Introduction
Definition and prevalence of non-suicidal self-injury in the context of eating disorders
Non-suicidal self-injury (NSSI) is a deliberate self-inflicted damage to the body without suicidal intent (Klonsky et al., 2011) and it is associated with different forms of mental illness including eating disorders (ED). According to a meta-analysis published by Cucchi et al. (2016), the average percentage of patients with a lifetime history of NSSI was 21.8% for anorexia nervosa (AN) and 32.7% for bulimia nervosa (BN). On the other hand, among those with NSSI, 19.4% also reported ED symptoms (Muehlenkamp et al., 2012). NSSI is more frequent in binge-eating/purging-type ED than restricting‐type ED (Davico et al., 2019). Claes and Muehlenkamp (2014) argued that eating disordered behaviors exist on the continuum of harmful acts with NSSI, with a higher frequency of NSSI, a greater variety of NSSI methods, and a medical treatment of NSSI being related to greater ED severity.
According to Claes and Muehlenkamp (2014) the frequent co-occurrence between ED and NSSI is based on common conditions that include the onset in adolescence or early adulthood and a female preponderance, difficulties in emotion regulation (Lavender et al., 2015) and impulsivity (Claes et al., 2015).
Emotion regulation, NSSI and ED
Emotion regulation is a psychological process or capacity involving several dimensions such as awareness or understanding of one’s emotions, acceptance of emotions experienced, behavioral control during negative emotional states, and flexible use of emotion modulation strategies (Gratz & Roemer 2004). The absence of any or all of these dimensions suggests emotion dysregulation (Gratz & Roemer 2004). Recent evidences regarding emotion dysregulation and NSSI showed that higher levels of emotion dysregulation were associated with an increased risk of NSSI) among individuals across different contexts, regardless of age or sex (Wolff et al., 2019; You et al., 2018). Indeed, a predominant function of NSSI seems to be negative reinforcement. NSSI serves to provide relief or escape from emotional distress and help to regulate emotions (Nock & Prinstein 2004). In the same line, the Experiential Avoidance Model of NSSI is based on the idea that NSSI is a negatively reinforced strategy for reducing or ending uncomfortable emotional arousal (Chapman et al., 2006).
Also, ED are linked to emotion dysregulation. Individuals with ED have been found to show higher levels of emotion dysregulation compared to healthy controls, specifically lower levels of emotional awareness, clarity, and recognition (e.g., Lavender et al., 2015; Monell et al., 2018). In addition, Pisetsky et al. (2017) found that cognitively-oriented symptoms of ED were associated with emotion dysregulation. Although less studied than NSSI, evidence indicates that some ED symptoms also serve emotion regulation functions by providing a sense of control over body and emotions states (Lavender et al., 2015).
Moreover, previous research supports the idea that eating disordered behaviors and NSSI may act as inadequate forms to regulate emotions. Indeed, both ED and NSSI provide negative reinforcement in the form of escape from, or distraction from, aversive emotional states (Klonsky et al., 2011).
In sum, there is some evidence of functional equivalence between ED and NSSI. Findings revealed that similar intrapersonal such as affect regulation, and interpersonal functions, such as interpersonal boundaries and autonomy, may be involved in the development and maintenance of both NSSI and ED behaviors (Muehlenkamp et al., 2019) and previous models of NSSI and ED behaviors highlight the role of similar emotion regulation deficits (e.g., Muehlenkamp et al., 2012).
Negative urgency, NSSI and ED
Negative urgency refers to the tendency to act impulsively while experiencing extreme aversive emotions (Whiteside et al., 2005). Individuals with high levels of negative urgency intent to reduce negative affect with specific behaviors such as binge eating or cutting, increasing the likelihood of inadequate behaviors through negative reinforcement pathways (Peterson & Fisher 2012). Therefore, NSSI has been conceptualized as the result of difficulties in impulse control, particularly in response to distress (Favazza 1998; Muehlenkamp et al., 2009). Additionally, in a recent study, negative urgency and difficulties in emotion regulation appeared as predictors of disordered eating and NSSI (Hasking & Claes 2019).
The present study
Taken together, the existing literature indicates a high co-occurrence of ED behaviors and NSSI, as well as a considerable mechanistic similarity between these behaviors. However, it is important to evaluate the meaningful interrelationships between ED, NSSI and some underlying mechanisms in an integrated model. In addition, the same patients with ED and a history of NSSI may experience different clinical symptoms and levels of disordered eating, emotion dysregulation and negative urgency. Therefore, the current study aimed to provide a clinical characterization of patients with ED and lifetime NSSI behaviors when considering eating pathology, emotion dysregulation and negative urgency, to explore empirically the severity of cluster of participants and to investigate how the clinical features and diagnosis were distributed among them. Exploration of the clusters of patients with both ED and NSSI, based on eating pathology, emotion dysregulation and negative urgency is relevant, as it can inform targeted and individualized interventions.
We expect to find distinct clusters of patients with ED who also endorsed in NSSI currently or in the past. Moreover, we hypothesized that eating pathology, emotion dysregulation and negative urgency would differentiate the clusters. We intend to contribute to the study of ED and NSSI considering the role of difficulties in emotion regulation and negative urgency at the presented ED symptomatology and severity, providing a clinical characterization of ED outpatients.
Method
Participants
Participants of the current study were 73 outpatients with ED who reported a history of engagement in NSSI. The age of participants ranged between 14 and 55 years old (M=26.42, SD=9.35) and the mean BMI was 20.30 kg/m2 (SD=5.45). Most participants were women (n=68, 93.2%), single (n=53, 73.6%), students (n=35, 49.3%), had secondary education (n=47, 65.3%) and related current psychiatric medication use (e.g., benzodiazepines and antidepressants; n=61, 83.6%). The distribution of the sample according to diagnostic group was 25 (32.2%) with AN restricting type, 7 (9.6%) with AN binge eating/purging type, 20 (27.4%) with BN, 6 (8.2%) with binge eating disorder (BED), and 15 (20.5%) with other specified ED (OSFED). Forty-five participants (61.6%) reported engaging in NSSI within the previous several months or more than a year ago and 28 (38.4%) had injured themselves during the preceding week or month of the study. On average, participants used more than one method of NSSI (M=2.52, SD=1.43).
Measures
Sociodemographic and Clinical Questionnaire. This questionnaire aims to collect information on gender, age, marital status, education, occupation, psychiatric medication use, weight, height, duration of treatment (months; “How long have you been attending to eating behavior consultations at the Hospital?”) and duration of the ED (months; “How long has your eating problem been?”).
Eating Disorder-15. The ED‐15 (Tatham et al., 2015; Portuguese version Rodrigues et al., 2019) is a brief questionnaire developed to assess eating attitudes over the preceding week through 10 items, using a Likert-type scale ranging from 0 (not at all) to 6 (all the time). Two attitudinal subscales - weight and shape concerns and eating concerns - and a total attitudinal score are obtained. Higher scores suggest greater levels of eating psychopathology. Five additional behavioral items are assessed: binge-eating episodes, self-induced vomiting episodes, laxative misuse days, eating restraint days and excessive exercise days. In this study, Cronbach’s α were as follows: total score, α=.92; weight and shape concerns, α=.90; and eating concerns, α=.81.
Difficulties in Emotion Regulation Scale. The Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer 2004; Portuguese version Coutinho et al., 2010) is a 36-item questionnaire developed to assess difficulties within the following dimensions of emotion dysregulation: limited access to emotion regulation strategies (Strategies); non-acceptance of emotional responses (Non-acceptance); lack of emotional awareness (Awareness); difficulties controlling impulsive behaviors when experiencing negative emotions (Impulses); difficulties engaging in goal-directed behavior when experiencing negative emotions (Goals); and lack of emotional clarity (Clarity). Participants are asked to indicate how often the items apply to themselves, with responses ranging from 1 (almost never) to 5 (almost always). It is possible to obtain a total score (adding all the 36 items) and a score for each subscale. Higher scores indicate greater difficulties in emotion regulation. In this study, we obtained the following Cronbach’s α for the subscales of strategies, α=.92, non-acceptance, α=.92, awareness, α=.80, impulses, α=.91, goals, α=.90, and clarity, α=.80. Cronbach’s α for the total score was .96.
UPPS-P Impulsive Behavior Scale - Negative Urgency Subscale. The UPPS-P Negative Urgency Subscale (Whiteside et al., 2005; Portuguese version Lopes et al., 2013) is a 12‐item subscale that assesses the tendency to engage in impulsive behaviors under negative affect. Items are scored on a 4‐point Likert‐type scale ranging from 1 (agree strongly) to 4 (disagree strongly). Higher scores indicate higher negative urgency. Cronbach’s α in this study was .87.
Self-Injury Questionnaire - Treatment Related. The Self-Injury Questionnaire - Treatment Related (SIQ-TR; Claes & Vandereycken 2007; Portuguese version Gonçalves 2008) is a self-report measure that assesses the presence of five methods of NSSI: scratching, bruising, cutting, burning, and biting (or other). For each method, it is asked how long ago the participant had engaged in this form of NSSI: a week; a month; several months; more than a year; and never.
Procedure
This study was authorized and approved by the University of Minho Ethics Commission‐Subcommittee of Ethics for Social and Human Sciences and the Ethics Committee São João Hospital Centre/Faculty of Medicine, University of Porto. Participants were recruited from an initial and larger sample of patients with ED. Data collection took place in a public psychiatric service that provides specialized treatment for ED in the north of Portugal. Participants were all outpatients and referred for the data collection by clinicians. They were invited to complete self-report questionnaires by a research assistant before or after the psychiatric consultation. Information about the research aims and data confidentiality was assured. Participants provided written informed consent before participating. Based on the data obtained through the SIQ-TR, the sample was divided into participants who reported absence of NSSI over their lifetime and participants with current or past NSSI. For the present study, only participants who reported current or past NSSI were considered, that is, a total of 73 participants.
Statistical analyses
The statistical analyses were conducted with IBM SPSS Statistics 27.0 (SPSS, Inc., Chicago, IL). Descriptive statistics examined demographic and clinical characteristics of the sample, including ED diagnoses and NSSI. A cluster analysis was performed with the total scores of ED-15, DERS and UPPS-P negative urgency to identify different groups based on eating psychopathology, difficulties in emotion regulation and negative urgency. First, a hierarchical cluster analysis, using the between-groups linkage and the squared Euclidean distance, was performed to estimate the probable number of clusters. Second, a non-hierarchical procedure, the K-means cluster analysis, was performed to find the optimal cluster solution. In this analysis, the number of clusters determined by the hierarchical procedure was pre-specified. The Silhouettes coefficient was also used to measure the goodness of the final cluster solution. This coefficient allows to verify if the elements within a cluster are similar or cohesive to each other, while the clusters themselves are different or separated. The Silhouette values range from -1 to +1. In a good solution, the coefficient close to the value of 1.
One-way analyses of variance (ANOVA) were used to determine differences among the clusters regarding total scores of ED-15, DERS and UPPS-P negative urgency, as well as regarding age, BMI, durations of the ED or treatment, and number of methods of NSSI. One-way multivariate analyses of variance (MANOVA) were used to analyze differences among the clusters in eating attitudes and dimensions of emotion dysregulation. Kruskal-Wallis tests (χ 2) were also used to analyze differences among the clusters in eating behaviors (ED-15). Finally, Chi-Square tests (χ 2) were conducted to determine the distribution of current (in the preceding week or month of the study) and past (within the previous several months or more than a year ago) NSSI across clusters. The relevant assumptions of all statistical analyses were tested; p values<.05 were considered significant.
Results
Cluster analysis
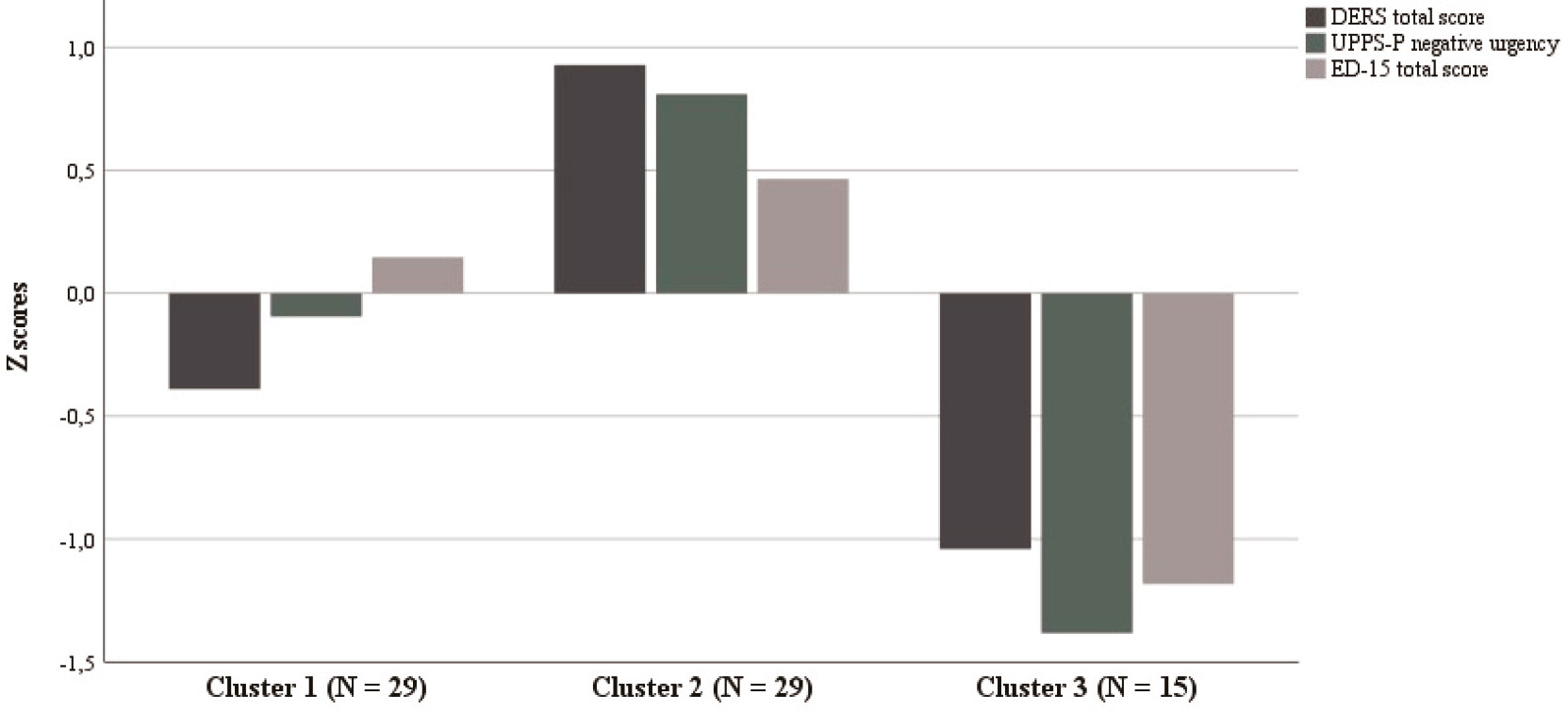
Based on the total scores of ED-15, DERS and UPPS-P negative urgency, three clusters were estimated by the hierarchical cluster analysis, which coincided with the optimal solution chosen by the K-means cluster analysis. The Silhouettes coefficient was used as a measure of the goodness of the final cluster solution and its mean value was .301 (min. -.086; max. .508), suggesting a fair fitting. Cluster 1 comprised 39.7% of the sample (n=29), Cluster 2 also included 39.7% of the sample (n=29) and Cluster 3 represented 20.5% of the participants (n=15). The standardized scores for the three clusters are presented in Figure 1. Cluster 1 represented the participants with high ED-15 total scores relative to the sample mean, as well as the participants with lower-than-average total scores of DERS and UPPS-P negative urgency. Cluster 2 was characterized by participants with the highest scores in the three variables relative to the sample means. Cluster 3 represented the participants with the lowest scores in the three variables relative to the sample means.
Comparison among the clusters
A series of one-way ANOVAs were conducted to test differences among the clusters in the main variables (Table 1). The results revealed significant differences among the three clusters in the total scores of ED-15, F(2,70)=22.18, p<.001, DERS, F(2,32)=63.22, p<.001, and UPPS-P negative urgency, F(2,32)=48.30, p<.001. In pairwise comparisons, the ED-15 total score in Cluster 1 was significantly higher than in Cluster 3 (mean difference=2.09, p<.001), and the ED-15 total score in Cluster 2 was also significantly higher than in Cluster 3 (mean difference=2.59, p <.001). No differences were found between the Clusters 1 and 2 in ED-15 total score (mean difference=-.50, p=.34). For DERS total score, Cluster 1 scored significantly lower than Cluster 2 (mean difference=-40.43, p<.001) and scored significantly higher than Cluster 3 (mean difference=19.91, p=.04). Cluster 2 scored significantly higher than Cluster 3 (mean difference=60.34, p<.001). For UPPS-P negative urgency, Cluster 1 also scored significantly lower than Cluster 2 (mean difference=-6.38, p<.001) and scored significantly higher than Cluster 3 (mean difference=9.07, p=.04). Cluster 2 scored significantly higher than Cluster 3 (mean difference=15.45, p<.001).
Additionally, the differences among the clusters in attitudes and eating behaviors, as well as in the dimensions of emotion dysregulation were analyzed (Table 1). Regarding eating attitudes, the MANOVA revealed a significant overall effect of the clusters on the subscales of the ED-15, F(4,138)=9.83, p<.001; Wilk’s λ=.61, partial η 2 =.22. Univariate ANOVAs indicated that both weight and shape concerns, F(2,70)=21.29, p<.001, and eating concerns, F(2,70)=14.41, p<.001, were significantly different among clusters. Post-hoc comparisons suggested that weight and shape concerns in Cluster 1 were significantly higher than those in Cluster 3 (mean difference=2.19, p<.001). Weight and shape concerns in Cluster 2 were also significantly higher than those in Cluster 3 (mean difference=2.73, p<.001). Additionally, eating concerns in Cluster 1 were significantly higher than those in Cluster 3 (mean difference=1.96, p<.001), as well as eating concerns in Cluster 2 were significantly higher than those in Cluster 3 (mean difference=2.41, p<.001). No differences were found between the Clusters 1 and 2 in weight and shape concerns (mean difference=-.54, p=.35) or eating concerns (mean difference=-.46, p=.54).
Table 1 Differences among the clusters in the main variables
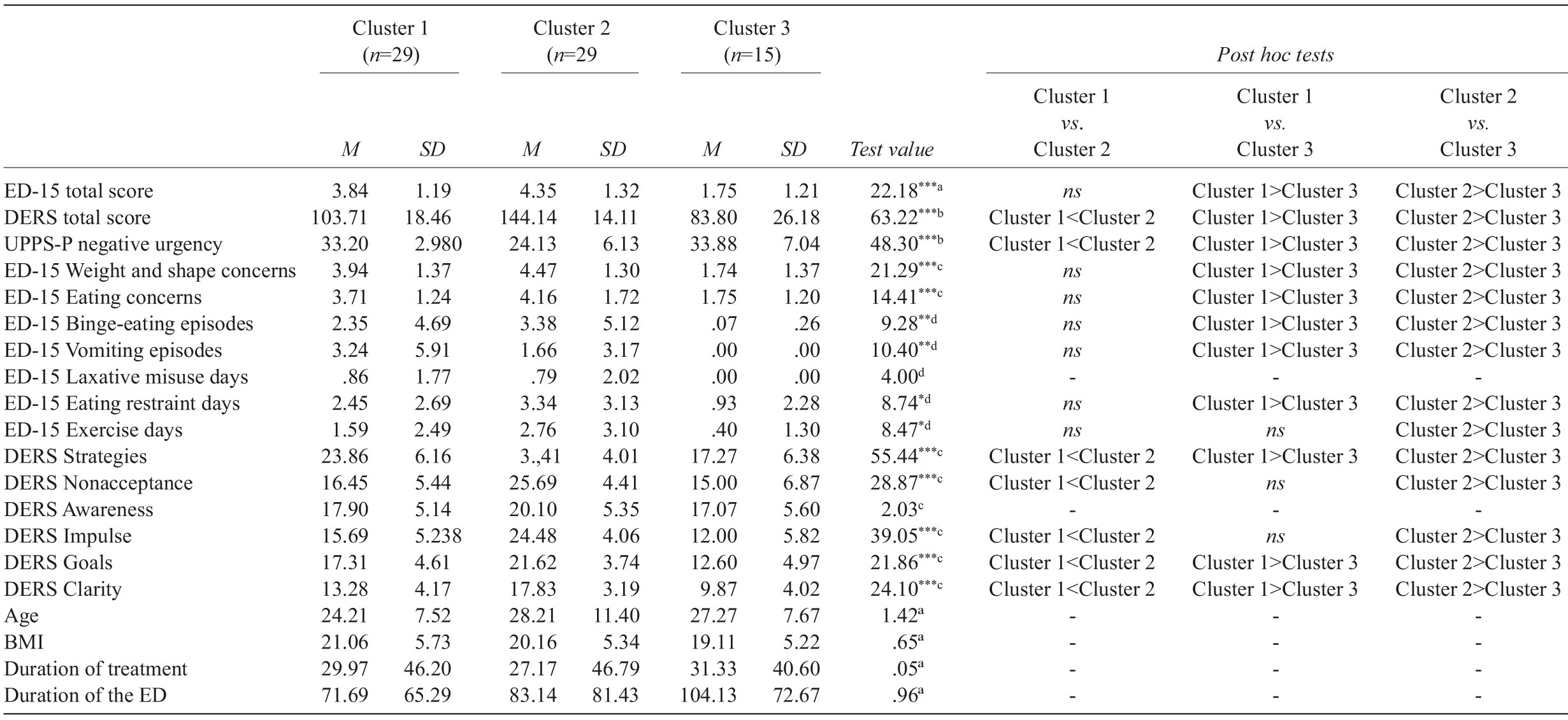
Note. DERS=Difficulties in Emotion Regulation Scale; ED-15=Eating Disorder-15. aANOVA (post hoc Gabriel); bANOVA (Welch’s F and post hoc Games-Howell); cMANOVA with pairwise univariate contrasts (post hoc Gabriel); dKruskal-Wallis test (Mann-Whitney tests with Bonferroni correction). *p<.05; **p<0.01; ***p<.001.
For eating behaviors, Kruskal-Wallis tests showed significant differences among the clusters in binge-eating episodes, χ 2 (2)=9.28, p=.010, vomiting episodes, χ 2 (2)=10.40, p=.006, eating restraint days, χ 2 (2)=8.74, p=.013, and excessive exercise days, χ 2 (2)=8.47, p=.015. No significant differences were found among the clusters on laxative misuse days, χ 2 (2)=4.00, p=.135. Mann-Whitney tests with Bonferroni correction suggested that participants from Cluster 1 scored significantly higher than those from Cluster 3 in binge-eating episodes, U=144.50, p=.021, vomiting episodes, U=120.00, p=.003, and restraint days, U=135.50, p=.026. For excessive exercise days, no differences were found between the Clusters 1 and 3, U=160.00, p=.077. Participants from Cluster 2 scored significantly higher than those from Cluster 3 in binge-eating episodes, U=112.00, p=.002, vomiting episodes, U=112.50, p=.002, eating restraint days, U=108.00, p=.004, and excessive exercise days, U=117.00, p=.005. No differences were found between the Clusters 1 and 2 in all eating behaviors.
With respect to the dimensions of emotion dysregulation, the MANOVA revealed a significant overall effect of the clusters on the six subscales of the DERS, F(12,130)=10.65, p<.001; Wilk’s λ=.25, partial η 2 =.50. Except for awareness, F(2,70)=2.03, p=.139, univariate ANOVAs indicated that strategies, F(2,70)=55.44, p<.001, nonacceptance, F(2,70)=28.87, p<.001, impulse, F(2,70)=39.05, p<.001, goals, F(2,70)=21.86, p<.001, and clarity, F(2,70)=24.10, p<.001, were significantly different among clusters. Post-hoc comparisons suggested that participants assigned to Cluster 1 scored significantly lower than those assigned to Cluster 2 in strategies (mean difference=-10.55, p<.001), nonacceptance (mean difference=-9.24, p<.001), impulse (mean difference=-8.79, p<.001), goals (mean difference=-4.31, p<.001) and clarity (mean difference=-4.55, p<.001). On the other hand, the Cluster 1 scored significantly higher than the Cluster 3 in strategies (mean difference=6.60, p<.001), goals (mean difference=4.71, p=.003) and lack of emotional clarity (mean difference=3.41, p=.016). Finally, the Cluster 2 scored significantly higher than the Cluster 3 in strategies (mean difference=17.15, p<.001), nonacceptance (mean difference=10.69, p<.001), impulse (mean difference=12.48, p<.001), goals (mean difference=9.02, p<.001) and clarity (mean difference=9.02, p<.001).
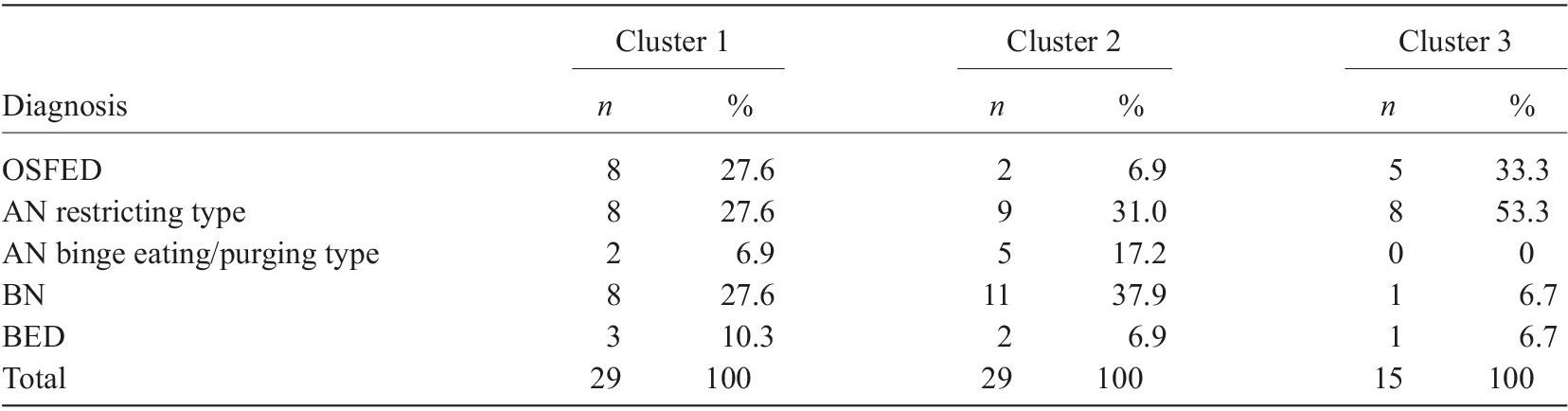
No significant differences were found among the clusters regarding age, BMI and durations of the ED or treatment (Table 1). Regarding the distribution of the DSM-5 ED diagnostics into each cluster (Table 2), Cluster 1 included equal proportions of patients with AN restricting type, BN and OSFED. Most patients in Cluster 2 were diagnosed with BN, followed by patients with AN restricting type. Cluster 3 did not include participants with AN binge eating/purging-type and most of the patients in this cluster were diagnosed with AN restricting type.
Characteristics of NSSI in each cluster
Chi-square tests were conducted to determine the distribution of current (in the preceding week or month of the study) and past (within the previous several months or more than a year ago) NSSI across clusters. A significant relationship was found between cluster membership and engagement in current or past NSSI, χ 2 (2)=14.37, p=.001. While in Cluster 2, most participants (n=17, 58.6%) reported NSSI during the preceding week or month of the study, in Clusters 1 (n=18, 62.1%) and 3 (n=15, 100%), more participants reported NSSI within the previous several months or more than a year ago.
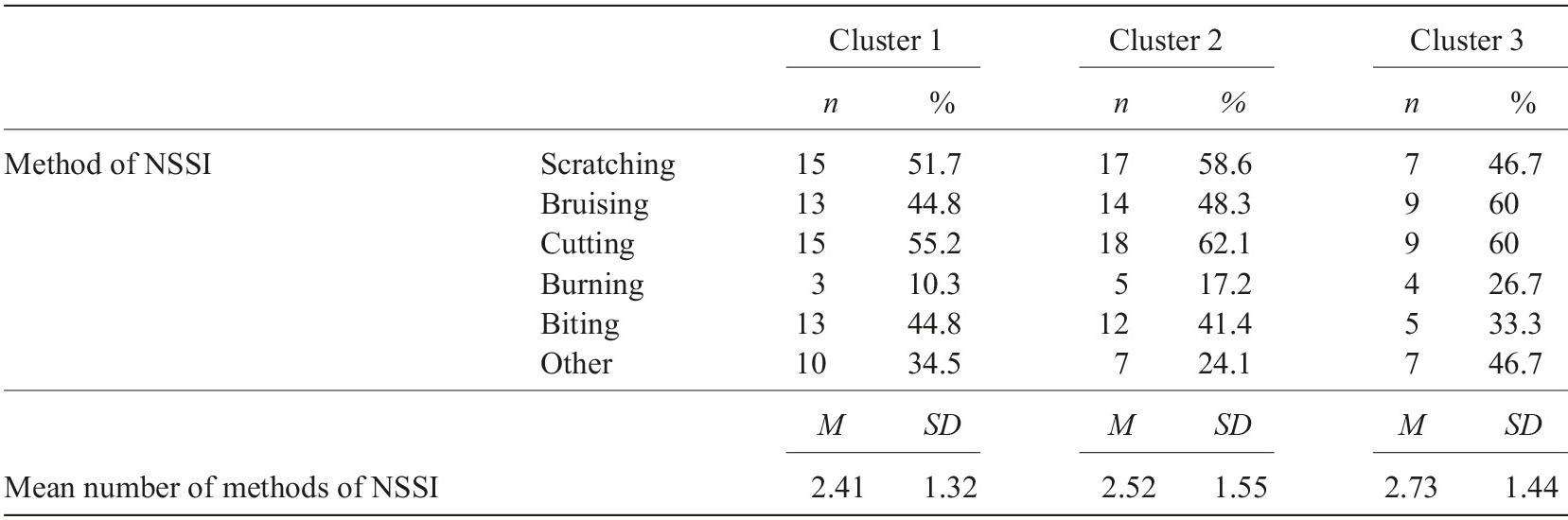
There were no significant differences among the clusters in number of methods of NSSI, F(2,70)=.24, p=.79. As outlined in Table 3, the most common method of NSSI in the three clusters was cutting.
To sum up, Cluster 1, compared to the sample mean, included participants with higher levels of eating pathology. It was also characterized by lower emotion dysregulation and negative urgency than Cluster 2, but both higher than Cluster 3. The most frequent diagnoses in this cluster were AN restricting type, BN and OSFED. Finally, Cluster 1 included more participants with past NSSI. Cluster 1 was labeled in this study as the “moderate severity cluster”.
Cluster 2 included the participants with the highest scores in the main variables, namely greater levels of eating pathology, emotion dysregulation and negative urgency than the other clusters. The most frequent diagnoses in this cluster were BN and AN restricting type. Cluster 2 also included more participants with current NSSI. It was labeled as the “high severity cluster”.
Cluster 3 included the participants with the lowest levels of eating pathology, emotion dysregulation and negative urgency. The most frequent diagnosis was AN restricting type, and this cluster included more participants with past NSSI. Cluster 3 was labeled in this study as the “low severity cluster”.
Discussion
The aim of the present study was to explore empirical severity clusters with outpatients with ED and lifetime NSSI regarding ED symptomatology, emotion dysregulation and negative urgency. A three-cluster structure has emerged based on the factors considered. These clusters ranged from a less dysfunctional cluster (low severity) to moderate and highly severity clusters of patients.
The first cluster, the “moderate severity” cluster, included participants with high levels of eating pathology but moderate levels of emotion dysregulation and negative urgency. This cluster included more participants with past NSSI (more than one year) These moderate difficulties, concerning potential mechanisms underlying ED and NSSI found in this cluster, may be explained by higher ED symptomatology precisely when NSSI is not a current symptom. In fact, no differences were found between the clusters 1 (“moderate severity” cluster) and 2 (“high severity” cluster) on ED-15 total score and on all eating disordered behaviors evaluated (e.g., binge-eating). The second cluster, the “high severity” cluster, was characterized by high difficulties in emotion regulation, high ED symptomatology as well as by high negative urgency. Within this cluster there was the highest prevalence of patients with current NSSI. Although all the patients in this study reported some kind of NSSI across the lifespan, we found that present NSSI is related with highest severity in ED symptomatology, what is in accordance with prior literature (Claes & Muehlenkamp, 2014; Islam et al., 2015). Additionally, within this “high severity” cluster there was the highest prevalence of patients with BN. This is also consistent with previous studies that showed that NSSI can be a part of a spectrum of multi-impulsive behaviors that include binging and purging behaviors, and both NSSI and eating disordered behaviors may represent attempts to deal and regulate negative emotions (Gómez-Expósito et al., 2016; Muehlenkamp et al., 2012; Wolff et al., 2019). In sum, the “high severity cluster” might be driven by the comorbid ED symptomatology. Furthermore, the pathology of this cluster may be related to personality features, as those with both ED and NSSI seem more likely to have certain comorbidities, such as borderline personality disorder (Jacobson & Luik, 2014). It also appears that borderline personality disorder and ED (particularly, binge-eating/purging-type ED) share common risk factors, including childhood trauma (Sansone & Sansone, 2007), impulsivity and urges of self-harm (Sansone & Sansone, 2011), and emotion dysregulation (Selby et al., 2009). Then, more studies are needed to examine personality features as playing a role in the etiology and risk for EDs and NSSI. When considering treatment for patients who are in this cluster, it is also important to target not only eating symptomatology but also factors that may be responsible for the current maintenance of NSSI.
Addressing emotion regulation and impulsivity could be an important focus of treatment in this “high severity” cluster.
The third cluster, the “low severity” cluster, was the one with the lowest scores on ED symptomatology, emotion dysregulation and negative urgency. This cluster also included more participants with past NSSI and the highest percentage of patients with AN restricting type. These results are in line with previous research (e.g., Cucchi et al., 2016) that showed that NSSI is more prevalent among patients with BN and with AN binge eating/purging type compared to patients with AN restrictive type.
In sum, the results of the current study describe a three-cluster structure that range from a less severity and less dysfunctional cluster to a higher severity and dysfunctional cluster. Our intent was to contribute to a better understanding of NSSI in the context of ED and to a better individualization of treatment by identifying possible mechanisms underlying both conditions and levels of severity, such as emotion dysregulation and negative urgency.
This study has several limitations. First, the small number of participants and consequently the small dimension of participants in each cluster. Second, the sample included most women and only outpatients with both ED and NSSI. So, the results cannot be generalized to men, to inpatients or to individuals without NSSI. Future research using cluster analysis may also include ED patients without NSSI and patients with other types of treatment (e.g., inpatient treatment) to compare clinical presentations and to understand the impact of treatment on differences among the clusters. Third, the fair fitting of the cluster solution and the cross-sectional nature of the study, which allows us only to draw correlational conclusions from the current results; for future studies, with larger samples, it will be important to replicate current analyses and to explore longitudinally how the behaviors and mechanisms evaluated interact during time. Finally, the use of self-report measures to evaluate behaviors such as NSSI and ED symptoms, as these measures are open to several biases (e.g., social desirability); for future studies, it will be important to use semi-structured interviews to better explore and understand both conditions. Despite the limitations, as far as we know, this study is the first to investigate different clusters among Portuguese outpatients with ED who have also engaged in NSSI. Thus, this study provides important information about the distinct features of subgroups with ED and lifetime history of NSSI, and the results suggest that emotion regulation and impulse control should also be assessed and incorporated in the interventions, especially among individuals with a more severe ED and current NSSI.