Introduction
Population aging and the high prevalence of chronic diseases are increasing the occupancy of hospital beds, and alternatives to conventional hospitalization are needed.
Home hospitalization (HH) is an innovative health model that provides hospital-level care to hemodynamically stable patients with acute medical conditions inside their own residence1,2. However, certain geographic and social criteria need to be met so that home care can be provided safely: the patient must reside in the area of influence of the hospital, and if he is not able to perform the activities of daily living autonomously, there must be a permanent caregiver at home3.
Advantages of this health model compared to conventional hospitalization include a reduction of nosocomial complications, higher patient satisfaction (likely related to patients’ remaining in the comfort of their homes), lower economic costs, and ambulatory medication reconciliation1,2,4.
Literature data about bacterial skin infections, namely acute bacterial dermo-hypodermitis (ABDH), treated at HH are sparse. This article aimed to describe the demographic and clinical features of these patients, to evaluate if this model can be a safe alternative to hospital care, and to assess patients’ global satisfaction regarding their HH experience.
Methods
The first part of this work is a descriptive retrospective study based on the revision of clinical records in which patients admitted to our HH unit with the main diagnosis of ABDH were included in the period from November 16th, 2015, to November 16th, 2022. Exclusion criteria were patients with surgical site infections, hardware/line infections, and bite wounds as entry points. Several variables were studied: age, gender, origin of referral to HH, infection site, number of previous ABDH, the existence of an entry point, risk factors (lymphedema, obesity, and chronic venous insufficiency), comorbidities (arterial hypertension, dyslipidemia, diabetes mellitus, cardiac failure or structural cardiopathy, vascular peripheral disease, cerebrovascular disease, atrial fibrillation, active or treated neoplasia, chronic kidney disease, chronic obstructive pulmonary disease, anemia, gastrointestinal pathology, benign prostatic hyperplasia, thyroid pathology, and osteoarticular disease), oral antibiotic failure at admission, hospital care admission during HH, local infectious complications – blister, abscess, necrosis; systemic complications – bacteriemia, adverse drug reaction, decompensation of underlying disease, death; empiric antibiotic regime, duration; length of stay in HH and hospital care; readmission rate after 1 and 3 months of discharge.
For the second part, the study protocol consisted of a brief, structured phone questionnaire directed to all patients studied in the first part, applied in April 2023. All participants gave their oral consent before participating. The following questions and possible options were asked: (1) “What is your overall satisfaction regarding your HH stay?” – very bad, bad, neither bad nor good, good, and very good; (2) “In the case of a previous hospitalization stay, how do you compare the HH experience with the hospital stay?” – much worse, worse, neither better nor worse, better, much better.
Results
Part I – Characterization of the sample study with ABDH admitted to HH
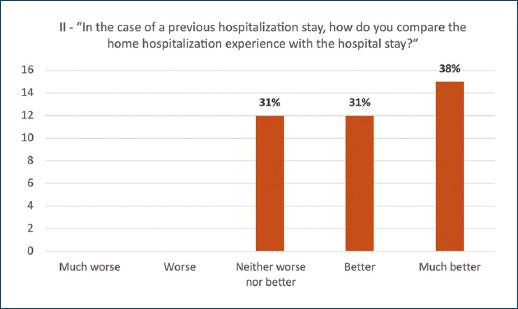
During the study period, 92 patients met the inclusion criteria, but only 88 were eligible (4 patients were excluded). Demographic, clinical features, and local and systemic complications of the study population are described in table 1. About half of the population studied (51%) had at least three comorbidities. Arterial hypertension (65%), dyslipidemia (36%), and diabetes mellitus (25%) were the most common (Fig. 1).
Table 1 Demographic and clinical features of the study population and complications of ABDH admitted at the home hospitalization
| Patients (n = 88) | |
|---|---|
| Age – mean ± SD (min, max) | 66.6 ± 16.8 (20-91) |
| Distribution by age group – n (%) | |
| 20-49 | 15 (17) |
| 50-74 | 36 (41) |
| ≥ 75 | 37 (42) |
| Gender – n (%) | |
| Female | 38 (43) |
| Origin of referral – n (%) | |
| Emergency department | 71 (81) |
| Hospital ward | 16 (18) |
| Hospital consultation | 1 (1) |
| Entry point (e.g., ulcer, tinea pedis or local trauma) – n (%) | 46 (52) |
| Infection location – n (%) | |
| Lower limb | 78 (89) |
| Upper limb | 8 (9) |
| Face | 1 (1) |
| Other | 1 (1) |
| History of previous ABDH – n (%) | 25 (28) |
| 1 episode | 14 (16) |
| ≥ 2 episodes | 11 (13) |
| Risk factors – n (%) | |
| Obesity | 23 (26) |
| Chronic venous insufficiency | 21 (24) |
| Lymphedema | 4 (5) |
| Oral antibiotic failure at admission – n (%) | 24 (27) |
| Antibiotic prophylaxis for ABDH at admission and after discharge – n (%) | 1 (1) | 1 (1) |
| HH length of stay – mean ± SD (min, max), n days | 13,8 ± 6,9 (4-44) |
| Hospital-care and HH – mean ± SD (min, max), n days | 16,4 ± 11 (6-93) |
| Duration of antibiotic treatment – mean ± SD (min, max), n days | 14,6 ± 8,7 (4-57) |
| Local complications – n (%) | 21 (24) |
| Blisters | 13 (15) |
| Abscess | 6 (7) |
| Necrosis | 2 (2) |
| Systemic complications – n (%) | 7 (8) |
| Bacteriemia | 2 (2) |
| Adverse drug reaction | 1 (1) |
| Decompensation of underlying disease | 4 (5) |
| Death | 0 (0) |
ABDH: acute bacterial dermo-hypodermitis; HH: home hospitalization; SD: standard deviation.
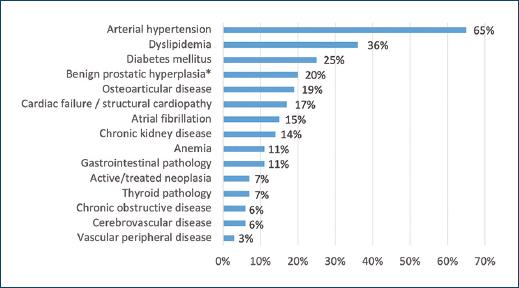
Figure 1 Comorbidities of the study population (n = 88). Arterial hypertension, dyslipidemia and diabetes mellitus are the most frequent.*Percentage relative to male population.
During HH, 8 (9%) patients had to be transferred back to hospital care – 6 patients for clinical decompensation, 1 for surgical drainage, and 1 for social reasons (Table 2). Three patients returned to the HH soon after clinical stabilization.
Table 2 Patients transferred back to hospital care during home hospitalization: 8 patients (9%). Number of home hospitalization patients: 88
| Clinical reasons (7 patients) | ABDH complications (2) | – Abscess drainage in the operating room – Osteomyelitis complicated with bacteriemia Controlled infection after below-knee amputation |
| Exclusion of local complications due to refractory pain (2) | ||
| Adverse drug reaction (1) | – Morbiliform drug eruption | |
| Underlying disease decompensation (2) | – Syncope – Atrial fibrillation with rapid ventricular response |
|
| Social motives (1 patient) | Caregiver unavailability (1) |
ABDH: acute bacterial dermo-hypodermitis.
Fifteen different empiric antibiotic regimens were used for the treatment of ABDH (Table 3): flucloxacillin (45%), intravenous, 4 times per day; ceftriaxone (18%), intravenous or intramuscular, once daily; and piperacillin-tazobactam (15%), intravenous, 3 times per day, were the most frequently chosen. Only one patient was treated with penicillin G, intravenous, 6 times per day. The average number of days of antibiotic therapy for ABHD was 14.6 ± 8.7.
Table 3 Empiric antibiotic regimen for acute bacterial dermo-hypodermitis
| Patients (n = 88) | |
|---|---|
| 1st line empiric antibiotic regimen – n (%) | |
| Flucloxacillin | 40 (45) |
| Ceftriaxone | 16 (18) |
| Piperacillin-tazobactam | 13 (15) |
| Clindamycin | 4 (5) |
| Ceftriaxone + Clindamycin | 3 (3) |
| Meropenem | 2 (2) |
| Flucloxacillin + Penicillin | 2 (2) |
| Imipenem + Cilastatin | 1 (1) |
| Flucloxacillin + Amoxicillin-Clavulanate | 1 (1) |
| Vancomycin + Flucloxacillin | 1 (1) |
| Clindamycin + Penicillin | 1 (1) |
| Clindamycin + Flucloxacillin | 1 (1) |
| Amoxicillin-Clavulanate | 1 (1) |
| Cefuroxime | 1 (1) |
| Penicillin G | 1 (1) |
| 1st line empiric antibiotic failure – n (%) | 6 (7) |
| Penicillin allergy – n (%) | 3 (3) |
Part II – Patients’ global satisfaction regarding HH stay
From the 88 patients admitted to HH, we could only apply the phone questionnaire to 49: 10 patients had passed away, and 29 had unavailable phone numbers.
The median number of days between patients’ HH and the phone questionnaire was 1262 (the minimum interval was 150 days and the maximum was 2643).
The results to the first question, “What is your overall satisfaction regarding your HH stay?” are presented in figure 2. Most participants (n = 41; 84%) rated HH with the maximum grade of satisfaction, and none classified it as “very bad” or “bad”.
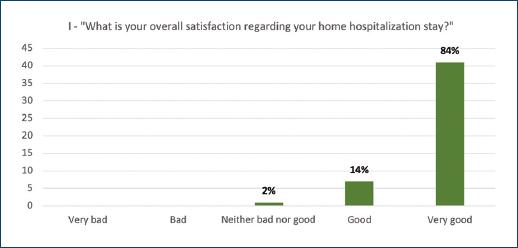
Figure 2 Phone questionnaire. Patients’ global satisfaction regarding home hospitalization (n = 49). Results are shown in frequency (y-axis) and percentage.
The second question focused on the comparison between patients’ satisfaction with HH and conventional hospital stay. Ten participants had never had a previous hospital stay. The results are presented in figure 3: 27 participants (69%) preferred HH to hospital stay, and the rest (n = 12; 31%) had no preference between the two models.
Discussion
Compared to studies of inpatients with ABDH, the mean age of our population was higher than reported by Wojas-Pelc et al. and Roda et al. (63 and 61.2 years, respectively) and slightly inferior to that described by Batista et al. (68.6 years)5-7. As in previous studies, the prevalence was higher in males, and the lower limb was the most frequent site of infection8,9. The percentage of patients with previous ABDH was similar to that reported by Batista et al. (30.4%)7.
Dupuy et al. found that local risk factors (e.g., toe web intertrigo) are the most important in the epidemiology of lower limb ABDH, and in our work, more than half of the patients had an identified portal of entry (Table 1)10. This data shows the importance of identifying and treating these factors in the prevention of ABDH.
The percentage of local complications was lower than described by Wojas-Pelc et al. in a retrospective analysis of 319 hospitalized patients with ABDH (25%) and higher than reported by Roda et al. (18%)5,6. Systemic complications such as bacteremia, adverse drug reaction and decompensation of underlying disease were identified in 8% of patients, a significant lower percentage than reported by a study with 102 patients hospitalized with ABDH (16%)7. These data can be explained by the higher clinical stability of ABDH patients admitted in home care. Only seven patients (8%) needed transfer to hospital care for clinical reasons, a lower percentage compared to a similar study with 101 patients with cellulitis treated with intravenous antibiotics at home, wherein 11 patients (12%) required hospital admission due to complications11. The low readmission rate 3 months after discharge (1%) is noteworthy. This data indicates that the HH team, in most cases, can address ABDH and its comorbidities effectively and safely.
The mean duration of antibiotic therapy, which already includes days of treatment after clinical discharge, was very similar to that reported by Batista et al. (14.5 days) and higher than other studies of inpatients with ABDH7,10. The prolongation of antibiotic therapy may have to do with the persistence of inflammatory signs in a later phase of ABDH, which is probably related to the local reaction of degradation products of the microorganism and tissue damage and not with persistent infection7.
The mean length of stay (including home and hospital stays) was longer than that reported by Batista et al. (12.9 days) and Kozłowska et al. (11.6 days), both studies of ABDH treated in hospital, which could be explained by the overcrowding problem of conventional hospitalization and higher pressure to discharge7,12. Corwin et al., in a randomized controlled trial comparing intravenous antibiotic treatment for cellulitis at home versus in the hospital, did not find a significant difference in the number of days for discharge between the two groups of patients11.
Only 1 patient (1%), who had 6 previous episodes of ABDH, was on prophylactic antibiotic therapy, a lower percentage than reported by Roda et al. (4%)6. We did not have access to the timing of this patients’ previous ABDH episodes; however, it should be emphasized that in patients with recurrent episodes (3 or more per year) or with lymphedema, the initiation of prophylaxis with monthly intramuscular benzathine penicillin G should be considered7.
The data suggest that our population is aged and has a high prevalence of comorbidities. Still, the percentage of systemic complications is similar to that of patients admitted to hospital care. On the other hand, whenever there is a serious clinical decompensation or when social or geographic criteria are no longer met, patients are immediately transferred to the hospital, ensuring their safety.
The participants showed an extraordinary rate of satisfaction regarding their HH experience. Most of the participants with previous hospital admissions preferred home care over hospital care; these results are in line with the existing evidence, where several studies (evolving medical conditions such as cellulitis, chronic heart failure and chronic obstructive pulmonary disease) reported increased patient satisfaction in the group treated at home1,13,14. These findings support further dissemination of the home care model.
The study has the limitations of a retrospective analysis, a reduced sample, and the absence of well-defined clinical criteria for the treatment of ABDH at HH. Regarding the limitations of the phone survey on patient satisfaction, we report the small size of the participants as well as the subjectivity of the questions. When comparing home and in-hospital care, satisfaction results may be influenced by the potential severity and instability of the medical condition that required conventional hospitalization.
Conclusion
This study suggests that, even though the population with ABDH admitted to HH is aged and has a high prevalence of comorbidities, HH is a safe and effective alternative for stable ABDH. It’s not only a solution to the overcrowding problem of hospitals nowadays but also to reduce nosocomial complications and improve patient and family empowerment.
This work also corroborates the association between HH and high levels of patient’ satisfaction.
Further studies are needed to identify clinical criteria to select the patients that will benefit the most from this alternative model of care.