Introduction and Aim
Endoscopic retrograde cholangiopancreatography (ERCP) is a minimally invasive, nowadays essentially therapeutic, advanced endoscopic procedure for biliary and pancreatic diseases. The vast majority of ERCP procedures is performed on adult patients and increasingly in the very elderly [1], as the incidence of biliary and pancreatic diseases requiring intervention is growing in this age group. In the pediatric population, ERCP has been performed for several decades, with the first pediatric biliary sphincterotomy performed in 1982, but it remains an uncommon procedure [2].
Its conservative use in children is a result of the low incidence of biliopancreatic diseases requiring ERCP, the perception that the procedure is technically more difficult in this age group, uncertainties about indications and safety, and ongoing debate on the examiner’s qualification [3, 4]. Frequently, pediatric patients requiring ERCP are referred to high-volume, highly specialized, adult referral centers, with high technical expertise, but less familiarity with pediatric diseases [4].
Furthermore, the pediatric age group is a nonhomogeneous population, including the very young patients with particular age-related indications (e.g., biliary atresia, choledochal cysts) and anatomical conditions requiring specific pediatric endoscope; and on the other side adolescents with clinical and anatomical characteristics that resemble adult patients [5]. The aim of this retrospective observational study was to characterize the experience of an adult endoscopy unit with ERCP on pediatric patients, with a special focus on very young patients.
Population and Methods
Our center is an academic, tertiary, and referral hospital in Lisbon (Portugal), providing health services for 1.5 million inhabitants in a country with about 10 million inhabitants. It is composed of a group of hospitals in central Lisbon and has most medical and surgical specialties for both adult and pediatric population. The Bilio-Digestive Techniques Unit is part of the Gastroenterology Department for adults and was established on 1982. It is one of the first units performing ERCP in Portugal and has been accumulating expertise over the last decades, becoming nationally recognized by many colleagues and departments from other hospitals that commonly refer their patients directly to this unit when local resources or expertise is lacking.
In our center, we perform 350-400 ERCPs in adult patients every year and provide services for children of all ages suffering from gastrointestinal, liver, or pancreatic diseases. Care for these children is organized in multidisciplinary teams, with close cooperation between adult gastroenterologists, pediatricians, and pediatric surgeons.
For this study, we reviewed every ERCP performed on individuals aged 17 years or less at the Bilio-Digestive Techniques Unit between January 1, 1994, and June 31, 2022. Physical and electronic medical records were searched and assessed, both related to the endoscopic procedure and to the respective hospital admission.
Patient characteristics, endoscopic procedure details, and registered complications were analyzed. Technical success of the intervention was defined as deep cannulation allowing accurate diagnosis and/or adequate therapy as to the pre-specified indication. Due to the procedural specificities of this particular demanding technique when performed on very young patients, a subanalysis was performed on procedures performed on patients aged 5 years or less. Statistical analysis was performed with Microsoft® Office Excel.
Results
Over the 27-year period between January 1994 and June 2022, 65 ERCPs were performed on 57 patients at the Bilio-Digestive Techniques Unit of our center.
Overall Population
Demographics
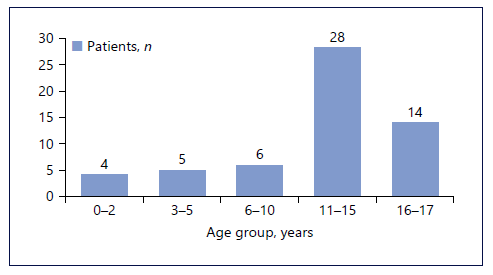
Most patients were male (n = 34; 59.6%), and the median age was 13 years (range 1-17 years). Nine patients were aged 5 years or less (corresponding to 12 ERCPs), and 4 patients were aged 2 years or less (Fig. 1). The ma-jority of the patients (n = 51) underwent a single procedure, 5 patients underwent two procedures, and 1 patient underwent three procedures.
Indications
Indications for ERCP were biliary obstruction (n = 40; associated with cholangitis in 4 cases), mainly due to choledocholithiasis, lithiasic acute pancreatitis (n = 19), recurrent pancreatitis (n = 3), stent extraction (n = 2), and post-operative biliary fistula (n = 1).
Interventions
All procedures were performed by adult ERCP highly expert endoscopist (total of 5 endoscopists with a median of 8 procedures/endoscopist), with attending pediatricians, pediatric anesthesiologists, and therapeutic endoscopy nurses on-site, under general anesthesia, with the patient in the prone position. Adult duodenoscopes were used in all procedures. Selective biliary cannulation was performed with a catheter (5.5 Fr), and the guidewire-assisted technique has been used since 1998. Ambient air was used for insufflation until 2020 when carbon dioxide became available at our center.
Routine post-ERCP pancreatitis prophylaxis with rectal indomethacin was performed in all patients since 2010. ERCP was finished as therapeutic ERCP in 52 interventions (80%) and as diagnostic in 13 (20.0%). Successful intervention was achieved in 95.4% (62/65 ERCPs). In 3 patients with acute pancreatitis, aged 12-17 years old, cannulation of the papilla was not possible due to duodenal edema.
Diagnostic Findings
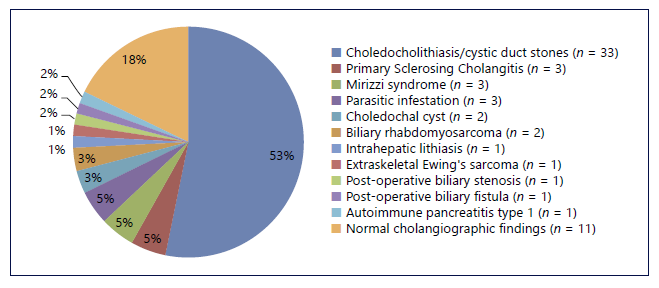
Diagnosis after ERCP was (≥1 diagnosis/patient) choledocholithiasis/cystic duct stones (n = 33; 6 patients with hemolytic anemia), primary sclerosing cholangitis (n = 3), Mirizzi syndrome (n = 3) (Fig. 2a), parasitic infestation (n = 3), choledochal cyst (n = 2), biliary rhabdomyosarcoma (n = 2) (Fig. 2b), intrahepatic lithiasis (n = 1), extraskeletal Ewing’s sarcoma (n = 1), post-operative biliary stenosis (n = 1), post-operative biliary fistula (n = 1), and autoimmune pancreatitis (n = 1). The final diagnoses after the procedures are demonstrated in Figure 3. A normal cholangiography was found in 11 exams.
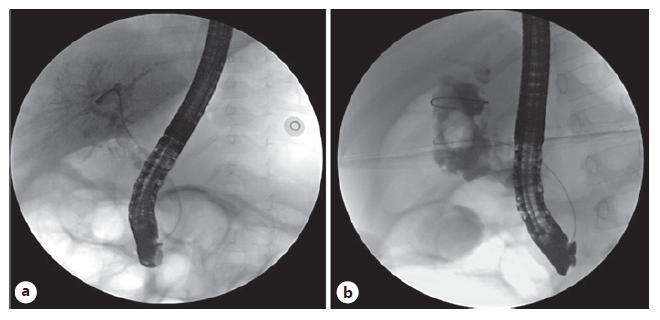
Fig. 2 Cholangiography of a 15-month-old boy with Mirizzi syndrome (a) and a 4-year-old boy with biliary rhabdomyosarcoma (b).
Autoimmune pancreatitis, an infrequently recognized disorder in this age group, was diagnosed in a 13-year-old male presenting with abdominal pain, elevated pancreatic enzymes, and cholestasis. Imaging tests showed a pancreatic head mass and dilatation of the biliary tree. Serum immunoglobulin G4 levels were elevated (280 mg/dL), and cancer antigen 19-9 was normal. He underwent endoscopic ultrasound with fine needle aspiration of the pancreatic mass, and histopathology revealed lymphoplasmacytic infiltrate with fibrosis, negative for immunoglobulin G4 staining and neoplastic cells. ERCP revealed stenosis of the intrapancreatic bile duct. Biliary drainage with stent placement and an exfoliative cytology were performed with success.
Endoscopic Therapy
Therapeutic procedures were performed in 52 ER-CPs: sphincterotomy of the biliary duct (n = 42; 64.6%) with precut in two cases, common bile duct exploration with Dormia basket/Fogarty balloon (n = 41; 63.1%), extraction of biliary stones/parasites (n = 33; 50.8%), insertion of biliary plastic stents (7-10 Fr, 5-9 cm) (n = 14; 21.5%), stent extraction (n = 8; 12.3%), insertion of pancreatic stent (n = 4; 6.2%), and exfoliative cytology (n = 3; 4.6%).
Adverse Events
Clinical follow-up was done as inpatients for at least 24 h after the procedure in all patients. Complications were recorded in two procedures (3.1%). There was one episode of mild pancreatitis, managed conservatively, and one case of immediate post-sphincterotomy bleeding, resolved with endoscopic therapy (adrenalin injection) during the procedure. There were no complications attributable to mechanical stress on the gastrointestinal tract, perforations, or cardiopulmonary suppression. No mortality was associated with ERCP.
Population Aged 5 Years or Less
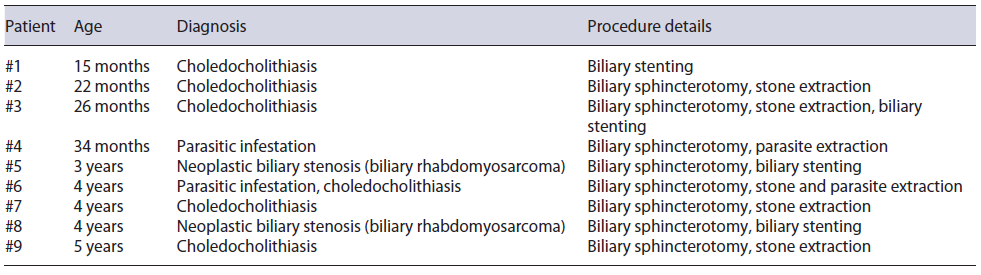
Due to the diagnostic specificities and particular technical demands of ERCP on very young patients, we detail on this population in Table 1. In total, 12 ERCPs were performed on 9 patients aged up to 5 years.
Discussion
In our experience, ERCP in children can be safely performed with high success rates by advanced adult-trained expert endoscopists at a high-volume center. This adds to the growing evidence supporting the use of ERCP by skilled endoscopists in this age group [3]. Few pediatric gastroenterologists receive sufficient training on advanced endoscopy including procedures such as ERCP. This gap is usually filled by adult gastroenterologists. It is particularly helpful to coordinate findings and further therapeutic steps with the attending pediatrician as adult-trained endoscopists may not be familiar with specific pediatric diseases [6].
Pediatric duodenoscopes are recommended for children <10 kg or younger than 12 months of age, beyond which an adult diagnostic or therapeutic duodenoscope is acceptable [7]. A standard adult duodenoscope was used in all procedures since all the children were older than 12 months of age/weighing more than 10 kg and our endoscopy unit does not have a pediatric duodenoscope, which is in accordance with current ASGE recommendations.
In Western countries, the most common indications for adult ERCP are choledocholithiasis and acute/chronic pancreatitis, as was seen in our pediatric cohort. This is not surprising given the median age of 13 years of our population and the fact that indications in adolescents are comparable to adult ERCP.
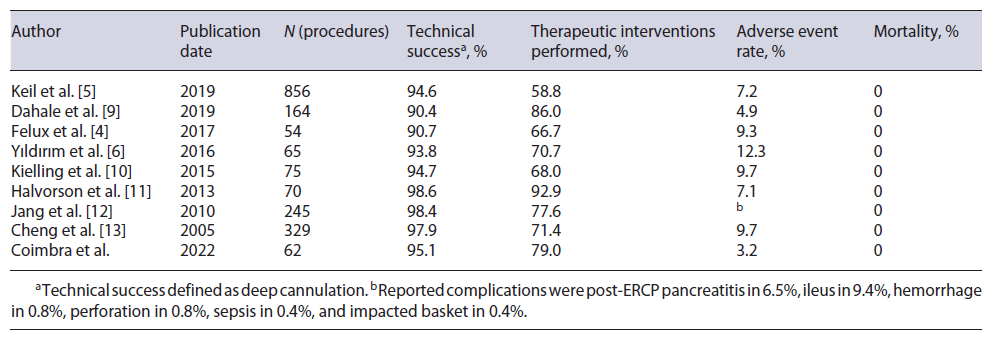
The technical principles of selective biliary cannulation in children are similar to those used in adult patients, with the additional limitations of space within the duodenum in small patients. Despite this, the technical success rate was very high, similar to what has been reported for other pediatric (89.5-100%) (Table 2) and adult populations [6].
Table 2 Comparison with other large single-center series of ERCP performed on patients aged up to 18 years for non-selected indications
ERCP was performed for diagnostic intent in some procedures at the beginning of our observation period, when alternative noninvasive diagnostic methods were still unavailable. Given the development of imaging methods, especially magnetic resonance cholangiopancreatography, diagnostic indications have naturally decreased, and in the most recent years ERCP has been indicated essentially as a therapeutic procedure [5]. There was a remarkable amount of therapeutic interventions (80.0%) in this pediatric patient series. In most of the procedures, more than one intervention was performed.
The incidence of procedure-related complications in children has not been well established in prospective studies. Reports in literature suggest complication rates between 3 and 10% in children older than 1 year [2]. It is unclear whether complication rates are slightly higher in infants younger than 1 year. The overall complication rate found in the present study was lower than the rates observed in the literature in other pediatric populations, but the retrospective nature of the study may lead to its underestimation (Table 2).
There is some evidence that administration of indomethacin via rectal suppository at the time of the ERCP may help prevent post-ERCP pancreatitis, based on a preponderance of evidence in adults [8]. Children-specific recommendations on minimizing adverse events are lacking and are usually extrapolated from the adult population [3]. We routinely used indomethacin for prophylaxis since the recommendation was established for adult patients, and as patients are monitored for at least 24 h after ERCP, post-procedure pancreatic enzyme levels are not regularly measured.
This study has several limitations that should be noted, namely, due to its retrospective nature. Complete medical reports were not available on all patients because of the use of paper charts in the 1990s and early 2000s. The best reasonable efforts were made to attain all available records, including those archived and stored at off-site facilities. Nevertheless, incomplete records may influence outcomes such as underestimating the total adverse event rate and limiting access to other important information, such as the length of stay of biliary stents and how they were removed (upper endoscopy or new ERCP). Notwith-standing these limitations, our study covers 27 years of pediatric ERCP experience from a large endoscopic referral center with an associated dedicated children’s hospital.
The results emphasize the beneficial impact of ERCP in a pediatric cohort, with high success rates and a low overall rate of adverse events. The overall efficacy and safety support the performance of pediatric ERCP by experienced adult endoscopists at high-volume centers.
Pediatric patients who require ERCP should be managed in a multidisciplinary team, with close cooperation between adult and pediatric gastroenterologist. We consider this setting a prerequisite for ERCPs in this age group since adult-trained endoscopists may not be intimately familiar with specific pediatric diseases.