Introduction
Dr. Miguel Guimarães, the former President of the Portuguese Medical Association, argued that the doctor-patient relationship should be recognized as an intangible heritage by UNESCO for it is the foundation of medical practice.1 Doctor-patient relationship relies on the doctor’s knowledge of how to assess and decide what to do in each situation, emotional intelligence, and the patient’s trust that the proposed treatment/course of action is in its best interest. (2-3
Even nowadays a more significant role is commonly attributed to the doctor, while the patient is considered the most passive and fragile element in the clinical appointment. (4 However, the incremental process of shared decision-making has been shown to improve affective-cognitive outcomes, with Rappley advising the doctor-patient relationship as a distributed relational entity, as opposed to a single, isolated encounter. (5 This will strengthen the bond, promoting the patient’s intervention and autonomy. Additionally, a good doctor-patient relationship decreases the likelihood of regretting any decisions, encourages a more active role in the treatment, and leads to a successful clinical practice. (6-7 Hughes et al proved, by assessing the patient’s rating of shared decision-making and then examining data from the Medical Expenditure Panel Survey (MEPS), how essential shared-decision making can be and how strongly it can affect the patient.8 MEPS was based on patient-reported physical and mental health ratings, prescription drug usage (statins/HMG-COA reductase inhibitors), use of health services (such as emergency room visits), and healthcare spending. (8
Studies have shown that prioritizing patient-centered care and communication by engaging the patients in the conversation, using open-ended questions, not interrupting, and understanding their concerns and expectations, improves their well-being and overall health outcomes. (9-10 Emotional clarity and emotional repair in a fully informed patient, are strongly correlated with treatment adherence, which increases by 19% when there is good communication with the physician, proving the importance of psychological education. (11-12
Efforts are being made to include the teaching of communication skills in the university curriculum of the Integrated Master’s Degree in Medicine. (13 Abilities such as emotional intelligence and empathy, exemplified by perceiving the other’s feelings, comprehending emotions, and performing actions that show understanding, are linked to higher-quality care and therefore should also be part of the medical curriculum for all students. (14-16
Street et al. proved that patients were more pleased with the medical assistance and more willing to follow treatment recommendations when there was a more in-depth mutual understanding of the treatment goals and benefits. (17 Other researchers in the United States of America, have established that atherosclerotic cardiovascular disease patients who feel enlightened, empowered, and respected by their health providers have better adherence to the standard care treatment regimens, namely statins and aspirin. (18
Suboptimal communication has been associated with lower physical and mental health rates that lead to a higher percentage of visits to the emergency department, particularly in aging adults with more than five chronic conditions. (19 Studies indicate that the doctor-patient relationship in these cases is significantly lower in quality, therefore not fulfilling the patient’s needs. (20 In oncologic patients, communication substantially impacts the diagnostic stage, especially when delivering bad news, many patients show low expectations regarding the contact with the medical team responsible for their follow-up, even though admitting how crucial it could be. (21
If doctors used a method based on patients’ values and priorities, it would be easier to motivate patients to engage in the treatment plan, with positive results. (22
Patients’ principles are seldom reflected in the cardiovascular clinical guidelines (NOCs) released in Portugal between 2011 and 2013, 75% of these NOCs revealed no suggestion related to the inclusion of patients’ ideas, concerns, and expectations, therefore compromising patient-centered care, and possibly lowering the medical process’s quality. (23
Evaluating the possible correlation between the doctor-patient relationship and the patient’s enablement after the doctor’s appointment is important since it has been shown to affect patient outcomes. (24-25 Portuguese studies establish that patients tend to feel more enabled after a patient-centered doctor’s appointment. (24-25 However, there is still no evidence on how the patient-doctor relationship can affect it.
The Patient-Doctor Depth of Relationship (PDDR) is a scale specifically designed to measure doctor-patient relationship but not yet adapted or validated for European-spoken Portuguese. (26 This study aimed to perform its cross-cultural adaptation and convergent validity, with the enablement PDDR can bring about.
Methods
The PDDR’s cross-cultural adaptation to European-spoken Portuguese began after the author’s authorization and the Ethics Committee’s consent. The USF Coimbra Sul coordinator’s agreement was also granted.
It consisted of translating the survey, followed by linguistic verification and reverse translation.
Two current healthcare professionals, unconnected to the study and who were both native in English and European Portuguese, analysed and translated the PDDR scale from its English original form to European Portuguese.
The translation was then examined by a group of experts, whose native languages were both English and European Portuguese. After analysing the translation to the targeted population, the panel selected the most accurate and suitable translation for each topic, with the least word length and number of words per sentence as criteria, according to the English sense of each sentence.
Once the translation and the linguistic verification were completed, the reverse translation was performed with the distribution of the PDDR questionnaire to other two translators who were not related to the research and were both fluent in English and European Portuguese. No significant differences were identified between this last translation and the original PDDR questionnaire, by the investigation team.
Then and for credibility and assurance of future work’s quality, the PDDR was handed out to 15 conveniently chosen patients who had a scheduled family medicine/general practice doctor’s appointment, during the Fall of 2022, at the Unidade de Saúde Familiar (USF) Infante D. Henrique, in Viseu, Central Portugal. This allowed the PDDR’s internal consistency and reliability ascertainment and the identification of any doubts or criticism the patients might have had, concluding this step.
The Portuguese-adapted version of the PDDR and the Patient Enablement Instrument (PEI), which had previously been validated, to study enablement after consultation, with the Portuguese community and had already been implemented, were then part of the cross. (26-27
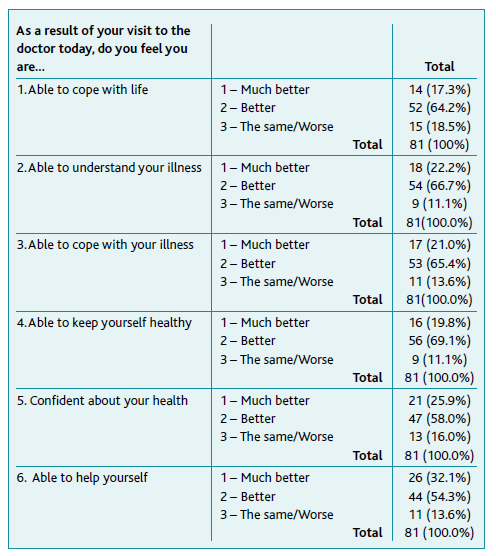
The PDDR is an eight-item scale, completed by the patient. Each item is attributed a score from 1 to 5 (1 - Disagree; 2 - Neither agree nor disagree; 3 - Slightly agree; 4 - Mostly agree; 5 - Completely agree). Using this distribution, a single overall depth of relationship score can be calculated, which ranges from 8 (no patient-doctor relationship) to 40 (very strong/deep patient-doctor relationship). The PEI questionnaire is a six-questions one with three possible choice answers: 1 - Much better; 2 - Better; 3 - The same/Worse. The total final score can extend from 6 (feeling much better than before the consultation) to 18 (feeling the same/worse than before the consultation).
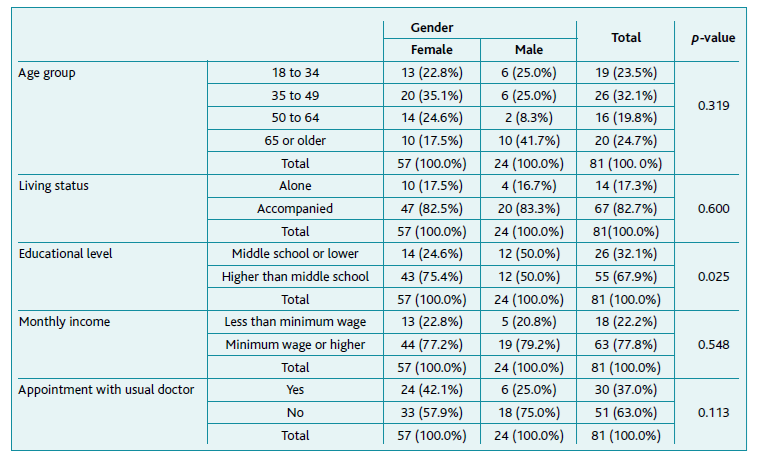
To understand the context of the sample population, gender, age group (18 to 34, 35 to 49, 50 to 64, 65 or older), living status (alone or accompanied), educational level (illiterate, primary school, middle school, high school, or college education), monthly income compared to the minimum national wage (less or equal or more) and whether or not the patient had an appointment with the usual doctor, were gathered.
The Socioeconomic Deprivation Index (SEDI) of the sample population was calculated by attributing a score based on: the living status (alone - 1 point; accompanied - 2 points); educational level (illiterate - 1; primary school - 1; middle school - 1; high school - 2; college education - 2); and monthly income (less than minimum wage - 1; minimum wage or higher - 2), being that the total score ranged from 3 to 6.
The number of questions in the surveys determined the sample size. Since PDDR has 8, a sample of a minimum of 81 participant persons, according to Trust Scale Length, was determined. (28-29
A random distribution of the inquiring days in January and February 2023, was performed, with patients being invited in convenience on each day, due to consultation length and some non-attendance of pre-scheduled consultations. The two questionnaires and the context questions were self-filled-in, at USF Coimbra Sul (located in Coimbra, Portugal), after their family medicine/general practice consultation. Patients who agreed to collaborate in the study should be able to read/hear the explanation about the study before expressing written consent to participate.
The investigator was in the same room as the patients, available to answer any questions or doubts, always ensuring the patients’ privacy, was properly identified, and stated no liaison with the USF Coimbra Sul. The chosen room was far from the doctors’ offices and doctors at work, who were not aware that the study was going on.
In Portugal, general practice/family medicine health units in the National Health Service can be UCSP, the Personalised Health Care Unit, and the Family Health Unit model A or model B, depending on a crescent level of autonomy.
Descriptive and inferential statistics, using the Statistical Package for the Social Sciences (SPSS) 27th version software, were applied. The normality of the numerical variables’ distribution was studied by the Kolmogorov-Smirnov test with the Lilliefors correction. Non-parametric tests were used for ordinal and non-normal distributed variables. Fisher’s exact test was performed for nominal variables. Correlational tests were also applied.
Results
After the translation, linguistic verification, and reverse translation tasks, 15 patients completed the PDDR Portuguese version. Of this sample 60.0% were female, 20.0% were 65 years of age or older and 93.3% had had an appointment with the usual doctor. Patients were pleased with the questionnaire’s layout and found the items were easy to understand and answer. There was no need to adjust the Portuguese PDDR questionnaire.
The validation study’s sample was n=81 patients, 70.4% (n=57) women.
According to Table 1, there was a significant difference between gender and educational level (p=0.025), with female participants showing a higher level of education. No other significant differences were found for the context variables.
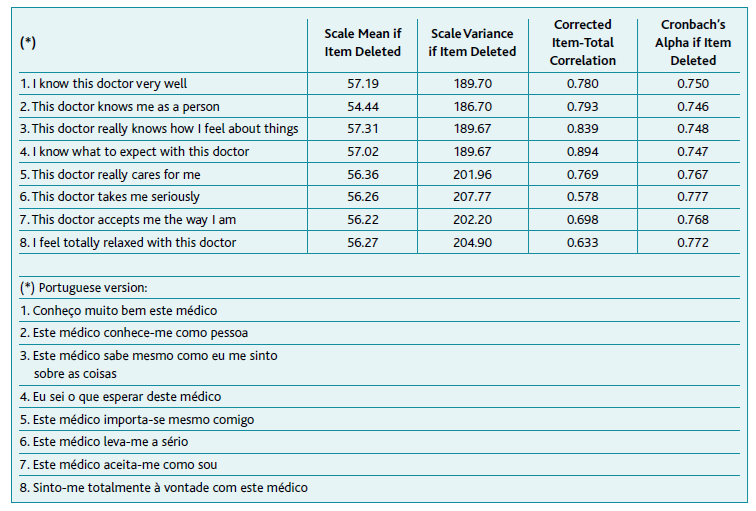
The internal consistency was tested using Cronbach’s α was of 0.785. The item-total statistic showed that Cronbach’s α was lower than 0.785 when any of the items of the PDDR were deleted according to Table 2.
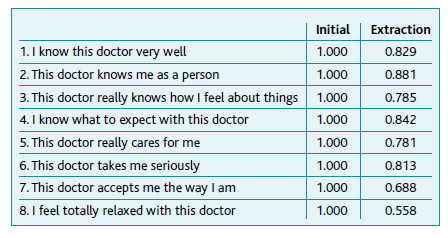
The average measured intraclass correlation coefficient was 0.785 (F (80,640) = 4.660, p<0.001). The factorial structure of the PDDR questionnaire revealed Kaiser-Meyer-Olkin (KMO) of 0.879 and Bartlett’s test of Sphericity, p<0.001. Item communalities varied from 0.558 for the eighth item to 0.881 for the second item, yielding moderate to high communalities (Table 3). One single factor explained 61.91% of the total variance, using the principal component analysis.
Regarding the PEI questionnaire, the calculated value of Cronbach’s α was 0.805. The item-total statistic showed that Cronbach’s α was lower than 0.805 when any of the items of the PEI were deleted. The average measure intraclass correlation coefficient was 0.805 (F (80,480)=5.127, p<0.001).
The frequency distribution of PDDR scores for each of its eight items is shown in Table 4, with 59.3% (n=48) of the sample feel accepted and 55.6% (n=45) relaxed with their doctor. For 19.8% (n=16) of the participants, the doctor knew how they “felt about things”. The mean total score of the PDDR questionnaire was 30.3±7.5 [8 to 40].
The frequency distribution of PEI scores for each of the six items is described in Table 5. For all six questions, most of the patients responded “better” (Table 5). The mean total score of the PEI questionnaire was 11.5±3.0 [6 (better) to 18 (worst)].
The Kolmogorov-Smirnov test with the Lilliefors correction revealed that the PDDR, SEDI, and PEI total scores did not follow a normal numeric distribution (p<0.001). Therefore, non-parametric statistics were used, namely Mann-Whitney U, Kruskal-Wallis, and Spearman correlation.
When studying the PDDR total scores according to the context variables no significant differences among the group medians were found (p>0.05, Mann-Whitney U test), the same happening for the age group (p>0.05, Kruskal-Wallis test). However, when grouping PDDR total scores based on whe-ther the appointment had been with the usual doctor or not, the group medians were significantly different: 35 [8 to 40] vs 23 [8 to 40] (p<0.001, Mann-Whitney U test).
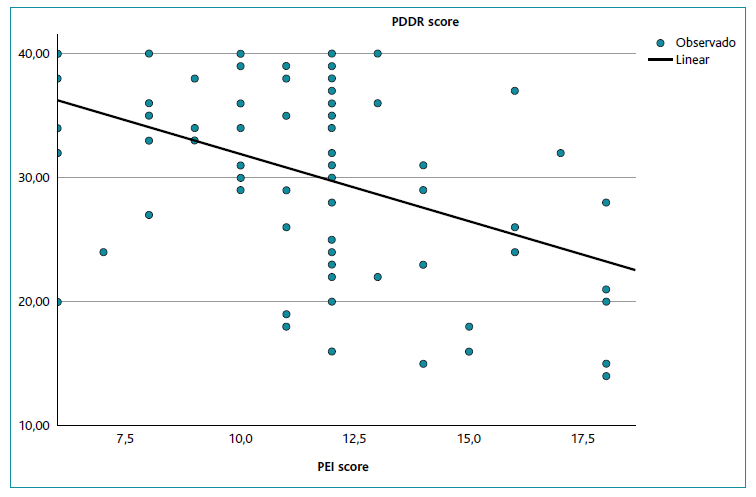
Spearman’s correlation between the PDDR total score and the SEDI score was weak positive non-significant, ρ=0.300, p=0.790, and with PEI total score was weak negative and significant ρ=-0.396, p<0.001. Figure 1 shows the estimated curve between PDDR and PEI scores.
Discussion
This study intended to cross-culturally adapt to the European-spoken Portuguese a questionnaire the au-thors deemed necessary. Portuguese studies have already reflected on the issue of seeking to understand the patient’s needs, perceiving the importance of the “social roles played by the actors of a clinical ga-thering and recognizing the importance of non-verbal communication the context of ambiguity and uncertainty of the patient’s hidden information”. (30-31
Care must be taken for some aspects in consultation like “well-groomed appearance, the use of a white-coat, the use of simple language, the mastering the Portuguese language, the punctuality, the giving out of information in writing, the sharing of all information, the continuity of care throughout time and in different types of care”. (32
Communication also affects the GP/FM, preventing its stress when it is well performed, so needing to play a key role in consultation that must be learned, trained, and practiced in the pre-and post-graduate settings. (33-35
Training communications is of paramount importance for it has been discovered that chatbot answers are perceived as more empathic than human ones. It is posted that this could be advantageous in preparing the doctor’s drafts. (36
So, many factors can influence the result of a clinical encounter, but no study measuring the phenomenon of the patient-doctor relationship has yet been made with a validated scale in Portugal. (37-38
In this study, the Portuguese version’s internal consistency of the PDDR questionnaire was good, with a Cronbach’s α of 0.785 meaning that the eight items of the survey produce similar scores. The item-total statistics of the PDDR questionnaire showed high reliability and the intraclass correlation coefficient of 0.785 (0.75<ICC<0.90) showed high reliability as well.
The KMO value over 0.5 (KMO value=0.879) and Bartlett’s test <0.05 (Bartlett’s test<0.001) suggest there is a substantial correlation in the data. Item communalities varied from 0.558 to 0.881, representing moderate to high communalities, the extracted factors accounting for a substantial proportion of the variable’s variance. One factor represented 61.91% of the total variance.
The study’s sample population was fully retrieved from one Primary Care Health Unit, the USF Coimbra Sul. Even though its composition seems to be consistent with the average Portuguese population distribution and with the fact that more female (70.4%) than male (29.6%) patients attend doctor’s appointments in a health center of the Portuguese National Health Service. (39
Patients were studied according to gender and five different context characteristics no significant differences by age group (p=0.319), living status (p=0.600), monthly income (p=0.548), or whether the appointment was with the usual doctor (p=0.113) being found. However, there was a significant difference between gender and educational level (p=0.025), with female participants revealing a higher level of education. This is consistent with the higher percentage of female students that enrol in college education in Portugal. (40
For 59.3% of the patients, the feelings of being accepted and 55.6% of being relaxed next to their doctor were found. As no other studies were found to compare our results, further studies must now reveal if this is a figure to be improved once GP/FM doctors increase their knowledge on these issues.
For 19.8% of the participants, there was the belief that their doctor knew how they felt about things. A social desirability bias must, nevertheless, temper these figures.
The PDDR’s total score ranges from 8 to 40, with higher scores meaning deeper relationships. The median score was 35, with 54.3% of the respondents scoring higher than that. It is possible that these results can be improved when doctors come to know them and participate in continuous medical development actions.
PEI questionnaire score ranges from 6 to 18, the lower the better. The median score was 12, with 76.5% of the sample below it. More work is needed to explain this apparent paradox, for it is believed that better relationships can improve enablement.
PDDR score according to gender and SEDI, for socioeconomic study, did not reveal any significant differences. Gender, living status, educational level, and monthly income of this sample of patients did not seem to be correlated to the depth of the doctor-patient relationship, meaning that family doctors can achieve good relations with patients from all socio-economic statuses.
When analysing the PDDR score for whether the appointment was with the usual doctor or not, a significant difference was revealed. Patients who had an appointment with their usual doctor scored higher (33.8±5.5 [8 to 40]) than the ones who did not (24.2±6.4 [8 to 40]), p<0.001. This suggests that continuous relationships can be advantageous.
A significant negative weak correlation between the PDDR and PEI total scores was found, meaning that a stronger doctor-patient relationship correlates to hi-gher patient enablement.
For future validation, patients from several healthcare centers, convergent validity with other instruments, such as the ones from patient-centered medicine, are deemed necessary. (41
This study assumes some limitations such as having been performed in one single primary health center (USF Coimbra Sul), the patient’s misleading belief that these questionnaires served as an evaluation of their doctors, and the fact that patients were in the same building as their physician.
Conclusion
The cross-cultural adaptation of the PDDR questionnaire to European-spoken Portuguese and its population was successfully carried out. It is a reasonable measure of the patient-doctor relationship’s depth.
For 54.3% of the study’s sample, a good relationship with its GP/FM doctor existed, a continuous relation-ship being advantageous.
For 76.5% of the patients a feeling of better and more enabled after the medical consultation was revealed.
The deeper the patient-physician relationship was, the more enabled patients felt after the consultation, with a Spearman correlation of ρ=-0.396, p<0.001.
Authors contribution
Conceptualization, MM, LMS, and JAS; methodology, MM, and LMS; software, MM, and LMS; validation, MM, and LMS; formal analysis, MM, and LMS; investigation, MM, and LMS; resources, MM, and LMS; data curation, MM, and LMS; writing - original draft preparation, MM, and LMS; writing - review and editing, MM, LMS, and JAS; visualization, MM, LMS, and JAS; supervision, LMS; project administration, MM, and LMS. All authors have read and agreed to the published version of the manuscript.