A 5-year-old girl had confluent, translucent papules on her tongue for 3 years (Fig. 1A and B). Biopsy revealed dilated lymphatic vessels with mononuclear and polymorphonuclear leukocytes (Fig. 1C).
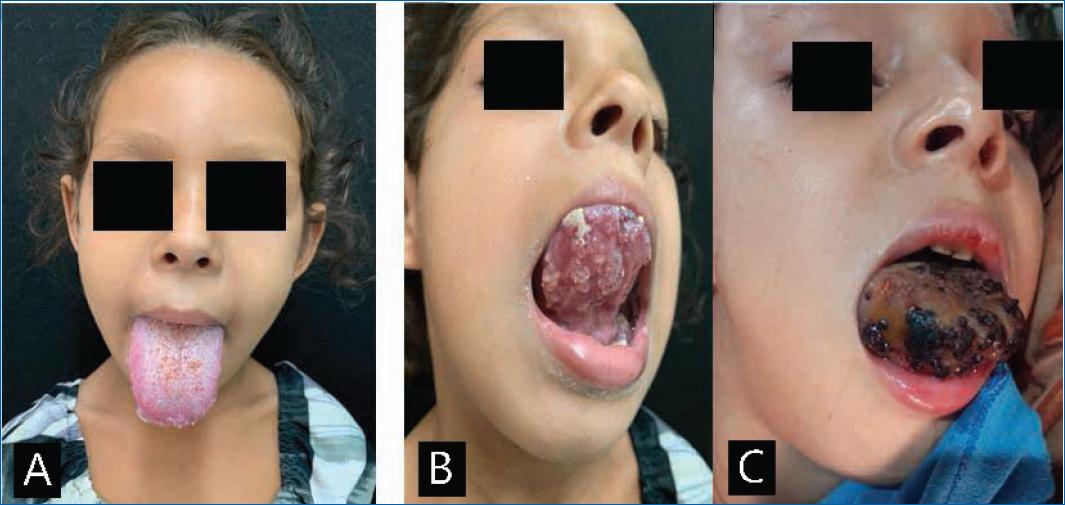
Figure 1 A: lesion in the anterior and posterior portion of the tongue before clinical treatment. B: multiple cystic lesions with serohemorrhagic content on the lingual dorsum before clinical treatment. C: complication 2 days after performing an incisional biopsy for diagnostic purposes.
Dermoscopy showed irregular translucent lakes with clear and serosanguineous content (Fig. 2A and B). After the biopsy, macroglossia worsened, and the papules showed necrotic content (Fig. 3A, B and C).
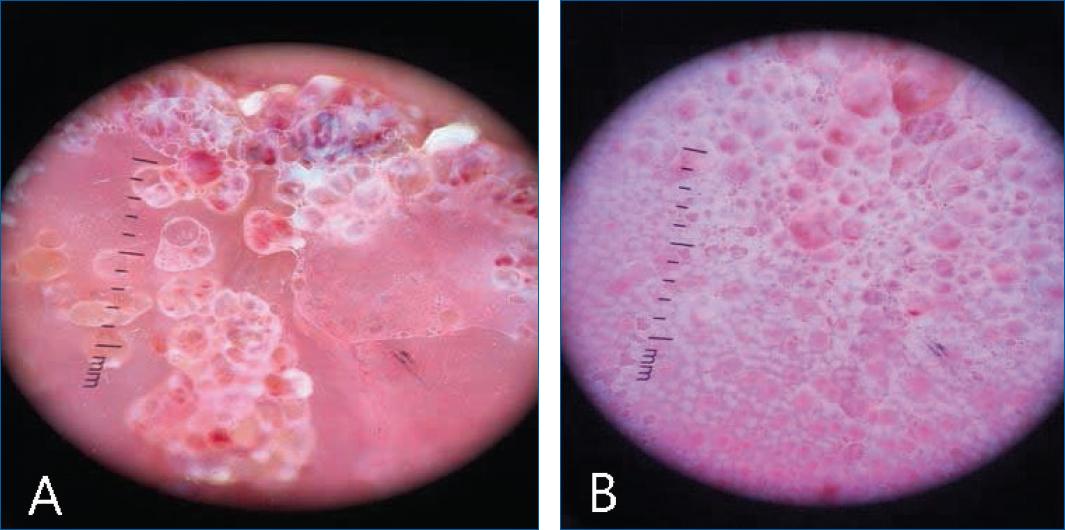
Figure 2 A: dermoscopy under polarized light of the dorsum of the tongue revealing papules with serohematic content and intermingled keratotic areas. B: papules separated by septum demonstrated by dermoscopy under polarized light.
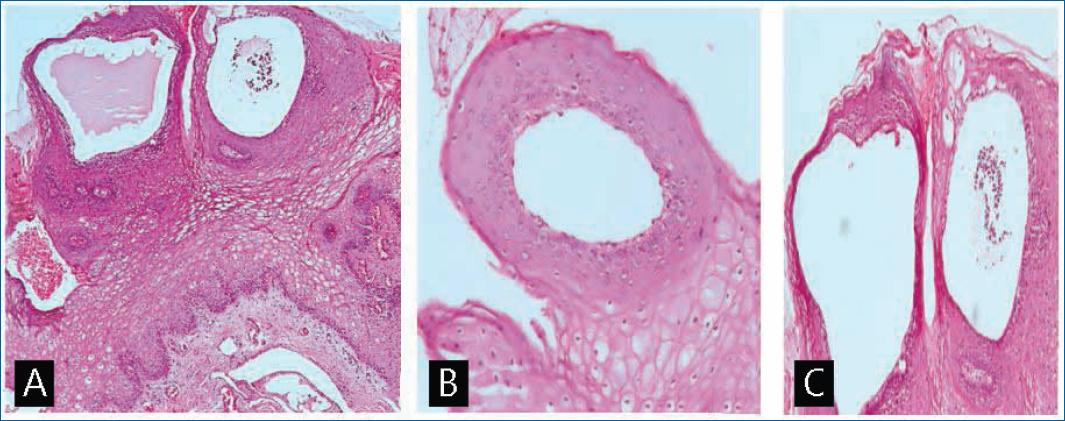
Figure 3 Histopathological features showing dilated lymphatic vessels not connected to the lymphatic network and thin, smooth muscle covered by flattened endothelium, without the presence of a capsule and amorphous lymphatic material inside. A: hematoxylin and eosin (H&E), 100× magnification, B and C: H&E stain, 200× magnification.
Treatment with triamcinolone acetonide ointment to reduce inflammation and systemic antibiotics was proposed. However, imaging exams to verify the extension of the condition and appropriate clinical treatment were not performed because the patient was lost to follow-up.
Discussion
Lingual lymphangioma circumscriptum (LC) is a benign condition that results from the formation of muscle- lined cisterns, not connected to the lymphatic drainage system, projecting bumps on the skin or mucosa1,2.
Congenital or acquired, LC targets the pediatric population and is diagnosed in children under 2 years of age in about 90% of cases2,3. The oral cavity is rarely involved, with the more common site being the tongue and, more rarely, palate, buccal mucosa, gingiva, the floor of the mouth, and lips3.
Clinically, LC is asymptomatic and has a good prognosis. However, cases in the head, neck, and oral cavity may be serious due to obstruction of the airways and death2.
Lymphangioma circumscriptum (LC) treatment remains challenging because current therapeutic options are limited and have to be adapted according to the size of the lesion, its location and the range of anatomical structures and surroundings that are involved. Treatment includes excision, cryotherapy, sclerotherapy, laser, radiofrequency, radiotherapy, and local steroids. Also, topical imiquimod with oral propranolol had success4.
TOPical sirolimus in linGUal microcystic lymphatic malformatioN [TOPGUN] protocol, ongoing until 2025, is studying the efficacy and safety of topical sirolimus in the case of lymphangioma, which can pave the way into the first-line treatment for lingual microcystic lymphatic malformations5.














