic attack (TIA). The patient also complained of headache and dizziness associated with the LIA episodes. Physical examination revelled bilateral carotid bruits with no other relevant finding.
Past medical history included peripheral artery disease, for which he had already been referred to a vascular surgical outpatient clinic and followed since 2012, chronic heart failure class II of New York Heart Association (NYHA) based on an ischemic and valvular heart disease, hypertension, dyslipidaemia, and permanent atrial fibrillation. He was a heavy former smoker, with a 50 pack-year history until the age of 59. Chronic medical therapy included full dose anticoagulation with rivaroxaban, antiplatelet therapy with acetylsalicylic acid, atorvastatin, beta-blocker, and angiotensin receptor blocker.
Carotid doppler ultrasonography suggested significant stenosis of the left common carotid artery (CCA). Internal carotid arteries were difficult to visualise due to intense calcification causing significant acoustic shadowing.
A computed tomography angiogram of the head and neck was performed revelling a significant morphologic stenosis of the left common carotid artery, left internal carotid artery with sub occlusive disease and right internal carotid artery stenosis estimated at 70-75%, both calculated with the North American Symptomatic Carotid Endarterectomy Trial (NASCET) method (Figure 1, A and B). The vertebral arteries study did not reveal significant morphologic disease and circle of Willis was patent.
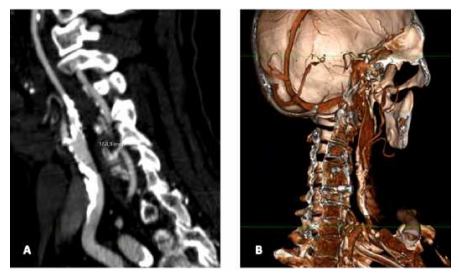
Figure 1 Pre-operative computed tomography angiogram. A - stenosis of the left common and internal carotid artery (longitudinal section); B - Volume rendering reconstruction of left carotid bifurcation (internal projection).
LIA was suspected and the patient was submitted to left common and internal carotid artery endarterectomy with a Dacron patch angioplasty (Figure 2). A circumferential calcified heterogeneous coralliform plaque was found.
Left common and internal carotid artery endarterectomy with a Dacron patch angioplasty.
He was discharged home two days later, with no focal neurologic deficits. In the first month after surgery, the symptomatology was reduced but still present. The dizziness and headache were completely gone. After three months of follow-up the symptoms were less frequent, but occasional weekly LIA episodes were still referred.
discussion
LIA is a rare presentation of ICA stenosis. It is thought to be caused by an impairment in regeneration of the retinal visual pigments that result from degenerative changes on the retina due to chronic ischemia.5 As showed in the present case, patients complain of blurry “white out” episodes.
Amaurosis fugax (AF) is a well-known clinical entity. It is typically defined as transient monocular visual loss and is frequently associated with vascular thromboembolic events arising from the internal carotid artery. Patients classically describe a "curtain coming down” in their visual field or as a generalized darkening or shadow. It is usually painless, and it is not usually trigger related. AF is also a type of OIS presentation but is unrelated to light exposure.
LIA is thought to have a hemodynamic cause, related to hypoperfusion of the retinal vessels.6 As a symptom, LIA might express the inability of internal carotid circulation to sustain the increased retinal metabolic activity occurring when the retina is exposed to bright lights in dark environments.7
Differential diagnoses of LIA also include hemeralopia and photophobia. Hemeralopia, often called “day-blindness”, is the inability to see in bright environments as clear as in dim light.8 Photophobia is abnormal light intolerance.9 These two conditions are commonly associated with cone dystrophies and should be distinguished from LIA.
Lack of knowledge about LIA can lead to misdiagnosis, under recognition and possibly leaving patients untreated, increasing the relevance of publicizing this entity.6 The episodes are unpredictable and do not occur every time a patient is exposed to bright lights.7 Carotid artery endarterectomy was previously documented as a successful way to treat LIA in patients with severe vessel disease like the presented.10
In conclusion, when evaluating complains of vision loss after bright light exposure, clinicians should be aware that this symptomatology might be linked to severe carotid artery occlusive disease. It is our intention with this report to raise awareness for this presentation to increase its recognition, necessary for timely surgical intervention.
















