Introduction
Cancer has a major impact across the world and is among the leading causes of death worldwide with 9.6 million deaths in 2018 (World Health Organization, 2018). The diagnosis of chronic disease is a factor of rupture, loss, and intense psychological disorganization. The oncological disease remains a threat with a devastating impact on human life, as it is a pathology that transcends the physical, private, personal, and family domains (Castro et al., 2011; Chaves & Simães, 2018). Patients with cancer often experience many psychological disturbances such as anxiety, depression, confusion, and memory problems (Fann et al., 2008; Tang et al., 2017; Zabora et al., 2001). Emotional distress after a diagnosis of cancer is common as well as doubts and fears about the future, pain, fatigue, and sleep disturbances (Hoffman et al., 2007). Physical symptoms or functional losses resulting from the disease or its treatment are among the triggering factors (Speca et al., 2000).
Over the years, nonpharmacological complementary therapies, such as psychological counseling and hypnosis, have been found to reduce psychological symptoms in health care applications (Fischer & Wedel, 2012; Newell et al., 2002; Weisberg, 2008). Hypnosis has always been a controversial issue and its medical use is also controversial (Green et al., 2005).
The definition of hypnosis is fundamental to scientific inquiry, but the endeavor to define hypnosis from differing theoretical perspectives has given rise to controversy as to the “real” meaning of hypnosis (Elkins et al., 2015; Green et al., 2005). Some researchers believe that hypnosis is related to an altered state of consciousness while others assume that this phenomenon can be explained by clinicians/patients’ expectations (Vanhaudenhuyse et al., 2014). Although the controversy prevails, hypnosis occupies the 30th division of the American Psychological Association (APA), where it is defined as “a procedure during which a health professional/researcher suggests to a client/patient, in an investigation, changes in their subjective sensory-perceptual experience thoughts and behaviors” (Kirsch, 1994, p. 143).
In 2014, to solve the definition problem of hypnosis, an APA executive committee reached a consensus for a definition of hypnosis that would solve the controversy surrounding the old definition. In this way, Elkins et al. (2015) published an article in the American Journal of Clinical Hypnosis that revised the concept: “A state of consciousness that involves focused attention and reduced peripheral awareness, characterized by a greater capacity to respond to the suggestion” (p. 6). It remains difficult to provide an optimal definition of hypnosis but describing hypnosis as a therapeutic intervention during which individuals undergoing relaxation procedures followed by therapeutic suggestions to help with changes in their lives seems to be the main feature of this technique (Flynn, 2018). This definition emphasizes the relationship between the hypnotherapist and the patient as a necessary condition for anyone practicing hypnosis (Flammer & Bongartz, 2003; Montgomery et al., 2011). Another fact of controversy is the methodological limitations including underpowered sample sizes and lack of reporting of the method of randomization in the Randomized Controlled Trial (RCT) studies available (Newell et al., 2002; Richardson et al., 2006).
Although there are still conceptual and methodological problems in the study of hypnosis, in the last few decades, there have been multiple studies that eliminated some myths. Recently, hypnosis has generated interest in managing cancer symptoms (Chen et al., 2017; Cramer et al., 2015). Some studies have highlighted the importance of hypnotic procedures in the management of stress and pain and minimizing the side effects of chemotherapy and radiotherapy (Berlière et al., 2018; Forester-Miller, 2017). APA (Elkins et al., 2015; Green et al., 2005) acknowledges that although the use of hypnosis for medical purposes has been controversial, clinicians now agree it can be an effective technique for many conditions, including anxiety, mood disorders, chronic pain (Flynn, 2018; Plaskota et al., 2012; Snow et al., 2012), allergies, hypertension, nausea, enhancing positive emotions (Schnur et al., 2009), and quality of life (Álvarez & Uribe, 2016; Castañeda & Krikorian, 2018; Flynn, 2018; González-Ramírez et al., 2017).
Although several literature reviews have been conducted regarding the efficacy of psychological interventions for cancer patients, no reviews have specifically looked at the efficacy of hypnosis interventions. The present review aims to summarize and assess the evidence regarding the efficacy that hypnosis has on treatment, treatment side effects, and what type of interventions have been most used and by whom.
In this literature and integrative review, the authors intend to answer three central questions: (a) Who are the health professionals who use hypnosis? (b) What interventions, within the scope of hypnosis, have been performed on cancer patients? And what effects does hypnosis provide?
Method
This review was conducted on a range of databases and was guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses, PRISMA (Shamseer et al., 2015).
Search strategy
A comprehensive search was carried out. This review was conducted on a range of databases and following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Moher et al., 2009). All searches covered articles about the use of hypnosis in cancer patients published between 2012 and 2019, using B-on, SciELO, MEDLINE, and Web of Science databases.
The relevant literature was searched using groups of keywords: Hypnosis-related keywords (e.g., “hypnosis”, “hypnotherapy”, hypnot*), cancer-related keywords (e.g., cancer*, tumor). Also, other terms were associated with these combinations to further specify the search, such as “treatment” and “patients”. After removing duplicates, the remaining articles were screened by reading the abstracts. Discrepancies were rechecked and discussed until consensus was reached. This screening excluded other articles, leaving articles for full-text evaluation. Abstracts were independently reviewed by the authors to identify articles that meet the criteria for this review. Furthermore, some efforts were made to identify ongoing research and unpublished studies.
Study selection
Each study satisfied the following criteria according to:
Types of studies: Empirical studies peer-reviewed of patients with a diagnosis of cancer (children and adults) published in English.
Types of intervention: An intervention using hypnosis or hypnosis combined with other psychological interventions.
Types of the control group: Standard care control group or a single group.
Exclusion criteria
Regarding the exclusion criteria, articles prior to 2012; publications that only addressed one of the study variables (hypnosis or cancer); articles published in other languages, other than in English, Portuguese or Spanish; studies where the intervention was focused exclusively on self-hypnosis; systematic reviews, meta-analysis, thesis and conference abstracts were rejected.
Results
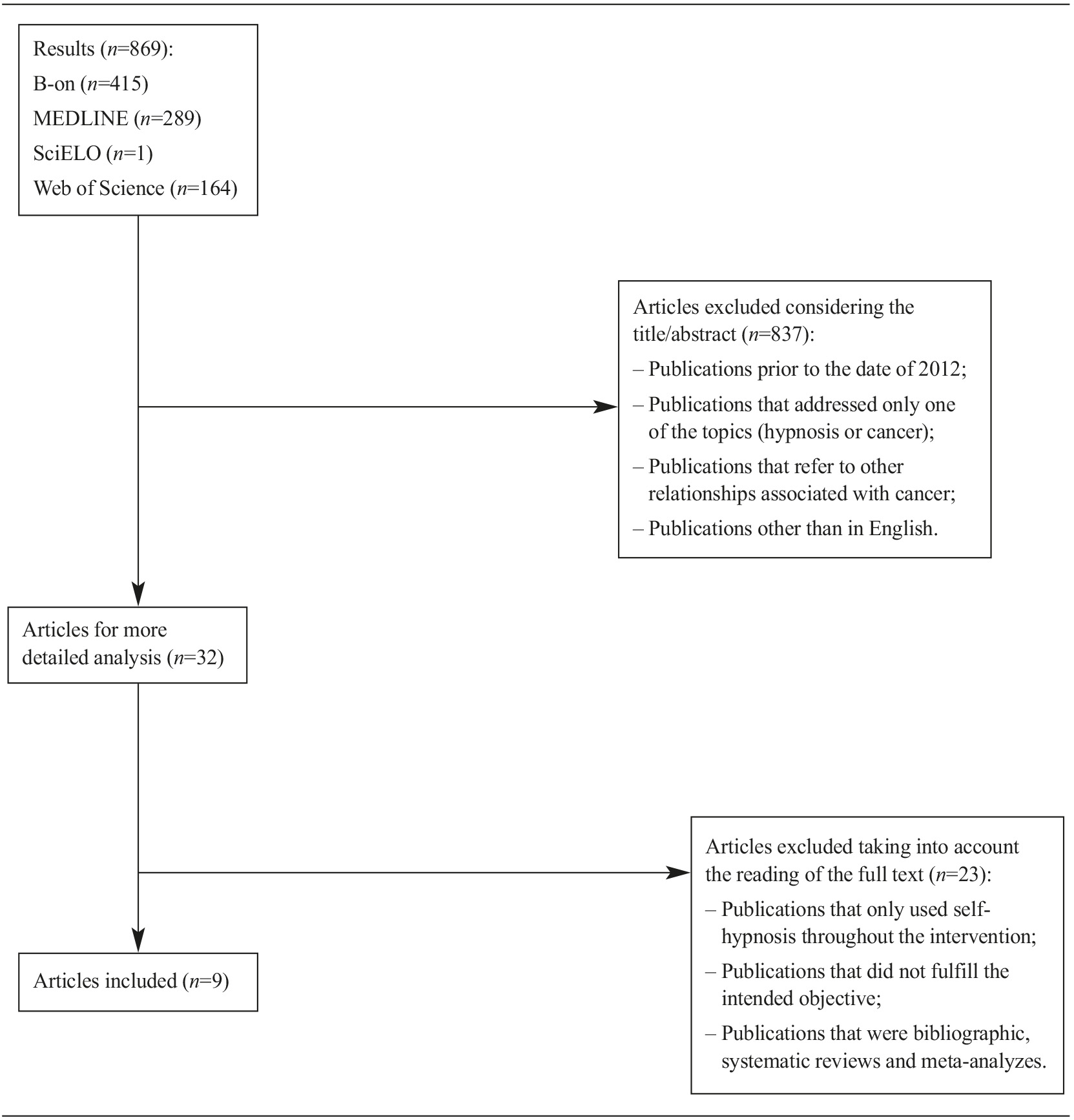
The literature search yielded 869 papers (including manual searching) for evidence on the efficacy of hypnosis in cancer patients. After removal of duplicates and excluding studies based on their abstracts or through examining their full text, nine papers were identified as eligible for inclusion, published between 2012 and 2019, focusing on the effects that hypnosis had on the treatment and side effects of cancer (Berlière et al., 2018; Grégoire et al., 2018, 2019; Johnson et al., 2016; Montgomery et al., 2017; Plaskota et al., 2012; Snow et al., 2012; Sterkers et al., 2018; Zemmoura et al., 2016) (Figure 1).
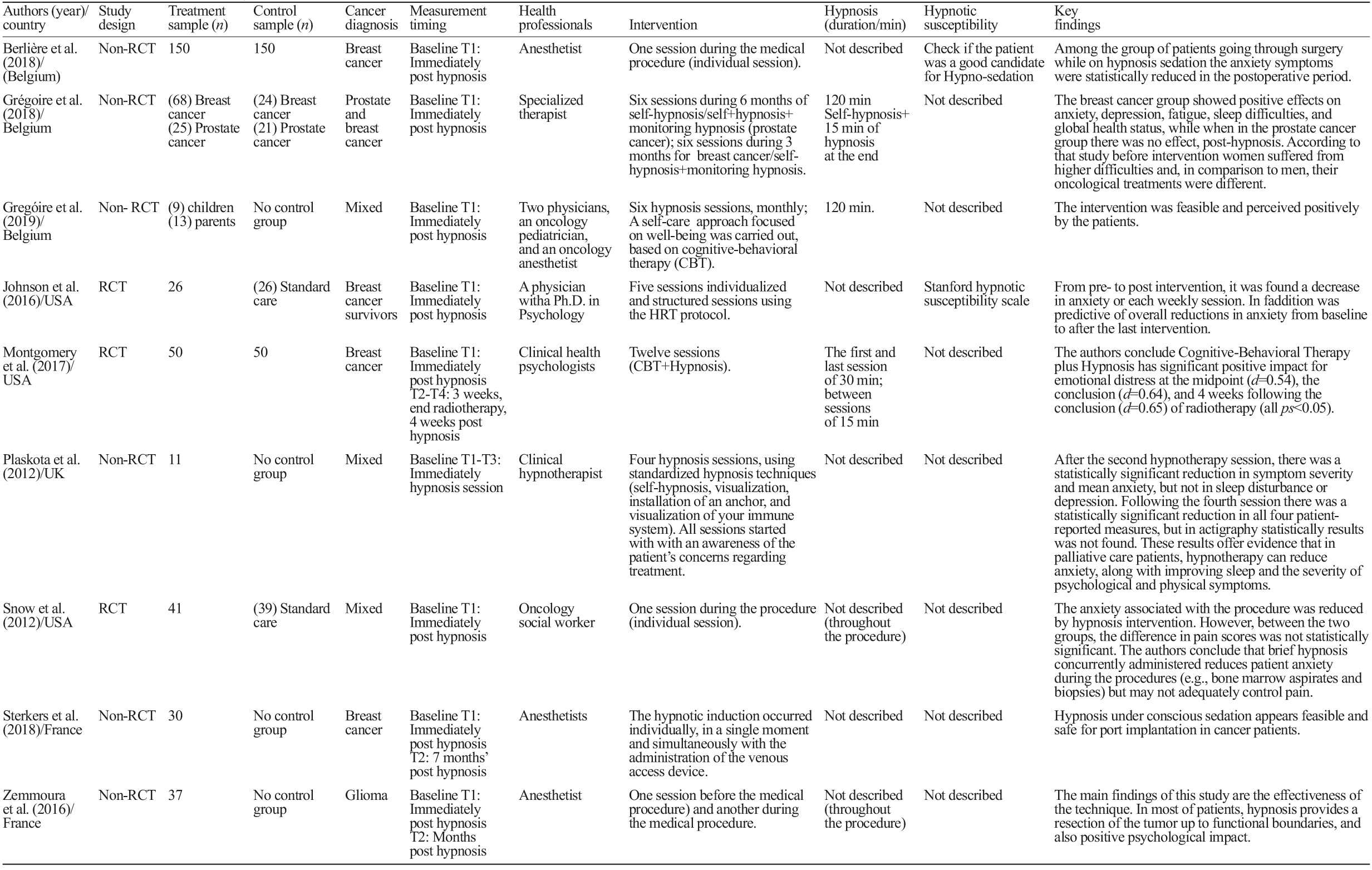
Table 1 presents the description of the nine studies based on the characteristics of participants, research design, settings, outcome measurements, were analyzed (Table 1).
Study characteristics
Country. From the nine studies, three were conducted in the United States (Johnson et al., 2016; Montgomery et al., 2017; Snow et al., 2012), three in Belgium (Berlière et al., 2018; Grégoire et al., 2018, 2019), two in France (Sterkers et al., 2018; Zemmoura et al., 2016), and one in the United Kingdom (Plaskota et al., 2012).
Studies characteristics. Three studies were RCT (Johnson et al., 2016; Montgomery et al., 2017; Snow et al., 2012) and six were single-group studies that did not randomize patients (non-RCT) (Berlière et al., 2018; Grégoire et al., 2018, 2019; Plaskota et al., 2012; Sterkers et al., 2018; Zemmoura et al., 2016). The RCT studies used a standard care control group (Johnson et al., 2016; Snow et al., 2012). The nine studies had a longitudinal design and two of these nine studies applied hypnosis during surgery (Berlière et al., 2018; Zemmoura et al., 2016).
Patient characteristics
Gender. In terms of gender, five studies used mixed samples (Grégoire et al., 2018, 2019; Plaskota et al., 2012; Snow et al., 2012; Zemmoura et al., 2016) and four used only women (Berlière et al., 2018; Johnson et al., 2016; Montgomery et al., 2017; Sterkers et al., 2018), one of the studies the sample included children and adults (Grégoire et al., 2019).
Cancer diagnosis. The majority of studies included breast cancer (five) (Berlière et al., 2018; Grégoire et al., 2018; Johnson et al., 2016; Montgomery et al., 2017; Sterkers et al., 2018) but four studies included patients with other cancers (Grégoire et al., 2018; Grégoire et al., 2019; Plaskota et al., 2012; Snow et al., 2012), and in one study patients were diagnosed with cerebral neoplasms with a higher grade of malignancy (Zemmoura et al., 2016).
Number of participants. Sample sizes were very different, with a minimum of 11 mixed cancer patients (Plaskota et al., 2012), and a maximum of 300 breast cancer patients (Berlière et al., 2018).
Cancer symptoms. Anxiety was addressed in eight studies (Berlière et al., 2018; Grégoire et al., 2018, 2019; Johnson et al., 2016; Montgomery et al., 2017; Plaskota et al., 2012; Snow et al., 2012; Sterkers et al., 2018), followed by depression (four studies) (Grégoire et al., 2018; Montgomery et al., 2017; Plaskota et al., 2012; Snow et al., 2012), fatigue (4 studies) (Berlière et al., 2018; Grégoire et al., 2018, 2019; Montgomery et al., 2017), pain (five studies) (Berlière et al., 2018; Grégoire et al., 2019; Snow et al., 2012; Sterkers et al., 2018; Zemmoura et al., 2016), and sleep distubance (three studies) (Grégoire et al., 2018; Plaskota et al., 2012; Sterkers et al., 2018). In addition other variables were also analyzed, including: global health status (Grégoire et al., 2018); stress (Zemmoura et al., 2016); self-esteem and self-confidence (Grégoire et al., 2018, 2019); tension, anger, confusion and activity level (Montgomery et al., 2017); quality of life (Grégoire et al., 2019); nausea and vomiting (Berlière et al., 2018); tolerance and satisfaction with hypnosis (Sterkers et al., 2018); and presence of post-traumatic stress disorder (PTSD) (Zemmoura et al., 2016).
Psychological assessment
The outcome measures differed among the nine studies. Three studies used a questionnaire designed specifically for the research (e.g., common beliefs about hypnosis, participants’ satisfaction with the intervention) (Berlière et al., 2018; Grégoire et al., 2019; Sterkers et al., 2018). One of the studies used a wrist actigraph unit to obtain objective sleep data that measures and records movement over time in the form of activity counts (Plaskota et al., 2012). In three studies the Hospital Anxiety and Depression Scale (HADS) was used (Grégoire et al., 2018; Johnson et al., 2016; Plaskota et al., 2015). In addition, more specific scales were used to better analyze the desired variables. Grégoire et al. (2018) study used the European Organization for Research and Treatment of Cancer - Quality of Life Core Questionnaire-30 (EORTC-QLCQ30) and the Insomnia Severity Index (ISI); Johnson et al. (2016) study used the Numeric Visual Analog Scale for Anxiety (NVAAS) and Stanford Hypnotic Clinical Scale (SHCS); Montgomery et al. (2017) study used (Shortened Version of the Profile of Mood States (SV-POMS); Plaskota et al. (2012) study used the Edmonton Symptom Assessment System (ESAS) and the Verran and Snyder-Halpern Scale (VSH); Snow et al. (2012) used Visual Analog Scales (VAS) and the State Trait Anxiety Inventory (STAI); Zemmoura et al. (2016) study used the Cohen Perceived Stress Scale (PSS), the Posttraumatic Stress Disorder Checklist Scale (PCLS), and the Peritraumatic Dissociative Experience Questionnaire (PDEQ).
Health professionals
The majority of health professionals who used hypnosis were anesthesiologists (four studies) (Berlière et al., 2018; Grégoire et al., 2019; Sterkers et al., 2018; Zemmoura et al., 2016). However, hypnosis was also applied by a specialized therapist (Grégoire et al., 2018), an oncology pediatrician (Grégoire et al., 2019), clinical psychologists (Montgomery et al., 2017), a clinical hypnotherapist (Plaskota et al., 2012), and an oncology social worker (Snow et al., 2012).
Intervention
Concerning the type of intervention, three studies used a one-session of hypnosis (Berlière et al., 2018; Snow et al., 2012; Sterkers et al., 2018), and the remaining used several sessions ranging from two (Zemmoura et al., 2016) to 12 (Montgomery et al., 2017), with four of these studies being administered individually (Berlière et al., 2018; Snow et al., 2012; Sterkers et al., 2018; Zemmoura et al., 2016) and the remaining in a group format (Grégoire et al., 2018; Grégoire et al., 2019; Johnson et al., 2016; Montgomery et al., 2017; Plaskota et al., 2012).
Some studies described the use of hypnosis in combination with other techniques such as cognitive-behavioral therapy (CBT) (Grégoire et al., 2018; Montgomery et al., 2017). Another study used, the Hypnotic Relaxation Therapy (HRT) protocol (Johnson et al., 2016) and two studies used self-hypnosis with other techniques such as visualization, creation of an anchor, and visualization of the immune system (Grégoire et al., 2018; Plaskota et al., 2012). All nine studies regarding the information on hypnosis described the use of the technique ranging between 15 to 120 minutes each session.
Psychological and clinical outcomes
After the intervention, the results in six studies showed a reduction in anxiety (Berlière et al., 2018; Grégoire et al., 2018; Johnson et al., 2016; Montgomery et al., 2017; Plaskota et al., 2012; Snow et al., 2012). Positive effects in relation to the variables, depression (four studies) (Grégoire et al., 2018; Montgomery et al., 2017; Plaskota et al., 2012; Snow et al., 2012), fatigue (four studies) (Berlière et al., 2018; Grégoire et al., 2018, 2019; Montgomery et al., 2017), pain (four studies) (Grégoire et al., 2018, 2019; Sterkers et al., 2018; Zemmoura et al., 2016), difficulty to sleep (two studies) (Grégoire et al., 2018; Plaskota et al., 2012), global health status (Grégoire et al., 2018) and quality of life (Grégoire et al., 2019). Additionally, a study that used hypnosis combined with CBT, showed benefits in terms of emotional distress (Montgomery et al., 2017).
Other studies found an improvement in attitudes towards hypnosis and treatment (Grégoire et al., 2019; Sterkers et al., 2018; Zemmoura et al., 2016). In addition, one study found that children reported that hypnosis improved their learning strategies to cope with negative emotions, to relax, to respect themselves, and to be more assertive (Grégoire et al., 2019). One of the studies concluded that hypnosis reduced the length of hospitalization time, a reduction in lymphatic production, nausea and vomiting (Berlière et al., 2018), and hot flashes (Berlière et al., 2018; Johnson et al., 2016). One study indicated no significant reductions in pain (Snow et al., 2012), and in another study (Grégoire et al., 2018) men with prostate cancer reported no improvement in fatigue and insomnia.
Discussion
This review of the literature aimed to summarize and assess the evidence regarding hypnosis in cancer patients. The studies included in this review found that hypnosis reduced anxiety, depression, fatigue, and pain, and improved sleep difficulties and quality of life. The positive effect of hypnosis found in this study is consistent with previous studies of hypnosis effects for cancer patients receiving medical procedures (Álvarez & Uribe, 2016; Castañeda & Krikorian, 2018; Flynn, 2018; González-Ramírez et al., 2017; Plaskota et al., 2012; Schnur et al., 2009; Snow et al., 2012). The results extending the positive effect of using hypnosis in cancer patients, suggesting that this clinical intervention is valuable not only in relieving medical procedures, but also in reducing symptomatology by cancer patients after treatment (Chen et al., 2017; Cramer et al., 2015). Although there were few studies included, these results are in line with previous research, which showed the effectiveness of hypnosis in providing suggestions for the body to accept and improve the side effects of medical interventions, leading to greater adherence to treatments (Forester-Miller, 2017).
Studies have been developed mainly across western countries and did not include patients from Hispanic, Asian, or African’ origins. Therefore, generalizations need to be cautious due to possible cultural differences. More studies are needed about the effect of hypnosis on cancer, in different cultures. A large number of the studies reviewed were performed in western countries, with adults. However, one of nine included studies used a child population (Grégoire et al., 2019). In the future, these differences in target populations should be further studied.
In most studies, interventions focused on breast cancer patients and three studies used mixed cancer patients (Grégoire et al., 2019; Plaskota et al., 2012; Snow et al., 2012). Little is known about how useful these interventions would be in patients with different tumors and/or in male cancer patients, in general. One of the studies showed precisely that the hypnosis intervention was successful in reducing fatigue and sleep difficulties in women with breast cancer but not in male patients with prostate cancer (Grégoire et al., 2018). It is not known whether the results were due to gender or the type of cancer. Although one may expect that the results could be generalized to other cancer patients, more research including male patients and patients with different tumors need to be performed.
Only three of the nine included studies reported hypnosis duration. Further studies are needed to identify the best duration of a hypnosis session. Moreover, the studies did not address differences between the immediate and the sustained effects of hypnosis. According to the results, hypnosis seems to be more effective in the short term than in the long term. Nonetheless, only three in nine studies reported follow-up assessments. Hypnosis appeared to have, not only an immediate effect in reducing psychological and physical symptomatology (Newell et al., 2002), but the effect was also sustained (Chen et al., 2017; Cramer et al., 2015).
One key aspect that studies did not report was standard practice i.e., what cancer hypnosis protocol was being used and whether it was used alone or with other clinical interventions. Standard practice interventions for cancer-related procedures vary, depending on context and country. Inadequate reporting of the duration, content, and context of the hypnosis session (session duration and frequency) in some studies presents a challenge for study replication and comparison between interventions (Newell et al., 2002; Richardson et al., 2006). However, it has been suggested that hypnosis can be used as an adjunct to pharmacological interventions for pain control and distress management and in preparation for procedures such as general anesthetic (Liossi & Hatira, 2003).
Another limitation of the study is the heterogeneity of the studies included in the present review. There was some diversity concerning professionals who used hypnosis. One is left wondering which professionals are well placed to provide such supportive intervention and whether the success of hypnosis is due to its process or to the experience and training of the therapist.
The studies also revealed heterogeneity regarding the stage of the oncological disease, including patients undergoing current treatment, disease in remission, survivors or in advanced disease. In addition, the interventions used, in some cases, were mixed, so the results of the effects of hypnosis should be interpreted with caution. The studies described divergent procedures, some of which combined hypnosis with other techniques, namely, Cognitive-Behavioral Therapy (CBT) (Grégoire et al., 2018; Montgomery et al., 2017), the Hypnotic Relaxation Therapy (HRT) protocol (Johnson et al., 2016) and self-hypnosis (Grégoire et al., 2018; Plaskota et al., 2012). This suggests that hypnosis is controversial in nature and also harbors a considerable number of approaches and, as a result, becomes difficult to determine the efficacy of hypnosis as a single intervention.
The heterogeneity of the studies found may be explained by the difficult application of longitudinal methodologies of hypnosis, namely in cancer patients. Furthermore, cancer itself is a very heterogeneous disease. Cancer includes numerous particularities such as the communication experience of the diagnosis, the type of cancer, the stage of the disease, the type of treatment, the physical side effects and the psychological distress associated. The protocols must consider each specificity of the cancer disease, otherwise it is difficult to assess its efficacy.
The results seem to suggest that hypnosis is a useful therapeutic tool in improving the physical and psychological symptoms of cancer patients, but future randomized studies should be carried out in this context. Randomization is a more robust methodology commonly used to assess the efficacy of intervention programs (Bhide et al., 2018). In this review, only three (Johnson et al., 2016; Montgomery et al., 2017; Snow et al., 2012) of the nine studies used this design, and also with unclear protocols. A more structured and focused design of the investigations would be important, so that it is possible to overcome contradictions, inconsistencies and limitations and create more specific consensual protocols, appropriate to the particularities and specificities of this disease. In addition, measuring suggestibility to hypnosis at the beginning of each procedure is clinically relevant as it may help identify patients who might respond readily to hypnosis from those who may require additional training or support.
Limitations
Although the results found were relevant, this review has some limitations that need to be acknowledged. The first limitation corresponds to the small sample size, in this study only nine studies were included, which shows that the effects that hypnosis has on the treatment and side effects of cancer remain poorly studied. The second limitation relates to the small sample of most of the used studies and non-randomly assigned, which may limit the representativeness of the results to the remaining population. The control groups were rather heterogeneous, including the standard care group as well as the comparison treatment groups. Even if only standard care was included for the control-group analysis, the actual “standard” care might differ due to cultural differences or unit-related characteristics in different countries. Hypnosis may have a higher effect size when compared to standard care than when compared to other treatments. Also, some of the studies used CBT along with hypnosis, making it difficult to analyze the impact of hypnosis on the participants. Finally, the majority of the studies did not measure hypnotizability, a factor associated with the effect of hypnosis (Chen et al., 2017; Flynn, 2018).
Conclusions
This review provides a significant contribution to the literature and identifies some important implications for clinical practice and future research. Further studies are needed to examine the impact of hypnosis on cancer treatment and side effects, as only nine studies have been found. While more research is needed to underpin the results found in this review, the studies showed a positive impact of hypnosis on cancer patients. The findings suggest that hypnosis is used by a variety of different professionals showing interest in the technique and could contribute to the management of cancer-related procedures and the reduction of a set of symptoms after treatment. The findings may help to inform clinical practices and be used to improve the quality of the methodology of hypnosis interventions, in cancer patients.
Further research into the efficacy, feasibility, and safety of hypnosis for cancer patients with comparisons of age, developmental, sex, and type of cancer variables is recommended. Such evidence will assist in the formulation of evidence-based practice guidelines for using psychological interventions to prepare patients for invasive procedures.