Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Arquivos de Medicina
versão On-line ISSN 2183-2447
Arq Med vol.24 no.3 Porto jun. 2010
REVISÃO
Pulmonary Thromboembolism Revisited. The Radiologist's View.
Tromboembolismo Pulmonar Revisitado
Ana Sofia Preto*, Diogo Monteiro Rocha*, José Traila Campos*, Alexandre Lima Carneiro*, José Fonseca Gonçalves*
*Serviço de Radiologia, Hospital de São João
ABSTRACT
The authors have the following objectives: to review the mechanism and causes of Acute and Chronic Pulmonary Thromboembolism, to review clinical guidelines on when to ask for imagiological exams, to present the key imaging findings of this entity on 64-MDCT, to describe potential complications and identify possible pitfalls. MDCT angiography of the pulmonary arteries is very frequently performed to rule out Pulmonary Embolism at the emergency scene. If not recognized and treated it has an overall mortality of 30%. Sometimes, asymptomatic emboli organize, turning into a chronic picture. When there is pulmonary hypertension associated it results in cor pulmonale. After revision of some illustrative cases of Pulmonary Thromboembolism (PTE) from our institution, the authors realize that the classical conventional radiology signs are hard to see. The diagnostic criteria for acute PTE always include the presence of a filling defect on an arterial branch of pulmonary vasculature on MDCT. There are some variants presented on this essay. Chronic PTE may include signs of complete occlusion of a vessel that is smaller than adjacent patent vessels and a peripheral, crescent-shaped intraluminal defect that forms obtuse angles with the vessel wall, and contrast material flowing through thickened and often smaller arteries due to recanalization. The conclusions drawn from this paper might be summarized like this: MDCT is determinant for the diagnosis of this entity with its direct and indirect signs; differential diagnosis must be considered, as their treatment and prognosis might be very different; imagiological artifacts are among the worst pitfalls for the radiologist.
Key-words: pulmonary thromboembolism; diagnosis; prognosis
RESUMO
Os autores têm os seguintes objectivos: revêr os mecanismos e causas do Tromboembolismo Pulmonar agudo e crónico, rever guidelines clínicas sobre quando pedir exames imagiológicos, apresentar achados imagiológicos-chave desta entidade em Tomografia Computadorizada Multidetectores (64-TCMD), descrever complicações potenciais e identificar possíveis pitfalls. A angiografia por TCMD das artérias pulmonares é muitas vezes realizada para despiste de Tromboembolismo Pulmonar (TEP) no cenário de emergência. Se não reconhecido e tratado chega a ter uma mortalidade geral de cerca de 30%. Muitas vezes êmbolos assintomáticos organizam-se, constituindo um quadro crónico. Quando há hipertensão pulmonar associada, isso resulta em cor pulmonale. Após revisão de alguns casos ilustrativos de TEP da nossa instituição, os autores aperceberam-se que os sinais clássicos de radiologia convencional são muito difíceis de objectivar. Os critérios de diagnóstico de TEP agudo incluem sempre a presença de defeito de preenchimento num ramo arterial da vasculatura pulmonar em TCMD. Há algumas variantes apresentadas nesta revisão. O TEP crónico pode incluir sinais de obstrução completa dum vaso que é mais pequeno do que os vasos adjacentes e que estão patentes, um defeito intra-luminal periférico ou em forma de crescente que forma ângulos obtusos com a parede do vaso, e material de contraste fluindo através de artérias mais pequenas e espessadas devido a recanalização. As conclusões retiradas deste artigo pode são: a TCMD é determinante para o diagnóstico desta entidade com os seus sinais directos e indirectos; diagnósticos diferenciais devem ser considerados clinicamente, já que o seu tratamento e prognóstico podem ser muito diferentes e os artefactos em imagem estão entre os maiores inimigos do radiologista.
Palavras-chave: tromboembolismo pulmonar; diagnóstico; prognóstico
Introduction
Almost everyday clinicians need to rule out Pulmonary Embolism at the Emergency scenario. Pulmonary Embolism (PE) is the third most common acute cardiovascular pathology after myocardial infarction and stroke, resulting in thousands of deaths each year (1). If not recognized and treated it has an overall mortality of 30% (1). However, only 8% will dye if appropriate treatment is instituted. The challenge is that the disease is difficult to diagnose often because the symptoms are silent.
The term PE is a broad term that includes embolism from many sources such as air, bone marrow, talc, amniotic fluid, arthroplasty cement, tumor, and sepsis. The authors will focus specially on thrombolic venous PEs (Pulmonary thromboembolism - PTE) that develop from a distal source such as the deep veins of the legs. Usually, it is very difficult to know their proper origin just by image exams.
Revision of the mechanism and causes of acute and chronic pulmonary embolism
Pathophisiology
PTE is not a disease in and of itself. Rather, it is an often fatal complication of underlying venous thrombosis. Under normal conditions, microthrombi (tiny aggregates of red cells, platelets, and fibrin) are formed and lysed continually within the venous circulatory system. This dynamic equilibrium ensures local hemostasis in response to injury without permitting uncontrolled propagation of clot. Under pathological conditions, microthrombi may escape the normal fibrinolytic system to grow and propagate. PE occurs when these propagating clots break loose and embolize to block pulmonary blood vessels.
Thrombosis in the veins is triggered by venostasis, hypercoagulability, and vessel wall inflammation. These 3 underlying causes are known as the Virchow triad. All known clinical risk factors for Deep Vein Thrombosis (DVT) and PTE have their basis in one or more elements of the triad (1).
Patients who have known neoplasms, who have undergone gynecologic surgery, those with major trauma, and those with indwelling venous catheters may have DVTs that start at any location.
For other patients, venous thrombosis most often involves the lower extremities and nearly always starts in the calf veins, which are involved in virtually 100% of all cases of symptomatic spontaneous lower extremity DVT [1]. Current techniques allow us to demonstrate PE in 60-80% of these patients, even though about half have no clinical symptoms to suggest PE (1).
There is an easy way to memorize the most important risk factors – the 5 PM rule:
5 PM:
Past events of PE and /or DVT
Postoperative
Postpartum period
Pregnancy
Prolonged Immobilization
Malignancy
Acute PE
Clinical Manifestations -PTE has a wide spectrum of clinical manifestations ranging fromabsence of symptoms to patient death. Although most patients with PTE are asymptomatic, fewer than 20% present with the classical triad dyspnea, hemoptysis and pleuritic chest pain.
Chronic PE
Pathogenesis - The majority of pulmonary emboli resolve without sequelae. Ina small percentage of patients, particularly those with large emboli, the emboli undergo organization, recanalization, andretraction. The end result is vascular stenosis, which may leadto severe pulmonary hypertension and cor pulmonale.
Recognizing chronic pulmonary embolism is important because, without intervention, the survival rate is low, especially ifpulmonary hypertension is severe at the time of diagnosis. On the other hand, surgery usually results in good outcome in terms of both functional status (93% in New York Heart Associationclass I or II) and long-term survival rate (75% for patientswho had undergone surgery more than 6 years earlier) (1).
Clinical guidelines when to ask for imagiological exams
PTE has been described as the great masquerader because of the illusive, nonspecific and varied symptoms upon presentation.
Prompt diagnosis and stratification in patients with suspected PE and a high risk of adverse events may help to improve outcomes. For instance, highly sensitive D-dimer assays safely rule out pulmonary embolism in patients with a low or intermediate clinical probability, while less sensitive assays have been validated only in low probability patients in outcome studies. Clinical assessment has been shown to be useful for reducing the requirement for invasive tests in outcome studies and to be cost-effective. However is not enough.
Therefore, investigators developed prediction rules, the most widely validated of which are the Wells score and the Geneva score [1]. In our institution the cut-off value for image diagnosis is a Wells´ score of 2.
When evaluating patients with possible DVT, the initial task is to decide whether the clinical likelihood for DVT is Iow. When evaluating possible PE, the initial task is to decide whether the clinical likelihood is high. Patients with Iow likelihood of DVT or non-high (i.e. low to moderate) likelihood of PE can undergo initial diagnostic evaluation with D-dimer testing alone without obligatory imaging tests.
Diagnostic work-up
Nonimaging diagnostic modalities
Nonimaging tests are best utilized in combination with clinical likelihood of DVT or PE
BLOOD TESTS -The quantitative plasma D-dimer enzyme-linked immunosorbent assay (ELISA) rises in the presence of DVT or PE because of plasmins breakdown of fibrin. Elevation of D-dimer indicates endogenous although often clinically ineffective thrombolysis. The sensitivity of the D-dimer is greater than 80% for DVT (including isolated calf DVT) and greater than 95% for PE (1). The D-dimer is less sensitive for DVT than PE because the DVT thrombus size is smaller. The D-dimer is a useful "rule out" test. It is normal < 500 ng/rnL) in more than 95% of patients without PE. In patients with low clinical suspicion of DVT, it is normal in more than 90% without DVT. The D-dimer assay is not specific. Levels increase in patients with myocardial infarction, pneumonia, sepsis, cancer, the postoperative state, and second or third trimester of pregnancy. Therefore, it rarely has a useful role among hospitalized patients because their D-dimers are frequently elevated due to some systemic illness. Contrary to classic teaching, arterial blood gases lack diagnostic utility for PE, even though both the Po2 and PCO2 often decrease.
ELEVATED CARDIAC BIOMARKERS -Serum troponin levels increase in RV microinfarction. Myocardial stretch often results in elevation of brain natriuretic peptide or NT-pro-brain natriuretic peptide. Elevated cardiac biomarkers predict an increase in major complications and mortality from PE.
ELECTROCARDIOGRAM -The most cited abnormality, in addition to sinus tachycardia, is the S1 Q3 T3 sign: an S wave in lead I, Q wave in lead III, and inverted T wave in lead III. This finding is relatively specific but insensitive. Perhaps the most frequent abnormality is the ST-wave inversion in leads V1 to V4.
Noninvasive Imaging modalities
Chest X-Ray (CXR) - The initial chest x-ray (CXR) findings of a patient with PE are virtually always normal, although on rare occasions they may show the Westermark sign (i.e., a dilatation of the pulmonary vessels proximal to an embolism along with collapse of distal vessels, sometimes with a sharp cutoff) (2). Over time, an initially normal CXR often begins to show atelectasis, which may progress to cause a small pleural effusion and an elevated hemidiaphragm. After 24-72 hours, one third of patients with proven PE develop focal infiltrates that are indistinguishable from an infectious pneumonia. A rare late finding of pulmonary infarction is the Hampton hump, a triangular or rounded pleural-based infiltrate with the apex pointed toward the hilum, frequently located adjacent to the diaphragm. Another rare finding is an enlarged right descending pulmonary artery (2) (Pallas sign).
Multidetector Computerized Tomography (MDCT)
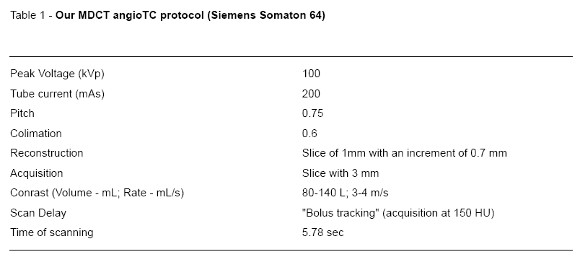
- The past few years have seen decisive dynamic developments in CT technology, mainly brought about by the advent of multi–detector row CT. The current generation of four–, eight–, and 16– and 64-detector row CT scanners now allow for coverage of the entire chest with 1-mm or submillimeter resolution within a short single breath-holdnow less than 6 seconds in the case of a 64–detector row CT, as it is in our institution. The protocol we use is according to the literature (Table 1).
The ability to cover substantial anatomic volumes with excelent spatial resolution has brought anumber of clear advantages. The high spatial resolution along the scan axis of a thin-collimation multi–detector row CT data set, allows an accurate evaluation of the full course of such vessels (2-5). The interobserver correlation for confident diagnosis of subsegmental emboli with thin-section multi–detector row CT by far exceeds the reproducibility of selective pulmonary angiography.
Key imagiological aspects on 64-MDCT
Direct MDCT signs of acute PE (3-5)
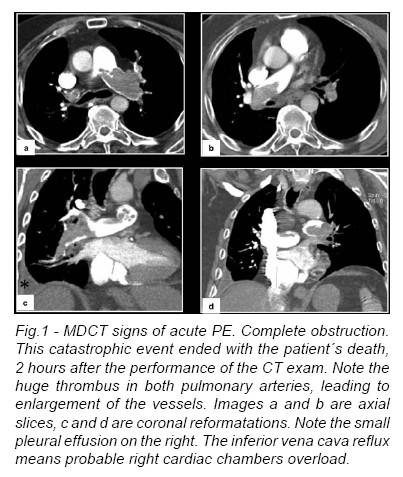
Complete Obstruction
On pulmonary angiograms,the diagnostic sign ofacute PE with complete obstruction is a concave filling defect or trailing edge that should be seen within the contrast material at thelevel of the obstruction.CTis able to show thrombus distal to the obstruction that cannot be seen on an angiogram. At the site of the thrombus, the diameter of the pulmonary artery may be increased because of impaction of the thrombus by pulsatile flow (Fig.1).
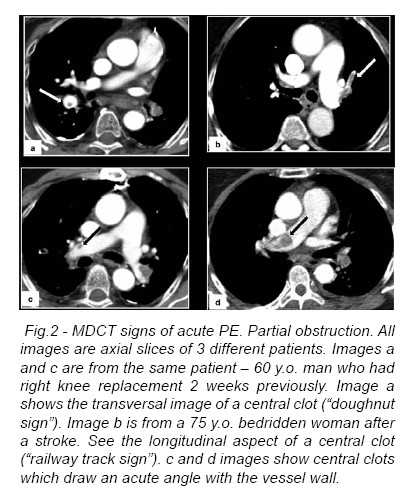
Nonobstructive Filling Defect
A nonobstructive filling defect may be central or eccentricin location. On angiography, a central filling defect is completely surrounded by contrast material. On CT, this finding is seen as a well-defined central filling defect in either an axial or a longitudinal plane with respect to the vessel. A nonobstructive central filling defect cannot float within the center of the lumen without physically touching the vessel wall and will be attached to either a nonobstructive eccentric filling defect or the thrombus of complete obstruction. In acute PE, a nonobstructing eccentric filling defect forms acute angles with respect to the vessel wall when seen on angiography orCT (Fig.2).
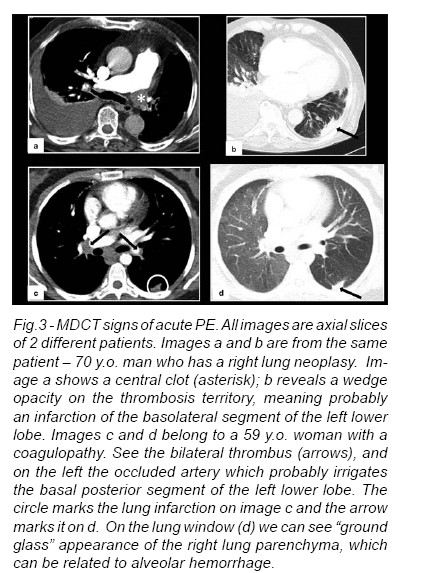
Areas of pulmonary infarction can also be present (Fig.3).
Indirect sign of acute Pe: nonuniform arterial Perfusion (3-5)
Oligemia, or a decrease in flow rate, due to acute PE is often identified on angiography. Nonunifor marterial perfusion due to acute PE can uncommonly manifest as a mosaic pattern of attenuation on CT. Occasionally, a large acute central PE can cause oligemia and a decrease in vessel diameter, which is reversible, can be seen on CT. The differential diagnosis of the indirect radiologic sign of nonuniform pulmonary arterial perfusion consists of congenital or acquired causes including chronic PE, emphysema, infection, compression or invasion of a pulmonary artery, atelectasis, pleuritis, and pulmonary venous hypertension.
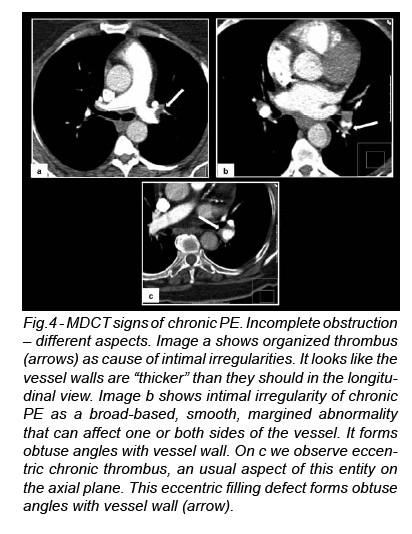
Direct signs of chronic Pe (3-5)
Complete obstruction
A decrease in the diameter of the vessel can be seen distal to the complete obstruction. This permanent reduction in vessel diameter is due to contraction of thrombus in chronic PE.
Nonobstructive Filling Defects
The organized thrombus of chronic PE can cause intimal irregularities, bands and webs, and abrupt vessel narrowing; any of these can lead to a pulmonary artery stenosis.
Intimal Irregularities
Intimal irregularities are broad-based, smooth, margined abnormalities that create obtuse angles with the vessel wall.They may beunilateral or bilateral. Pulmonary artery intimal irregularities can also be due to plaques secondary to pulmonary hypertension (Fig.4).
Bands and Webs
A band is defined as a delicate ribbonlike structure anchored to the vessel wall at two ends with a free unattached mid portion. A band generally ranges from 0.3 to 2 cm in length and from less than 0.1 to 0.3 cm in width. It is often orientated in the direction of blood flow along the long axis of the vessel. A web is a descriptive term for bands that have branches and form networks of varying complexity. Bands and webs are seen as thin lines surrounded by contrast material on angiography or CT.
Abrupt Vessel Narrowing
Abrupt vessel narrowing, often the result of recanalization,manifests imagiologically as an abrupt convergence of contrast material that leads to a thin column of intravascular contrast material distally.
Indirect signs of chronic Pe (3-5)
Poststenotic Dilatation
Poststenotic dilatation or aneurysm commonly occurs as a manifestation of chronic thromboembolic disease. The differential diagnosis includes congenital causes -for example, Marfan syndrome -or acquired causes. Acquired causes include mycotic aneurysms secondary to septic embolior adjacent pulmonary infection, pseudoaneurysms resulting from extra- or endovascular trauma (e.g., pulmonary artery catheterization),Behçet disease, and Takayasus arteritis.
Tortuous Vessels
Tortuous pulmonary vessels have been well described in patients with pulmonary artery hypertension. This radiologic sign is also seen in patients with pulmonary artery hypertension secondaryto chronic thromboembolic disease.
Enlargement of the Main Pulmonary Artery
Enlargement of the main pulmonary artery, greater than 33 mm,occurs in patients with precapillary, capillary, and postcapillary causes of pulmonary artery hypertension. This radiologic finding is commonly identified in patients with pulmonary artery hypertensionsecondary to chronic thromboembolic disease.
Enlargement of Bronchial Arteries
Enlarged bronchial arteries are often identified in patientswith chronic thromboembolic disease. Other causes of this finding include congenital vascular anomalies, bronchiectasis, acute or chronic lung abscesses, and mycobacterial and fungal infections. Enlargement of the bronchial artery collateral supply is easily seen on CT angiography but cannot be identified on conventional angiography of the pulmonary artery.
Nonuniform Arterial Perfusion
Chronic PE can cause a nonuniform arterial perfusion pattern identifiable on angiography and can manifest as a mosaic pattern of lung attenuation on CT. In addition, on CT one can see that the affected pulmonary arteries are permanently small relative to the accompanying bronchi and that unaffected arteries are often larger than their accompanying bronchi. The mosaic pattern of lung attenuation has two other major causes: small airways disease, in which the mosaic pattern of lung attenuation is accentuated by expiratory CT, and ground-glass opacification, in which it is not.
MR ANGIOGRAPHY (1,2) - Although a non-radiation exam modality, MR angiography still lacks spatial resolution and has not widespread use in acutely ill patients suspected of having PE, owing to lack of general availability, relatively long examination times, and difficulties in patient monitoring.
VENOUS ULTRASONOGRAPHY (1,2) -Ultrasonography of the deep venous system relies upon loss of vein compressibility as the primary criterion for DVT.
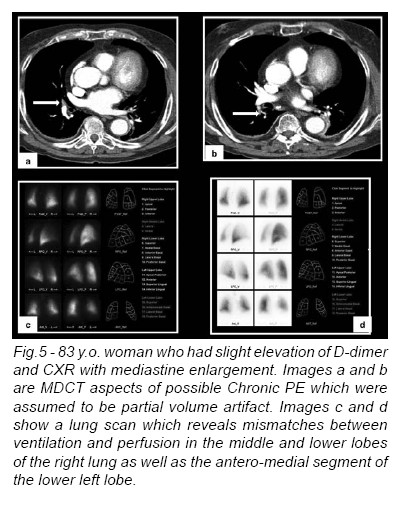
LUNG SCANNING (1,2) - Lung scanning is now a second-line diagnostic test for PE. It is mostly used for patients who cannot tolerate intravenous contrast. Small particulate aggregates of albumin labeled with a gamma-emitting radionuclide are injected intravenously and trapped in the pulmonary capillary bed. The perfusion scan defect indicates absent or decreased blood flow, possibly due to PE. Ventilation scans, obtained with radiolabeled (99mTc) inhaled gases such as xenon or krypton, improve the specificity of the perfusion scan. Abnormal ventilation scans indicate abnormal nonventilated lung, thereby providing possible explanations for perfusion defects other than acute PE, such as asthma or chronic obstructive pulmonary disease. A high probability scan for PE is defined as having two or more segmental perfusion defects in the presence of normal ventilation. The diagnosis of PE is very unlikely in patients with normal and near-normal scans but is about 90% certain in patients with high-probability scans. Unfortunately, most patients have nondiagnostic scans, and fewer than half of patients with angiographically confirmed PE have a high-probability scan. As many as 40% of patients with clinical suspicion for PE and low-probability scans do, in fact, have PE at angiography.
Forty-one percent of patients with PE have high probability scans and 87% of patients with this pattern have PE. In most clinical settings, a high-probability scan pattern may be considered positive for PE. These exams can particularly help on chronic PTE, which can be very difficult to recognize in imagiological exams (Fig.5).
Invasive diagnostic modalities
PULMONARY ANGIOGRAPHY (5) -Chest CT with contrast has virtually replaced invasive pulmonary angiography as a diagnostic test. Invasive catheter-based diagnostic testing is reserved for those in whom an interventional procedure such as catheter-directed thrombolysis or embolectomy is planned.Adefinitive diagnosis of PE depends upon visualization of an intraluminal filling-defect in more than one projection.
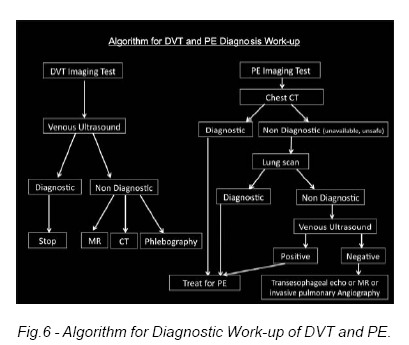
An Algorithm for Diagnostic Work-up can be defined (Fig.6).
Describe prognostic factors and identify-ing possible pitfalls
Clinical and Imagiological Identification of High-Risk
Patients
Estimation of acute PE clinical outcome in the International Cooperative Pulmonary Embolism Registry (ICOPER) and Management Strategy and Prognosis of Pulmonary Embolism Registry (MAPPET)studies underlined the importance of circulatory failure and systemic hypotension as predictors of poor prognosis. In patients with normal systolic arterial pressure, mortality increases with worsening of RV dysfunction.
The severity of PE can be also evaluated at CT by using different aspects, from the PE itself to upstream consequences and ultimately the origin of PE, namely venous thrombosis: (a) the obstruction of the pulmonary vascularbed;(b) the consequences of pulmonary vascular bed obstruction at the level of the heart; (c) upstream consequences at the level of abdominal and thoracic venous structures; and (d) the clot burden in lower limb and abdominal veins, which represents the risk for recurrent episodes of PE. Quantitative cardiac CT measurements obtained on axial CT images, namely the RV short axis, the LV short axis, and particularly the RV/LV short axes ratio, have shown a significant positive(RV short axis, RV/ LV diameter ratio) or negative (LV short axis) correlation with the severity of PE or with fatal outcome (6,7). An acute increase in volume and pressure in the right heart may be associated with raising diameters of the Superior Vena Cava and Azygos Vein (6,7).
Patient-related factors
Respiratory Motin Artifact Image Noise Pulmonary Artery Catheter Flow-related Artifact
Technical factors
Window Settings Streak Artifact Lung Algorithm Artifact Partial Volume Artifact Stair Step Artifact
Anatomic factors
Partial Volume Averaging Effect in Lymph Nodes Vascular Bifurcation Misidentification of Veins
Pathologic factors
Mucus Plug Perivascular Edema Primary Pulmonary Artery Sarcoma
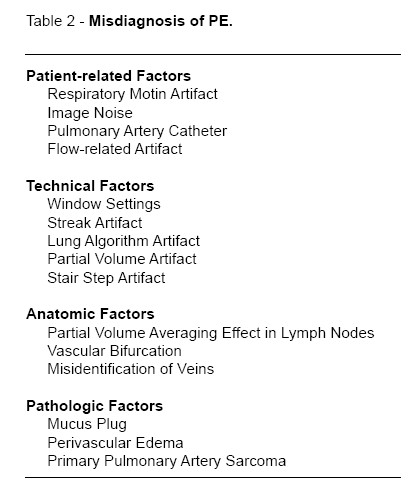
PITFALLS
A table listing potential pitfalls is given (Table 2
) and several cases illustrating them are presented (2,3). Never forget that besides PTE, there are other forms of PE, like gas and tumor embolism (8).
Conclusion
MDCT is determinant for the diagnosis of this entity with its direct and indirect signs. Differential diagnosis must be considered, as their treatment and prognosis might be very different. Image artifacts are among the worst pitfalls for the radiologist.
References
1 -Goldhaber S Z. Deep Venous Thrombosis and pulmonary Thromboembolism. In Harrison 17th edition. McGraw Hill. USA. 2007;256:1651-7. [ Links ]
2 -Gotway MB, Reddy GP, Dawn SK. Pulmonary Thromboembolic Disease. In Webb W. R., Higgins C. B. Thoracic Imaging: Pulmonary and Cardiovascular Radiology. Lippincott Williams and Wilkins. USA. 2005;27:609-29. [ Links ]
3 -Wittram C, Maher MM, Yoo AJ, Kalra MK, Shepard JA, McLoud TC. CT Angiography of Pulmonary Embolism: Diagnostic Criteria and causes of Misdiagnosis. Radiographics 2004;24:1219-38. [ Links ]
4 -Schoepf UJ, Costello P. CT Angiography for Diagnosis of Pulmonary Embolism: State of the art. Radiology 2004; 230:329-37. [ Links ]
5 -Wittram C, Kalra MK, Maher MM, Greenfield A, McLoud TC, Shepard JA. Acute and Chronic Pulmonary Emboli: Angiography-CT correlation. AJR 2006;186:421-9. [ Links ]
6 -Ghaye B, Ghuysen A, Bruyere P-J, DOrio V, Dondelinger RF, Can CT. Pulmonary Angiography Allow Assessment of Severity and Prognosis in Patients Presenting with Pulmonary Embolim? What the Radiologist Needs to Know; RadioGraphics 2006;26:23-39. [ Links ]
7 -Araoz PA, Gotway MB, Harrington JR, Harmsen WS, Mandrekar JN. Pulmonary Embolism: Prognostic CT Findings. Radiology 2007;242:889-97. [ Links ]
8 -Han D, Lee KS, Franquet T, Müller NL, Kim TS, Kim H. Thrombotic and Nonthrombotic Pulmonary Arterial Embolism: Spectrum of Imaging Findings. Radiographics 2003;23:1521-39. [ Links ]
Dr.ª Ana Sofia Preto
Serviço de Radiologia, Hospital de São João, Alameda Prof. Hernâni Monteiro, 4200-319 Porto. E-mail: sofiapreto@hotmail.com














