Introduction
Anemia is a major public health problem affecting both developed and developing countries. According to the World Health Organization, the prevalence of anemia among pregnant women in developed countries is approximately 14 percent, whereas it remains as high as 51 percent in the developing world 1-4. Anemia in pregnancy is called a “potential danger to mother and child” to be taken seriously by all parties involved in health care at the forefront line 3,5-7.
The results of basic health research conducted by the Indonesian government (Riskesda 2018) show that antenatal visits in Indonesia are still low at 86.6 percent for K1 (first antenatal visit to the midwife) and antenatal visits four times only 74.1 percent. Pregnant women who do not perform will not receive any antenatal visits (7T) or assistance that includes weight scales and iron tablets. 7T antenatal care includes weighing, measuring blood pressure, measuring the height of the fundus, providing complete tetanus toxoid immunization, provision of iron (Fe) tablets of at least 90 tablets during pregnancy, testing for sexually transmitted diseases, and referral preparation counseling (8). Consumption of iron is needed by pregnant women to prevent maternal and fetal anemia and other complications. Pregnant women are expected to consume more than 90 iron tablets during pregnancy. But in fact, 80.7 percent of pregnant women do not consume iron tablets 8-11.
A lack of iron consumption during pregnancy can lead to anemia in pregnant women. The prevalence of anemia in pregnant women in Indonesia in 2018 was as high as 48.9 percent, which means that 5 out of 10 pregnant women suffer from anemia. This condition is alarming because the government has run programs for iron tablet supplementation in pregnant women since 1970. Sociocultural factors also contribute to anemia. The absence of certain food knowledge in pregnant women contributes to anemia. There are also suggestions that during pregnancy, pregnant women’s food should be reduced because, in case the fetus becomes large, there is a fear about the labor 1,8,12-14. Based on the above, the discussion of the concept of EMIC that causes anemia is interesting for studying the factors and finding an attempt to tackle the problem of anemia. This study aimed to determine the basics or factors that are contextual causes which could contribute to maternal anemia and efforts to combat anemia in pregnant women from the perspective of pregnant women themselves. These findings will provide a better understanding of anemia during pregnancy for the prevention and control of anemia in during pregnancy.
Materials and Methods
This research is qualitative research using a phenomenological survey approach 15,16. This study uses phenomenological research and ethnographic methods. Research on phenomenology and ethnographic methods is qualitative research that departs from a phenomenon found in the field and reveals about culture and people’s lives. Phenomenology is a qualitative research approach that describes the meaning of the life experience of a phenomenon in several individuals, which in this case is anemia during pregnancy. Moustakas’ transcendental phenomenological approach, adapted from Husserl, was applied in this study, namely focusing on the descriptions given by the participants to produce the essence of life experiences. The ethnographic type is research that is more about “portraits of people” about descriptions of particular cultures, customs, beliefs, and behavior.
The objective of this study was to understand the phenomenon of anemia in pregnant women, which includes contextual factors that influence anemia in pregnant women, as seen in the cases that have been studied in this research, as well as efforts to combat anemia in pregnant women. The study participants were 20 pregnant women with anemia and 12 with focus group discussions. Pregnant women participants who met the requirements were identified by first checking their HB (hemoglobin) levels. This examination was conducted by a research team in collaboration with the Tanjung Rejo Community Health Center. A total of 48 pregnant women were examined, and 72.92 percent of pregnant women had anemia (35 women).
Informants were directly recruited, carried out on purpose, and designed to produce maximum varieties according to age, gravida, educational level, employment status, economic social status, and residence. Variety in sampling is based on these factors, as they affect maternal awareness and eating behavior during pregnancy. In addition, the inclusion criteria were pregnant women with anemia; willingness to participate in research and provide informed consent; and the ability to understand, speak, and communicate in Indonesian interviews. The exclusion criteria were pregnant women with severe anemia and reluctance to participate in any stage. The interview was conducted by the first author, a female doctoral candidate in public health who is familiar with qualitative research, has 20 years of work experience in the field of community nutrition, and is interested in this research topic. Other authors are experts in qualitative studies. The second and third authors are professors and PhDs in public nutrition, and the fourth author is a doctor of anthropology familiar with qualitative research, especially ethnographic research. A combined method of interviewing and sharing stories is applied. The interviewer provided open-ended questions and allowed time for participants to tell their stories. In conducting the interviews, the researcher did not use a list of questions, but the researcher asked the participants to follow the storyline. This method aims to provide flexibility and comfort for participants to express their opinions and understanding without the impression of patronizing/teaching and directing them.
In conducting the interviews, the researchers made home visits. The number of interview visits was different for each participant, but the average number of interview visits for each person was 4-5 times. The first visit aimed to build relationships with participants so that the interviewer had a close relationship with them. Since the participants were generally housewives, the interview time was adjusted according to their conditions. Interviews were conducted naturally, such as when the mothers cooked, cleaned the house, or washed dishes and clothes. The interviews ranged from to 30-60 min. To triangulate the data, the researcher interviewed the husbands of the participants and the parents of pregnant women who lived with their parents. The list of questions for this triangulation was created based on the results of the interview with the pregnant woman.
The interviews were recorded with the consent of all participants. Field notes were taken during the interviews. The researcher also recorded observations of nonverbal behavior, encounters, and interactions. The data collection procedure was carried out until data saturation occurred, that is, no new data were found. After in-depth interviews were conducted, Focus Group Discussions (FGDs) were conducted with key informants.
The results of in-depth interviews serve as the theme of the FGD. Twelve FGD informants were involved with pregnant mothers at health centers amounted to 12 people. The FGD informants consisted of one nutrition officer, two staff villages (village office), three midwives, a midwife coordinator, the head of the health center, two cadres, and two pregnant women. FGDs were conducted in the conference rooms of the PHC Tanjung Rejo.
Data Analysis: Tolley et al. 15 (2005) stated that qualitative data analysis began with spaciousness 15,17. Data analysis was performed manually and simultaneously with data collection. The interviews were transcribed word for word by all authors. The texts were read several times to identify general ideas. Units of meaning were identified, related units of meaning were combined, and codes were generated. Similar codes were combined, and codes that had related meanings were grouped into subcategories. After comparing the subcategories, the conceptually similar subcategories were combined to form the main category.
Credibility was achieved by spending sufficient time on data collection (approximately 8 months), ensuring diversity of participants, and including member checking (in which transcripts were returned to the participants for comment or correction). To confirm the validity of the data, coded interviews were conducted with six participants and their final opinions were determined. Members of the research team actively transcribed and analyzed the results, a process that included reviewing interviews and codes, discussing the findings, and compiling the final results. Dependability and conformability increased through external checking and peer debriefing. Regarding transferability, purposive sampling was used to obtain maximum variety. Authenticity was evaluated through member checking, in which participants compared the results documented by the research team to their views.
Results
The factors found were categorized into three thematic groups in our article, namely:
Anemia in the Preconception Phase
All informants interviewed were married early aged 16-20 years. During adolescence, they go on a diet that limits their food intake so that they do not become fat. Six informants experienced miscarriages due to anemia. Eleven informants stated that before marriage, they had experienced symptoms compatible with anemia, such as weakness, lethargy, and pallor, but had never seen a doctor. Six people were diagnosed by doctors with anemia in their teens due to fainting during menstruation. They stated that their anemia was normal, so it was not a frightening problem.
P1: “… when I was pregnant I didn’t like to eat before I became pregnant even when I was a teenager I didn’t like to eat, I liked snacking on crackers and snacks. It’s normal like that until I was pregnant.”
P12, who married at the age of 18, shared the same thing. Based on the results of the anemia screening, the mother was indeed suffering from anemia. She was pregnant with her second child at 5 months, but when she was pregnant with her first child, she had a miscarriage at 4 months.
P12: “I was pregnant with my second child, but my first child when I was 4 months pregnant had a miscarriage. The doctor said I was anemic. During pregnancy, I was indeed weak and dizzy. But before I got pregnant I also often had sudden headaches. As a teenager, I’ve experienced symptoms like this a lot.”
P20 is a mother aged 20 years and is pregnant with the first child at 5 months of pregnancy. She states that adolescents (before marriage) are already suffering from anemia (what she calls anemia) but have never seen a doctor. I know from the symptoms, namely, easily tired, weak, dizziness, and slight menstrual blood.
P20: “I do not know that I am pregnant now lacking blood because I felt when I was pregnant now I was healthier before marriage. When I was a girl, I liked to diet. I often took slimming drugs. When I was a teenager, I often experienced dizziness even when I was a girl - suddenly fainted. Blood was a little. So when I was pregnant I never fainted again. Dizziness and fatigue are common for pregnant women. The mother said that she often ate satay and ate the fruit to add blood. So, since this pregnancy, I have eaten satay almost every time, night.”
The anemia experienced by the informants at this time was probably related to previous medical history. From the interviews, it was also found that the informant had anemia.
P4: “When I was pregnant with my first child, I had a Hb test. At that time, there was also a free check in the village; he said I was anemic.”
P7: “When I was a teenager, I often got dizzy. I got tired easily and even fainted when I was menstruating. I went to the doctor and the doctor said I was anemic.”
Diets That Cause Lack Consumption of Iron
From interviews with informants, we found that the pattern of consumption illustrates the lack of intake of iron from the daily menu for pregnant women. The consumption of green vegetables as a source of iron was also low. Fruits are a source of vitamin C, which aids the absorption of iron in the body is also very less. In addition to current eating habits, consumption of meat, vegetables, and fruit is also influenced by economic factors and myths. From the interview, the informant stated that they were bored of eating fish, and some also stated that the fish was not consumed during pregnancy because of the stench which may have resulted in the birth of the baby being too fishy. The consumption of meat is the best source of iron, and in addition to being expensive, meat is also difficult to find in shops/markets. If there is a party, they eat meat.
The informant also stated that they know if shrimp or prawn ronggeng centipedes, which are found in the village, and their cheap price can contribute to increasing iron levels and consequently the concentration of maternal hemoglobin, but ronggeng prawns are also not consumed because they are bored with the taste of the prawns. A diet that illustrates the lack of intake of iron was also influenced by their favorite foods, such as informants liked to eat instant noodles since the girl and continued during pregnancy. Informants eat instant noodles without a full meal, such as rice, vegetables, and side dishes.
P5: “......I usually eat small portions. As the girl, I also lazy to eat vegetables. Eating fruit cannot be right during pregnancy. My mother forbade me to eat fruit, especially when young and pregnant. Because it tastes sour fruits that can result in heartburn during pregnancy. Fruit that can be eaten during pregnancy is just bananas alone. And that’s not often. Bored too.”
P8: “.... fish here a lot, but bored to eat the fish hold. Better to eat tofu or tempeh or eggs. Cheap and tasty. If you eat meat, it is expensive. It is difficult to find meat in the stall, must be ordered first. When there is a party, then I eat meat.”
P15: “....I prefer to eat tofu, tempeh, and eggs. The fish here is plentiful, but fish will cause the baby to smell fishy. If you eat meat, it’s very expensive.”
P17: “I do not like to eat anything if there is no instant noodle. Every day I eat instant noodles.”
Like the previous informant, this pregnant woman is also aware that prawn ronggeng can help to increase hemoglobin, but she also does not consume this food, being cheap.
“the ronggeng prawn also can blood added, but it can make you feel dizzy when you eat it.” (P1, P9, P11, P13, P17)
“the ronggeng prawn also can blood added, but it should not be a lot. Later his son fat times.”(P5, P8, P16)
In addition to a favorite food, some drinks are also one of the possible factors causing the lack of iron intake in the body, as some informants like coffee and sweet tea. From the interviews, several informants liked drinking hot tea while eating to prevent nausea and vomiting. Advertisements on television also greatly affect the diet of pregnant women, such as instant noodle advertisements that provide a lot of nutrition. The diet of the informants did not vary, and meal portions were incompatible with the food portions recommended for pregnant women. Pregnant women prefer to eat instant noodles and drink milk because they believe that the nutrients they need have been met by this type of food. Daily consumption of pregnant milk is believed to have adequate levels of nutrition during pregnancy.
P11: “I always eat with warm sweet tea to prevent nausea and vomiting.”
P19: “... I have the habit of drinking coffee because the body feels fresh coffee. This coffee drinking habits I have had since I was a teenager.”
Knowledge and Consumption of Iron Tablets in Pregnancy
The informant did not know the function or benefits of taking an iron tablet. Informants knew the Fe tablet given to the midwife every month as the blood booster, great shape, and the color red. Informants had a common understanding of the lack of blood related to the blood pressure that is measured each month. The informant states that if their blood pressure is good, then they are not anemic, so there is no need to take an iron tablet given by a midwife. Informants also argue that it is a blood booster medicine. In large numbers, drugs are not consumed by pregnant women. Informants do not consume iron tablets because of the large tablet size, smell, nausea, and fear because of the black stool.
The informant also stated that she never received an explanation or clarification from the midwife about the iron pills when they were given. The research team also found that the number of iron tablets received by participants varied each month. However, some informants received only 10 iron tablets from midwives during antenatal examinations. Some of the informants received only five iron tablets. If the informant did not examine the midwife, the informant did not obtain an iron tablet. Lack of communication, education, and information from midwives to pregnant women causes a lack of knowledge about the importance of consuming iron tablets during pregnancy. Pregnant women stated that iron tablets given by midwives are drugs that are not good for consumption during pregnancy.
P12: “Every month I do a pregnancy check-up with the midwife. The midwife gave me 10 tablets of medicine. The midwife said the drug was for a blood booster. But I don’t take the medicine because my blood pressure is normal, so why should I take the medicine?”
P5: “Fe tablets are medicine. I have heard information on television that states pregnant women should not take much medicine. If a pregnant woman eats a lot of drugs while pregnant, it can cause her child to have a disability. That’s why I never ate the Fe tablets given by the midwife. I am afraid my son is deformed.”
P11: “I did not ever drink tablet that the red color bu. this medicine treatment. I’m fine really. Besides, taking medicine was not good for a lot of pregnant women, right, Mom? Each month midwife said indeed, do not forget to take his medication yes ma’am, but that’s mom, not my ever eaten.”
P4: “I am pregnant with my fourth child. However, the midwife never told me about the iron tablets. The midwife only gives tablets which in my opinion are medicines for pregnant women. The midwife just reminded me not to forget to take the medicine. That’s all.”
P7: “Every month I check with the midwife, the midwife will measure my blood pressure and listen to my baby’s heartbeat. There is a device stuck in my stomach. The midwife declared my child healthy. However, every checkup the midwife gave me medicine. I didn’t know what medicine it was, the midwife never explained it. The midwife said, don’t forget to take medicine so that the baby is healthier. I just want to know it’s a blood booster, right? Because it’s red and well-shaped. My friend said it was a blood booster, even though I didn’t take it because my baby is healthy.”
P8: “... every month I go to the midwife for antenatal care. When I go to the midwife for antenatal care, I get 5 Fe tablets, but I never take them.”
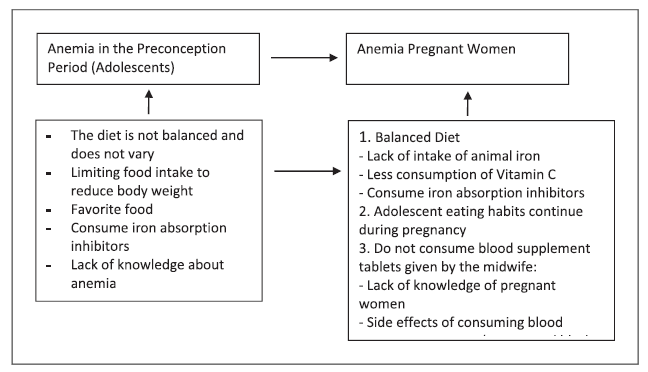
The Phenomenon of Anemia in Pregnant Women
Figure 1 illustrates the anemia cycle that occurs in pregnant women.
Discussion
In our study, we found that dietary problems during adolescence persisted during pregnancy. This error in the adolescent diet predisposes pregnant women to anemia. A balanced diet during childhood and adolescence is essential not only for a child’s well-being and growth but also for the formation of healthy eating habits that will continue 18-20. The results showed that the habit of limiting certain food intake during adolescence and favorite foods during adolescence continued to become a habit during marriage and even during pregnancy.
Adolescents are one of the most vulnerable groups to anemia and are the least explored area. The prevalence of anemia among adolescent girls in this category remains relatively high. Adolescence is a transition period between childhood development and childhood to adulthood involving biological, cognitive, and socio-emotional changes. The iron requirement increases in adolescence, both in young men and women. Young women require a high iron intake to replace the loss during menstruation. In addition, young women’s attention to their ideal body shape is very high, so young women often limit their food intake. An unbalanced diet with nutrient requirements results in a lack of essential nutrients, such as iron 21-23.
Adolescent girls are usually very concerned about body shape, which limits and restricts food consumption. When food intake is less than iron stores, iron levels drop. Anemia can cause teens to quickly be tired, and learning concentration decreases, resulting in low learning achievement and decreased productivity. Moreover, it lowers the immune system, making it susceptible to infection. If not treated properly, the high prevalence of anemia among adolescents will continue and contribute greatly to the incidence of anemia at the time of pregnancy 19,23-25.
Anemia in pregnant women is a health problem worldwide, especially in developing countries. The World Health Organization (WHO) reports that the prevalence of pregnant women experiencing iron deficiency is around 35-75% and increases with gestation. According to the WHO, 40% of maternal mortality in developing countries is related to anemia during pregnancy, and most anemia in pregnancy is caused by iron deficiency and acute bleeding, even less so in the two who interact 4,26,27.
Efforts to prevent anemia in pregnant women have been made with iron supplementation during pregnancy; however, the results are unsatisfactory, which is low and cannot be replaced by a daily iron-based diet alone or by taking iron supplements alone during pregnancy. In theory, iron supplements should be administered before pregnancy to anticipate a decrease in body iron reserves. This failure may be due to low iron stores that are empty before pregnancy (preconception), especially in developing countries. Therefore, iron supplementation during pregnancy is insufficient to prevent anemia 28-32.
Cases of anemia in adolescents and the phenomenon of increasing early marriage (married youth) in the community affect the incidence of anemia in pregnant women. For this reason, it is necessary to conduct a program for giving iron tablets to adolescents before pregnancy (preconception) based on the results of the discussions (FGD) that have been conducted. Adolescence is associated with anemia and malnutrition during pregnancy. From the results of in-depth interviews and focus group discussions, it was found that unhealthy eating patterns during pregnancy caused a lack of iron intake. Lack of knowledge and skills of pregnant women in providing healthy food during pregnancy is a major factor causing anemia, in addition to economic factors. Pregnant women are one of the groups most vulnerable to malnutrition because of the increased nutritional need to meet the needs of the mother and fetus. A wrong diet in pregnant women has an impact on the occurrence of nutritional disorders, including anemia 13,24,33.
The sources of iron are animal foods, such as meat, chicken, and fish. Other good sources include eggs, mashed cereals, nuts, green vegetables, and fruits. In addition to the amount of iron, the quality of iron in food is also known as its bioavailability. In general, iron in meat, poultry, and fish has high bioavailability; iron in cereals and legumes has moderate bioavailability; and iron in most vegetables, especially those containing high oxalic acid, such as spinach, has low biological availability. It is necessary to pay attention to the combination of a daily diet consisting of a mixture of iron sources from animals and plants as well as other sources of nutrients that can help absorb resources. The food menu in Indonesia should consist of rice, meat/chicken/fish, nuts, and vegetables and fruits rich in vitamin C 13,34-37. The results of the study found that pregnant women rarely consume meat because of the high price and lack of meat availability in food stalls.
The results of in-depth interviews found that the daily intake of iron from food was very small, and the informants also did not consume iron tablets provided by midwives; these are two factors to contribute to the occurrence of anemia in pregnant women. Based on the FGD and adjusted to the theory and research results of Fatima (2011), Ojofeitimi EO (2008), and Soeliastioningsih (2020), several things need to be done to overcome the problem of anemia in this research locus, namely 11,34,37: The dose of iron supplementation is adjusted according to the level of iron kinetics (ferritin and transferrin saturation); adjusting a balanced diet based on the food pyramid so that macronutrient and micronutrient needs can be met; increasing the consumption of food sources of iron, especially from animal protein; increasing the consumption of foods that can increase the solubility and bioavailability of iron, such as vitamin C; limiting the consumption of foodstuffs that can inhibit iron absorption, such as foods containing polyphenols or pitat; taking iron and folic acid supplements before pregnancy is planned for at least 3 months and provision of nutrition education during preconception.
The results of in-depth interviews with informants revealed that they did not know the benefits of consuming Fe tablets, the number that must be consumed during pregnancy, and the side effects of consuming Fe tablets. The informants also stated that the iron tablets received were drugs, and they interpreted anemia as a measure a blood pressure measurement that is checked during every antenatal care examination. If their blood pressure is normal, they do not have anemia. The results of the FGD showed that midwives also lacked communication/health education for pregnant women when giving Fe tablets. According to the Ministry of Health (2002), iron supplementation must be accompanied by information or education about anemia 38. This is to increase the knowledge of pregnant women about anemia and Fe tablets so that they want to consume iron (Fe) tablets. Changes in a person’s behavior are based on knowledge 24,33.
Many studies have indicated that factors such as education, age at marriage, socioeconomic status, poor knowledge, lack of birth spacing, and history of anemia before pregnancy are significant determinants of anemia. Another study on influence of awareness and attitude about anemia in South India found that, in women in rural areas misconceptions regarding oral iron intake and lack of counseling by health workers were significant predictors of anemia 39-41.
Conclusion
Pregnant women have anemia before they become pregnant. Adolescent eating habits (preconception), such as limiting food intake and favorite foods, continue during pregnancy. The diet of pregnant women, which does not reflect a varied and balanced diet, causes an iron deficiency. People often prefer to drink coffee and tea when eating. Lack of knowledge and compliance of pregnant women in consuming iron tablets and lack of health education by midwives when administering iron tablets to pregnant women exacerbate the problem of anemia in pregnant women. Guidelines for administering iron tablets to pregnant women have not been implemented, and there is a lack of evaluation and monitoring of the implementation of blood supplement tablets.
Limitations of the study were as follows: the reference to anemia was only associated with anemia caused by lack of iron, other causes of anemia were not considered, and women could have anemia due to another etiology such as hemoglobinopathies or a deficit of other elements such as folic acid. Conclusions were only drawn based on the given by the informants, which can be very limiting. Some information may not be complete, and other limitations that the study may have given are that it is a qualitative analysis.
Acknowledgments
We would like to thank the Ministry of Health of the Republic of Indonesia for funding this research. We also thank the research informants who shared their stories so openly and frankly. The author comes from Indonesia and is a native Indonesian, who is not familiar with Portuguese. If the author has many writing errors, we apologize and ask for help. Thank you for your generosity. This issue is very important in Indonesia and also has an impact on the high number of stunting cases. Prevention programs that have been carried out by the government have not shown a significant impact.
Statement of Ethics
Informed consent was submitted to the prospective informant. The researcher explains the aims and objectives of the research. Researchers ensure the confidentiality of all information provided by informants and are only used for research purposes. We confirm all personal/identifying information has been removed or disguised so that the person described cannot be identified and cannot be identified through the story details. Prospective informants who are willing have signed the consent form. And prospective informants are not willing; researchers do not compel and respect the rights of prospective informants. Before the implementation of the study, the researcher had obtained ethical clearance approval from the Medical Ethics Commission of the Politeknik Kesehatan RI Medan, Indonesia.