Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista Portuguesa de Saúde Pública
versão impressa ISSN 0870-9025
Rev. Port. Sau. Pub. vol.31 no.1 Lisboa jan. 2013
https://doi.org/10.1016/j.rpsp.2013.01.002
ARTIGOS ORIGINAIS
Efficiency and equity consequences of decentralization in health: an economic perspective
Consequências em eficiência e equidade da descentralização na saúde: uma perspetiva económica
Joana Alvesa*, Susana Peraltab, Julian Perelmana
aEscola Nacional de Saúde Pública, Universidade Nova de Lisboa, Lisboa, Portugal
bNova School of Business and Economics, Universidade Nova de Lisboa, Lisboa, Portugal
ABSTRACT
Over the recent years, decentralization has been adopted in many health systems. The question however remains of whether local actors do better than the central government. We summarize the main insights from economic theory on the impact of decentralization and its empirical validation. Theory suggests that the decision to decentralize results from a trade–off between its advantages (like its capacity to cater to local tastes) and costs (like inter–regional spillovers). Empirical contributions point that decentralization results in better health outcomes and higher expenditures, resulting in ambiguous consequences on efficiency; equity consequences are controversial and address the relevance of redistribution mechanisms.
Keywords: Decentralization. Efficiency. Equity. Health economics. Incentives.
RESUMO
Apesar de muitos sistemas de saúde terem optado recentemente pela descentralização, fica por esclarecer se os governos locais têm um melhor desempenho do que os centrais. Este artigo sumariza os principais resultados da teoria económica sobre o impacto da descentralização e a sua validade empírica. A decisão de descentralizar resulta duma arbitragem entre as vantagens, como a adaptação às preferências, e os inconvenientes, como as externalidades inter–regionais. Os estudos empíricos sugerem que a descentralização permite ganhos em saúde mas também despesas maiores, com consequências ambíguas em termos de eficiência, e que as consequências para a equidade, sendo controversas, indicam a relevância dos mecanismos de redistribuição.
Palavras-chave: Descentralização. Eficiência. Equidade. Economia da saúde. Incentivos.
Introduction
Over the recent years, decentralization has been one of the main reforms adopted in many health systems. Strong decision power of sub-central governments already existed in Scandinavian counties and in federal states like Canada, Switzerland and Australia1; the most recent devolution processes have been observed in NHS systems, namely in Spain and Italy (toward regions), and the UK (toward Wales, Scotland, Northern Ireland). In a few words, more delegation to local authorities was expected to improve services through a combination of better knowledge of local needs, preferences and providers characteristics, higher accountability of policy-makers and efficiency-enhancing competition among jurisdictions.
These expected benefits are however far from obvious and the major question for policy-makers and researchers remains, that is, whether local actors really do better than the central government. Put differently, the issue is whether decentralization allows for the provision of better and equitable health services to all citizens at an acceptable cost. Oates2 was the first one to suggest that the decision to decentralize results from a trade-off between its advantages and costs. Whether the benefits actually outweigh the costs – the efficiency issue – is ultimately an empirical question. The literature has mainly focused on overall efficiency by estimating the impact of decentralization on economic growth.3, 4 Another alternative is to measure the impact of decentralization on sectoral policies.5 Decentralization of health policies is relatively recent; the literature is still scarce and often provides contradictory results. We summarize the main insights from economic theory on the impact of decentralization of health policies, and we review empirical studies that have tested some of these theoretical assumptions.
Institutional context
Decentralization in health care can adopt many different forms. Following the typology proposed by Vrangbaek,6 our main interest here is in devolution or political decentralization, through which power is decentralized to lower-level political authorities such as regions or municipalities. Other forms of decentralization are also possible which are beyond the scope of the present paper. De-concentration and bureaucratization involve transfers between administrative levels and from political to administrative level, respectively (think for example in the Portuguese context, of transfer of competences to Regional Health Authorities). Decentralization also refers to delegation, which involves transferring power to more or less autonomous public organization management (like public enterprises, for example the hospitals S.A in Portugal, Foundation Trusts in the UK or public insurance companies in Bismarckian-type health systems). Privatization itself can be considered as a form of decentralization.
Our focus here is thus on the transfer of political authority in the health area from higher to lower levels of government or from national to sub-national levels.7 Regional, provincial or municipal elected governments may thus be responsible for planning, organizing, delivering and financing health services. Multiple arrangements are however possible and devolution has taken many different forms across OECD countries (for a complete mapping of decentralization experiences in Europe, see Bankauskaite et al.8). The size of decentralized entities is highly variable, from small counties in Sweden (average population 31,000) to large autonomous regions in Spain (average population 2,444,000). The extent of competences also varies. The central state may keep responsibilities in several domains, for instance the Canadian Federal state defines policies regarding health prevention and promotion, the Swiss Confederation defines the basic health benefit package, and generally all central states impose a series of more or less stringent regulations on quality, supply, coverage, pricing rules or budget allocation. A key issue which differentiates decentralization experiences relates to the funding of health expenditures and financial autonomy. Decentralized governments may have the power to raise taxes, or receive transfers depending on their contribution to fiscal revenues. They may then be free to set the budget allocated to health and its distribution among health sectors. By contrast, sub-central government levels may be financed by transfers based on risk-equalization schemes and benefit from low autonomy in defining tax rates. In the latter case, decentralized governments may thus have the political power to decide about allocation of resources but do not control the amount of available resources for health. Hence the expenditure side is decentralized, but revenue is not.
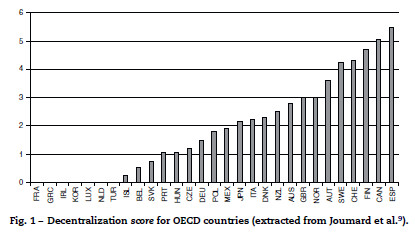
Fig. 1, extracted from Joumard et al.9, nicely describes the degree of decentralization in health in OECD countries (where a 0 score implies that central government takes most of key decisions while a 6 score implies residual competences for the central government). Countries have heterogeneous sub-central governments, with different size, autonomy and responsibilities allocated. The criteria to define this score have been established by Paris et al.10, using a survey. They include in particular the sub-central governments authority on setting tax bases and rates, the budget allocation for health and its distribution between health sectors, the financing of different health services and practitioners and the setting of public health objectives. Spain, Canada, Finland, Sweden and Switzerland have higher autonomy of sub-central governments while Portugal is among the countries with the lowest health decentralization.
Note that the decentralization question, the way we pose it (devolution or political decentralization), is more common in NHS-type health systems. These systems have been usually characterized by highly centralized decision-making, with one single insurer/payer and provider (the central state), and little autonomy given to providers. By contrast, health systems based on social insurance schemes have been usually characterized, to various extents, by multiple insurance schemes and some degree of publicly subsidized private provision. Hence, transferring power to local institutions has certainly responded to a demand for more autonomy in more rigid NHS-type health systems.
Spain, Canada and Italy are particularly relevant cases to understand the empirical literature because the consequences of decentralization in health have been more extensively analyzed. The most decentralized country according to Joumard et al.9 is Spain. The central government provides the general framework and coordinates the health system while Autonomous Communities (AC) provide health care services and are responsible for health planning, organization and management.11 Funds are centrally collected and allocated to regions by means of a block central grant following an unadjusted capitation formula.11 Only Navarra and the Basque Country benefit from fiscal authority.
By contrast, the Canadian Confederation, composed of 10 provinces and 3 territories, has been decentralized since the 19th century.12 Health funding, administration and delivering are competences of provinces, which also define physician financing rules and hospital global budgets. However health promotion, prevention and provision to specific groups are Federal competencies. Provinces are responsible for funding health care expenditures, based on provincial taxes and transfers from the central government. Transfers depend themselves on taxes collected at provincial level; an equalization program was however implemented to avoid strong differences in transfers related to discrepancies in provinces revenue-generating potential.13
Finally, the 20 Italian regions also control health care provision, although general objectives (like the detailed list of services to be provided) and main principles of the health system are defined at the central level. Regions can develop regional health plans, allocate resources and collect revenues freely, like setting user charges for drugs prescriptions or reimburse rates for drugs and services not covered at national level. Regional authorities also enjoy financial autonomy in taxation; in practice, regional health expenditures are financed at 36.7% by regional taxes.14 Additionally, regional health expenditures are financed by transfers from the central state (57.3% of expenditures), essentially from a so-called National equalizing fund. This fund is based on the idea that all regions must achieve a minimum level of expenditures, so that transfers top up regions own revenue in case it is unable to fund this minimum level.
Theoretical background
The debate on the relative merits of policy decentralization dates back to Tiebout,15 who put forward a very optimistic argument for the optimality of local public good provision, based on an analogy between competitive markets and competing jurisdictions. Oates,2 in contrast, suggests that decentralization results from a trade-off between its advantages and costs. According to Oates, the advantage of decentralization lies in its capacity to cater to local tastes, be it because of better information or simply because the central government cannot differentiate public good provision. The cost of decentralization stems essentially from the presence of inter-regional spillovers. For instance, better health prevention in one municipality benefits its neighbors. However, if health prevention is decentralized, each municipality fails to take into account the benefit of its investment in other municipalities, and is therefore likely to invest sub-optimally, leading to under-provision and/or low quality of health services. While Oates argument that a central government is unable to differentiate the provision of local public goods according to local preferences has been challenged since, his main intuition that the decision to decentralize rests on a fundamental trade-off between costs and advantages remains. One of the main costs of decentralization which has been analyzed in the literature is the failure to exploit economies of scale.16 For instance, collective purchasing of resources (drugs, medical devices, equipments, etc.) or collective administration of health services may display decreasing average costs and be thus more efficiently provided at a centralized level.
The inter-regional spillovers at the heart of Oates's argument, referred here-above, are of the horizontal type (that is, between sub-central governments of the same level). Another sort of spillovers which may create inefficiencies under decentralization is the vertical ones between local and central governments. These occur if one government level's policy decisions have an impact in the policy outcomes of the other level. These phenomena are highly plausible in the health care sector. If, for example, sub-central governments are responsible for some public health prevention programs and the central state delivers health care, local policies likely affect services use and costs at the central level. Unless sub-central governments are rewarded for their actions, they have little incentives to provide an optimal value of prevention, whose benefits are fully enjoyed by the central state.
Recently, the literature has put forward political economy arguments in favor of decentralization. For instance, it may be that the voters, who are imperfectly informed about the economy, use the policies put in place by the neighboring politicians to impose discipline on their own local representative. In such a world of opportunistic policy makers, decentralization may be a strong mechanism to prevent corruption or promote provision of public services.17 Another argument is that decentralization forces local jurisdictions to compete for mobile resources (for instance, labor or capital) and puts a downward pressure on taxation, thus prompting a more efficient use of scarce resources (see Wilson18 for a survey of the tax competition literature). Besley and Smart19 show that this need not be the case, since higher discipline of local politicians comes at the cost of a worse selection. Indeed, it is only when an opportunistic politician misbehaves that the voters are given the chance to oust her from power and replace her with a potentially benevolent politician. Political accountability results from a trade-off between these two mechanisms (discipline and selection), and further decentralization has opposite effects in both.
What can be said about the likelihood of local governments being captured by special interests? Bardhan and Mookherjee20 show that there is no theoretical reason to suppose that local governments are more prone to this than central ones. They put forward a theoretical model of probabilistic voting where capture by special interests results from a combination of voter awareness, interest group cohesiveness, electoral uncertainty and competition, district heterogeneity and the electoral system. Their main conclusion is that the extent of capture at the local level is most likely context-specific and needs to be assessed empirically.
A few authors have looked at the applicability of these arguments to the specific case of health decentralization. Levaggi and Smith21 claim that sub-central governments are better informed about the constraints of local supply and about variations in demand. Variations in demand are obviously related first to differences in local needs, for instance regions experience discrepancies in the prevalence of diseases, in behavioral and non-behavioral risk factors (including in particular ageing or social determinants), perhaps also in the effectiveness of specific interventions. Hence priorities are likely to differ according to burden of disease or cost-effectiveness criteria. Also local preferences shape variations in demand, leading to different priorities and resource allocation criteria. We may think that some regions have a higher concern for inequalities in health and social determinants, while others put a greater emphasis on provider choice and responsiveness to patients preferences. These differences in needs and preferences are very clear if we compare European countries. Discrepancies in local supply are related to the availability and density of physicians, nurses, equipments, but also to differences in local prices and practices. Central governments have tried to account for these differences in financing sub-central governments, through more or less sophisticated risk-adjustment schemes, but may not be able to address these issues to locally adjusted planning or organization. Sub-central governments may be better equipped to respond to local preferences and priorities, to coordinate providers actions and to identify the sources of inefficiency. Hence, decentralization is expected to enhance quality and responsiveness of care while reducing costs; this theoretical view is at the origin of most decentralization processes.
As regards the potential incentives that favor efficiency and/or quality in health care provision, both the tax competition and the yardstick competition mechanisms are likely to arise in health policies, thus leading sub-central governments to compete with each other to provide high-quality services at low user charges or financed through lower taxes. First, better and more efficient services contribute to attract mobile citizens, hence increase sub-central governments economic activity and fiscal revenues. Second, competition occurs through citizens benchmarking their demands on the basis of neighbor sub-central governments performance.22 If sub-central governments are politically accountable, a local politician providing poorer services than his neighbors counterparts would likely fail re-election. In a few words, efficient provision contributes to attractiveness and citizens satisfaction.
It is a well-known fact that decentralization may hamper redistribution (see, Cremer et al.23 for a survey of the literature), when taxes are locally collected. Areas with high health needs are in general the poorer ones (there is large evidence of the relationship between poverty and poor health status, see Marmot Review24); under fiscal decentralization, underprivileged areas capture lower resources from taxation and benefit from a lower capacity to invest in high-quality services and efficient provision. Decentralization then produces differences in the quality and availability of services, charges and outcomes. Increasing inequity is one of the major threats of decentralization, even if good risk-sharing agreements potentially mitigate this effect. In other words, the viability of decentralization depends on the existence of solidarity mechanisms between decentralized authorities.
The reverse is also possible, i.e., sub-central governments only competing on high-quality services, leading to over-provision of services and high health expenditures (race to the top). This situation is more likely to occur when fiscal decentralization is low and sub-central governments face soft budget constraints. This may the case, for example, if the central government systematically bails out sub-central governments which are excessively indebted or if transfers to sub-central governments are based on past expenditures.
This brings us to the fundamental question of the funding of local public goods. Indeed, various arrangements are possible regarding the degree of decentralization of both the expenditure and the revenue functions.25 A considerable share of local government funding comes from central government transfers. These transfer schemes must be carefully designed and rest on clear rules (depend on variables which are not easy for local governments to manipulate) so as to avoid moral hazard leading to excess expenditures. Indeed, as the central government is unable to distinguish the sources of high spending between higher needs and inefficiencies, sub-central governments have an incentive to hide their true needs to obtain higher financing from the central authority.
To sum up, the theoretical literature does not provide a definitive answer about the impact of decentralization on health policies. The high concern in many countries for equity in health is a major argument against decentralization, unless strong solidarity mechanisms are put in place. The contradictory expectations about efficiency require careful empirical validation. In these times of adverse economic circumstances, efficiency is more than ever a major issue in decision-making, and strong evidence is necessary before advocating for decentralization in health.
Empirical evidence
In order to get an exhaustive overview on empirical evidence, we performed a systematic literature review. We conducted a computerized literature search in PubMed (National Center for Biotechnology Information, Bethesda, Maryland) and Google Scholar, supplemented by a search of quoted references. Text keywords used in the search included decentralization, federalism, health, health care, equity, and efficiency. We restricted our analysis to those performed in OECD countries to allow for relevant comparisons, that is, in a comparable context. We only included empirical studies about the impact of decentralization, hence excluding theoretical studies, studies about legislation or about political or organizational aspects of decentralization, editorials and literature reviews. The search was limited to English-language articles published from 1995 to July 2012, when decentralization in health has become a relevant and applied policy option in OECD countries. Our search allowed collecting 17 papers, whose main characteristics and results are displayed in Table 1. Studies were divided according to distinct analyzes, based on the most relevant decentralization outcomes, namely inequalities in health and health care, health expenditures and health outcomes.
Inequality in health and health care use
The consequences of decentralization on inequality were the main issue analyzed by Zhong13, Jiménez-Rubio et al.1, Costa-i-Font26 and Frederiksson and Winblad27. Zhong13 found that in Canada inequalities in health care use (overall, within provinces and between provinces) decreased after decentralization. Most inequality was explained by within-provinces variation, while between-provinces variations did not much contribute to inequality.13 By contrast, Jiménez-Rubio et al.1 also using data from Canadian provinces observed that income-related inequalities in health care use resulted from between-provinces variations while income-related inequalities in health were related to within-region variations. While Zhong13 used an overall inequity measure, Jiménez-Rubio et al.1 used an income-related one, which possibly explains the discrepant results. The results by Jiménez-Rubio et al.1 certainly question the equalization scheme across provinces; the redistribution of funds from richer to poorer provinces does not seem to avoid inequity in health care use related to between-province variations (for example, health care use is lower in Quebec that has a lower-than-average income per capita). As the author emphasizes, advocates of decentralization would however consider these differences as related to different preferences, hence legitimate. Income-related inequity in health was mostly related to differences between rich and poor people within provinces, here questioning the efforts by provinces to reduce inequalities (would a central government be more committed to reduce inequity in health?).
For Spain, Costa-i-Font26 found a small overall, within and between regions income-related inequality in health, although somewhat higher in regions with lower autonomy. The author explains this difference by the greater role of the private sector in those regions. He also emphasizes that decentralization may have favored equity due to a high commitment of regions to achieve this objective, which corresponds to a high citizens concern. Finally, Fredriksson and Winblad27 studied a specific reform toward more provider choice in Sweden, where health care use is highly decentralized at the county level. The author showed that while some counties supported the reform through favoring choice, others implemented administrative barriers against it. Therefore, autonomy on decision making (regarding provider choice) resulted on inequalities between people living in different Swedish counties.
Health expenditures
Inequality related to decentralization was also observed indirectly, through examining the impact of regional GDP per capita on health care expenditures. Indeed, a greater impact of regional income on health care expenditure would mean that richer regions spend significantly more on health than poor ones, hence creating inequalities in health care use. Although all studies using regional data conclude that health care expenditures do not vary much with income (the elasticity with respect to income is below one), results are contrasted and vary between countries. For Spain, Prieto and Lago-Peñas28 found a positive relation between income and public health expenditures only in regions with higher fiscal autonomy. Regions without fiscal autonomy benefitted from national equalization efforts and therefore managed to achieve high levels of health care expenditures despite of lower income. The low impact of income on health care expenditures in Spain was confirmed by Cantarero, Costa-i-Font and Moscone.29, 11 The same conclusion could be drawn for Canada,21 although the impact of income on health expenditures was greater than in Spain. Using a specific indicator, Di Matteo and Di Matteo30 showed the positive impact of federal transfers on health care expenditure. That is, federal transfers certainly reduce the impact of regional income on expenditures but do not fully correct regional income discrepancies. The picture is somewhat different in Italy, where regional income had a strong impact on health care expenditures.31 The authors showed also that cost-containment measures have not altered cross-regional differences in health care expenditures and have even worsened them in some cases. For Switzerland, Crivelli et al.32 observed a large impact of physician supply, which is highly variable across regions, on health care expenditures. Hence cross-regional differences in health care supply may also be a source of inequality across regions. Finally, using data from 110 regions of 8 OECD countries, Lopez-Casasnovas and Saez33 showed a low elasticity of health care expenditure with respect to income. However, the impact of income was higher across regions in countries with higher inter-regional income inequalities, leading in turn to higher discrepancies in health care expenditures.
Scheffler and Smith34, Costa-i-Font and Moscone11, Costa-i-Font and Pons-Novell22 addressed the impact of decentralization on health expenditures, while Bordignon and Turati35 examined the impact of the interaction between central and sub-central governments. Scheffler and Smith34 showed for California that spending on uninsured patients decreased with the higher counties autonomy in allocating funds across health and social programs. Costa-Font and Pons-Novell22 observed that Spanish regions with both political and fiscal autonomy had higher health expenditures as compared to regions without autonomy or with political autonomy only. Costa-i-Font and Moscone11 observed however that decentralization increased expenditures only in the short run, producing savings in the long run. They argued that firstly decentralization increased health care costs due to sunk costs; then this effect was minimized in the long run by an experience curve, that is, learning-by-doing allowed reducing costs. Regarding assumptions from economic theory, Costa-i-Font and Moscone11 also showed the existence of spatial correlation of health care expenditures between neighbor jurisdictions, sustaining the assumption of horizontal spillovers. This result may hence be due to competition between neighbor jurisdictions to increase attractiveness or due to politicians being judged based on the neighbor counterparts actions.
Finally, Bordignon and Turati35 used 1990s Italian adjustment process imposed by an external entity (the European Union) to understand the role of expectations and the strategic interactions between the central state and regions, using data on health care expenditures. Regions expecting that the central government will intervene in case of debt softened their budget constraints and the relationship between the funding they receive from the central government and health expenditures was lower. By contrast, during external adjustment, the central government was perceived as more stringent and the link between funding and expenditures became stronger. And the central government was also more prone to cut funding to regions because it knew its commitment not to bailout would be taken more seriously. Interestingly, authors showed that more autonomy lead to more financially responsible policies because expectations of bailout were low. This paper thus emphasized that transfer mechanisms, which are always present in decentralized countries, created incentives that may be more or less detrimental for efficiency depending on how they are designed and put in practice.
Health results
Results about the impact of decentralization on health outcomes are scarce but consistent across studies. Jiménez-Rubio12, 36 and Cantarero and Pascual37 agree on identifying a positive relationship between fiscal decentralization and health results, measured through infant mortality. Cantarero and Pascual37 used an alternative measure of health status (life expectancy) which confirmed the positive contribution of decentralization to health status.
Conclusion
Although the economics literature has largely discussed the impact of decentralization, empirical results remain scarce, in particular regarding decentralization in health. Nevertheless, decentralization of health policies and funding has been largely implemented in various countries and is generally considered as a relevant option to improve efficiency in health care.7
Our review of the literature allows draw preliminary conclusions, based on relatively recent decentralization experiences, in particular in Canada, Italy, Spain and Switzerland. First and foremost, devolution of political (and fiscal) authority to sub-government levels seems to increase health care expenditures but also improve health outcomes, mainly measured through infant mortality rate. According to economic theory, decentralization may foster competition between jurisdictions to increase attractiveness, and increase pressure on local governments because citizens evaluate their performance based on neighbor counterparts actions. The empirical literature suggests that enhanced competition prompts local decision-makers to increase health care expenditures (race to the top) and not the reverse in order to decrease taxes (race to the bottom), with a favorable impact on health. The case of Spain is particularly enlightening, which shows that the increase in health care expenditures has been the highest in regions with fiscal autonomy. This result may reflect the high people's demand for high-quality health services, and the higher responsiveness of local authorities to this preference. The higher health care expenditures under decentralization may however reflect also higher costs, related for instance to duplication of inputs (two neighbor regions offering similar services which could be shared), diseconomies of scale, or the sunk costs associated to implementation of a local health provision scheme. To some extent, adverse incentives may play some role if sub-central governments are not fully financially responsible for their expenditures. In particular, moral hazard may exist if sub-central governments expect their debts being covered by the central state (bailout) or if their budget depends more largely from transfers from the central state. In a few words, decentralization does not appear at first sight as a means to control or reduce health care expenditures, but as an incentive to provide better and possibly more expensive services. The efficiency consequences are thus ambiguous, as it is unclear whether additional benefits – measured through a very reduced number of indicators – are worth additional costs.
Regarding equity, empirical results are ambiguous and certainly related to the specific countries context. Inequity in health and health care is low in Spain, where health expenditures are also poorly related to the region GDP/capita. Additionally, inequity in health care seems to be lower in more autonomous regions, so that decentralization may have favored equity. In Canada, income-related inequity in health care is related to between-provinces inequalities. In Italy and Switzerland, there is a strong relationship between regions (resp. cantons) income and health care expenditures, resulting in a large heterogeneity in health care expenditures. These results may certainly be related to lower equalizing mechanisms in these two countries coupled with a higher fiscal autonomy. Note also that different decisions across regions, namely about physicians or equipment supply, also potentially create differences/inequity in health care delivery.
To conclude, solidarity mechanisms across sub-central authorities are relevant to avoid the emergence of large inequalities across regions in health care delivery and expenditures. However, redistribution of funds also reduces jurisdictions financial responsibility, with possible detrimental consequences on expenditures and ambiguous consequences on efficiency. This last aspect is of particular importance if jurisdictions compete with each other for providing high-quality services and not through lowering tax rates.
Bibliografía
1. Jiménez–Rubio D, Smith P, Doorslae E. Equity in health and health care in a decentralised context: evidence from Canada. Health Econ. 2008; 17:377–92. [ Links ]
2. Oates W. Fiscal federalism. New York: Harcourt Brace Jovanovich; 1972. [ Links ]
3. Iimi A. Decentralization and economic growth revisited: an empirical note. J Urban Econ. 2005; 57:449–61. [ Links ]
4. Rodriguez–Pose A, Ezcurra R. Does decentralization matter for regional disparities?: a cross–country analysis. J Econ Geogr. 2010; 10:619–44. [ Links ]
5. Galiani S, Gertler P, Schargrodsky E. School decentralization: helping the good get better, but leaving the poor behind. J Public Econ. 2008; 92:2106–20. [ Links ]
6. Vrangbaek K. Towards a typology for decentralization in health care. En: Saltman R.B., Bankauskaite V., Vrangbaek K., editors. Decentralization in health care. Maidenhead: McGraw–Hill. Open University Press; 2007 (European Observatory on Health Systems and Policies Series). 44–62. [ Links ]
7. Bankauskaite V, Saltman RB. Central issues in the decentralization debate. En: Saltman R.B., Bankauskaite V., Vrangbaek K., editors. Decentralization in health care. Maidenhead: McGraw–Hill. Open University Press; 2007 (European Observatory on Health Systems and Policies Series). 9–21. [ Links ]
8. Joumard I, Bankauskaite V, Paris V, Dubois HFW, André C, Devaux M, Saltman RB, Nicq C, Wei L. Health systems institutional characteristics: a survey of 29 OECD countries. 23–43. [ Links ]
11. Costa–i–Font J, Moscone F. The impact of decentralization and inter–territorial interactions on Spanish health expenditure. Empir Econ. 2008; 34:167–84. [ Links ]
12. Jiménez–Rubio D. The impact of decentralization of health services on health outcomes: evidence from Canada. Appl Econ. 2011; 43:3907–17. [ Links ]
13. Zhong H. The impact of decentralization of health care administration on equity in health and health care in Canada. Int J Health Care Finance Econ. 2010; 10:219–37. [ Links ]
14. Ferrario C, Zanardi A. Fiscal decentralization in the Italian NHS: what happens to interregional redistribution?. Health Policy. 2011; 100:71–80. [ Links ]
15. Tiebout C. A pure theory of local expenditures. J Polit Econ. 1956; 64–416. [ Links ]
16. Haimanko O, Le Breton M, Weber S. Transfers in a polarized country: bridging the gap between efficiency and stability. J Public Econ. 2005; 89:1277–303. [ Links ]
17. Belleamme P, Hindriks J. Yardstick competition and political agency problems. Social Choice Welfare. 2005; 24:155–69. [ Links ]
18. Wilson JD. Theories of tax competition. Natl Tax J. 1999; 52:269. [ Links ]
19. Besley T, Smart M. Fiscal restraints and voter welfare. J Public Econ. 2007; 91:755–73. [ Links ]
20. Bardhan PK, Mookherjee D. Capture and governance at local and national levels. Am Econ Rev. 2000; 90:135–9. [ Links ]
21. Levaggi R, Smith PC. Decentralization in health care: lessons from public economics. En: Smith P., Ginnelly L., Sculpher M., editors. Health policy and economics: opportunities and challenges. London: Open University Press; 2004. [ Links ]
22. Costa–i–Font J, Pons–Novell J. Public health expenditure and spatial interactions in a decentralized national health system. Health Econ. 2007; 16:291–306. [ Links ]
23. Cremer H, Pestieau P. Factor mobility and redistribution. Handbook of regional and urban economics. Vol. 4. Amsterdam: Elsevier; 2004. 2529–60. [ Links ]
24. Institute of Health Equity. Marmot review: fair society, healthy lives: strategic review of health inequalities in England post 2010. London: Institute of Health Equity; 2010. [ Links ]
25. OECD. Taxing powers of state and local government. Paris: OECD Publications; 1999. [ Links ]
26. Costa–i–Font J. Inequalities in self–reported health within Spanish Regional Health Services: devolution re–examined?. Int J Health Plann Manage. 2005; 20:41–52. [ Links ]
27. Fredriksson M, Winblad U. Consequences of a decentralized healthcare governance model: measuring regional authority support for patient choice in Sweden. Soc Sci Med. 2008; 67:271–9. [ Links ]
28. Prieto DC, Lago–Peñas S. Decomposing the determinants of health care expenditure: the case of Spain. Eur J Health Econ. 2012; 13:19–27. [ Links ]
29. Cantarero D. Decentralization and health care expenditure: the Spanish case. Appl Econ Lett. 2005; 12:963–6. [ Links ]
30. Di Matteo L, Di Matteo R. Evidence on the determinants of Canadian provincial government health expenditures: 1965–1991. J Health Econ. 1998; 17:211–28. [ Links ]
31. Giannoni M, Hitiris T. The regional impact of health care expenditure: the case of Italy. Appl Econ. 2002; 34:1829–36. [ Links ]
32. Crivelli L, Filippini M, Mosca I. Federalism and regional health care expenditures: an empirical analysis for the Swiss cantons. Health Econ. 2006; 15:535–41. [ Links ]
33. López–Casasnovas G, Saez M. A multilevel analysis on the determinants of regional health care expenditure: a note. Eur J Health Econ. 2007; 8:59–65. [ Links ]
34. Scheffler R, Smith RB. The impact of government decentralization on county health spending for the uninsured in California. Int J Health Care Finance Econ. 2006; 6:237–58. [ Links ]
35. Bordignon M, Turati G. Bailing out expectations and public health expenditure. J Health Econ. 2009; 28:305–21. [ Links ]
36. Jiménez–Rubio D. The impact of fiscal decentralization on infant mortality rates: evidence from OECD countries. Soc Sci Med. 2011; 73:1401–7. [ Links ]
37. Cantarero D, Pascual M. Analysing the impact of fiscal decentralization on health outcomes: empirical evidence from Spain. Appl Econ Lett. 2008; 15:109–11. [ Links ]
Conflicts of interest
The authors declare that there are no conflicts of interests.
Funding
This investigation was funded by the Fundação para a Ciência e a Tecnologia through the project PTDC/EGE-ECO/104094/2008.
Received 17 September 2012. Accepted 21 January 2013
*Corresponding author: joana.alves@ensp.unl.pt













