Introduction
Terra firma-forme dermatosis (TFFD), also referred as Duncan’s dirty dermatosis, is a benign dermatological condition characterized by the presence of asymptomatic hyperpigmented plaques, with a “dirt-like” appearance. (1,2 These lesions are persistent and cannot be removed by conventional washing with water and soap. However, they are easily cleared with 70% isopropyl alcohol. (2-4 Although common, TFFD is relatively unknown among medical practitioners, as most cases go unreported or are misdiagnosed. (2 We herein present two cases of this condition.
Case Reports
Case 1
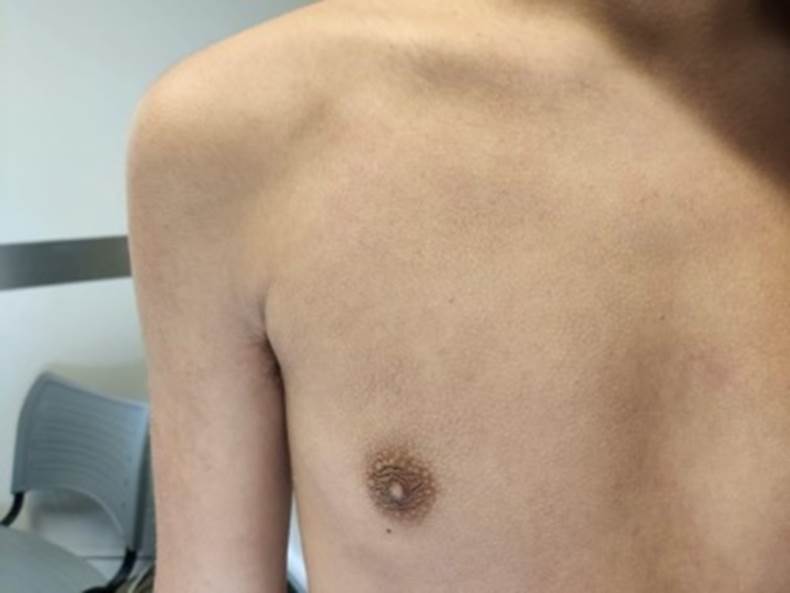
A 14-year-old boy presented to our consultation for the assessment of a persistent, brown-colored skin lesion, located on his upper chest, which had appeared one year earlier. He had no other associated symptoms, including pruritus. The patient’s past medical record was unremarkable. He maintained a regular hygiene, was non-atopic and was not receiving any medication. He had been previously medicated with ketoconazole topical gel, with no improvement. Physical examination revealed a hyperpigmented plaque on his upper chest (Fig. 1), and no other abnormal findings.
Given the appearance of the lesion, we considered TFFD as a possible diagnosis. We proceeded to wipe the affected area with a gauze immersed in 70% isopropyl alcohol, which cleared the lesions, revealing skin of a normal appearance underneath the treated area (Fig. 2). We confirmed the diagnosis of TFFD and instructed the patient to repeat this procedure in case of recurrence.
Case 2
A 13-year-old girl was referred to our consultation with complaints of menstrual irregularities (frequent metrorrhagias). Her menarche had occurred 8-months prior. She had been previously observed by her assistant physician, was diagnosed with iron-deficient anemia, and was subsequently medicated with oral iron supplements. Her gynecological ultrasound was normal, with no record of polycystic ovaries. Her remaining past medical record was unremarkable. On physical examination she presented with a body mass index of 26.86 kg/m2 (above the 97th percentile, according to the World Health Organization charts), which constitutes obesity. She had mild acne and noticeable hyperpigmentation over the lateral and posterior surfaces of the neck (Fig. 3) and axillae. There were no signs of hirsutism. When questioned, the patient mentioned that the skin changes had begun approximately one year earlier. Both the patient and her mother referred that these lesions were a cause of great psychological distress and bullying, as they were perceived as being the result of poor hygiene. The patient’s laboratory study revealed mild hypertriglyceridemia (158 mg/dL) and insulin resistance (HOMA-IR of 5.9), with normal fasting glucose and a HbA1c of 5.7%. Given the presence of obesity, insulin resistance and the location of the hyperpigmented plaques, the main hypothesis for the lesions described was acanthosis nigricans. Nonetheless, we performed swabbing of the affected regions with 70% isopropyl alcohol, which immediately cleared the skin, thus confirming the diagnosis of TFFD (Fig. 4).
Discussion
TFFD was originally described in 1987, by Duncan and colleagues, who firstly identified this dermatosis, giving it its Latin name for its “dirt-like” appearance. (1 Although common, TFFD is rarely described in the medical literature and remains relatively unrecognized among medical practitioners.5
This dermatosis occurs with higher frequency among children and teenagers, with equal incidence in both sexes.1,2,4,6 In a recent retrospective study published by Aslan et al, in a series of 79 patients with TFFD, 88.6% were children, with an average age of 10 ± 7.5 years. (7 Both our reported cases fall in this age group. The condition is characterized by the presence of persistent, asymptomatic, brown-colored plaques, frequently in multiple localizations (most commonly, the face, neck and torso).2,7,8
In terms of etiology, it is currently accepted that TFFD is the result of an abnormal keratinization process, with incomplete development of the keratin squames, leading to the retention of keratinocytes within the epidermis.4,5,9 Sunlight exposure has been identified as a possible triggering factor.1,3) However, this does not explain the onset of TFFD in non-sun exposed areas. Some authors postulate that other factors, such as an increased perspiration, may also contribute to the development of TFFD.5 There also seems to be a greater incidence of this pathology among individuals with concomitant atopic dermatitis.3,5
The diagnosis of this entity is clinical.1) Dermatoscopy is rarely needed, but if performed, the examination of the lesions would reveal multiple polygonal brown scales, organized in a cobblestone pattern.4,5) Treatment is performed by rubbing the lesion with 70% isopropyl alcohol. Since TFFD is a retention hyperkeratosis, other keratolytic agents (such as salicylic acid, alpha-hydroxy acid, topical retinoids or even lemon juice) have also proven to be effective.10
TFFD main differential diagnoses are dermatosis neglecta and acanthosis nigricans.3,5,9 Dermatosis neglecta, as the term implies, results from a neglected hygiene, whereas in TFFD patients maintain adequate washing habits.2,9) Clinically, in dermatosis neglecta, there is successful removal of skin lesions with soap and water, which is not seen in TFFD.2 Acanthosis nigricans is also an important differential diagnosis, as its lesions are usually located on similar sites of those associated with TFFD.2,5 This condition is frequently associated with obesity and insulin resistance, which was the case of patient 2. However, in acanthosis nigricans, the lesions cannot be removed with 70% isopropyl alcohol, which clarified the diagnosis of our patient.2 Other differential diagnoses include the ‘dirty neck syndrome’ of atopic dermatitis, confluent and reticulated papillomatosis (Gougerot-Carteaud syndrome), seborrheic keratosis, tinea versicolor and epidermal nevi.2,4
In conclusion, TFFD is a benign, easily resolved dermatosis. Nonetheless, its unesthetic appearance, which may be perceived as the result of poor personal hygiene, is often a cause of great distraught to the patients and their families. TFFD is treated instantly after rubbing the lesions with 70% isopropyl alcohol. This simple gesture serves as both a diagnostic sign and treatment. We believe that the reported cases can lead to further awareness of this entity, preventing futile referrals, exams and treatments and, ultimately, avoid unnecessary anxiety and distress.