Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Arquivos de Medicina
versão On-line ISSN 2183-2447
Arq Med vol.27 no.3 Porto jun. 2013
CASOS CLÍNICOS/SÉRIE DE CASOS
Obstructive sleep apnea manifested as an atypical major depressive disorder: a case report and review of the literature
Apnéia obstrutiva do sono manifestada como episódio depressivo atípico: um caso clínico e revisão da literatura
Rui Lopes1, Jacinto Azevedo1,2, Rosário Curral1,2, Manuel Esteves1,2, Rui Coelho1,2, António Roma-Torres1
1Clinic of Psychiatry and Mental Health, Centro Hospitalar de São João, Porto
2Department of Clinical Neurosciences and Mental Health, Faculty of Medicine, University of Porto, Porto
ABSTRACT
Background: Sleep disorders can be related to loss, disruption or inappropriate day-night rhythm of sleep and represent a great economic burden, involving morbidity and mortality. The insomnia or hypersomnia, secondary to a psychiatric disorder such as depression or psychosis, is frequent in psychiatric practice. Moreover, although uncommon, primary sleep disorders can also cause psychological or psychiatric problems, with some interdependence, which is not completely understood.
Case presentation: A 48-year-old woman presented atypical depressive symptoms resistant to antidepressants. In this atypical state, she also showed excessive daytime sleepiness (EDS), snoring, daytime naps and cognitive symptoms. After a sleep study with polysomnography, an obstructive sleep apnea (OSA) manifested as atypical depression was diagnosed. Remission of depressive symptoms was verified with additional continuous positive airway pressure (CPAP) therapy.
Conclusion: The awareness that OSA could be presented as an atypical depression allows its early detection and treatment, and possibly the prevention of numerous medical disorders. Psychiatrists and General Practitioners should be familiar with sleep disorders and psychiatric co-morbidities.
key-words: Sleep disorders, obstructive sleep apnea, disorders of excessive somnolence, depression, mental disorders
RESUMO
Contexto: As perturbações do sono podem estar relacionadas com a perda, desregulação ou inadequação do ritmo do ciclo sono-vigília, traduzindo-se em consequências económicas importantes a nível de morbilidade e mortalidade. A insónia ou hipersónia secundárias a uma doença psiquiátrica, como a depressão ou a psicose, são frequentes na prática clínica em psiquiatria. Por outro lado, e embora incomum, as perturbações do sono primárias também podem originar problemas psicológicos ou psiquiátricos, numa interdependência ainda não totalmente esclarecida.
Caso clínico: Mulher de 48 anos apresenta sintomatologia depressiva atípica resistente a antidepressivos, acompanhada por sonolência excessiva diurna, ressonar (roncopatia), adormecimentos diurnos e sintomas cognitivos. Após a realização de estudo do sono com polissonografia foi diagnosticado apneia obstrutiva do sono (AOS) manifestada como depressão atípica. A instituição adicional de terapia por pressão positiva contínua nas vias aéreas (continuous positive airway pressure, CPAP) originou a remissão dos sintomas depressivos.
Conclusão: A sensibilização para a apresentação da AOS como depressão atípica permite a sua detecção e tratamento precoces e, possivelmente, a prevenção de várias condições médicas. Os Psiquiatras e Médicos de família devem estar familiarizados com as perturbações do sono e comorbilidades psiquiátricas.
Palavras-chave: Perturbações do sono, apneia obstrutiva do sono, perturbações do sono por sonolência excessiva, depressão, perturbações mentais
BACKGROUND
There is an inherent need for sleep recognized in almost every mammal and humans spend almost one third of their life sleeping. This normal yet altered state of consciousness is defined by a complex physiologic pattern of sleep phases.1 The changes in the sleep -wake cycle can have an impact on health and on peoples day-time living.2
At least one in 10 persons suffer with a sleep-related problem.3, 4 Sleep disorders can affect mental and emotional functions, causing fatigue, poor concentration and depressive symptoms.5-7 A prolonged sleep disturbance can cause disorientation, illusions, hallucinations, persecutory ideas and cognitive impairments.7
Mental disorders and their treatment can interfere with the sleep-wake cycle as well. Initial insomnia, early morning wakening, disturbing dreams and day-time fatigue are frequently observed in major depression.8 Sometimes hypersomnia can also appear in atypical depressive cases, bipolar affective disorder and seasonal affective disorder.6 Alterations on rapid eye movement (REM) sleep latency are frequently noticed in certain forms of severe depression7 and sleep deprivation is reported as having an antidepressant effect and may precipitate the onset of a manic episode.6 Interestingly, the symptoms of sleep disorders are sometimes wrongly evaluated as psychiatric disorders, such as depression. This fact, together with the non-recognition of sleep disorder symptoms, can compromise their appropriate diagnosis and treatment.
We present a clinical case of an OSA with an atypical major depressive disorder symptoms presentation. The appreciation of depression in OSA has been reported earlier in the literature,9 But its aetiology remains unclear.10 Although there is a higher prevalence of depression in OSA,10-13 the underappreciation of this association in medical practice can sometimes cause undesirable medical disorders, such as high blood pressure, that could otherwise be treated.
The importance of this connection for primary care and for mental health clinicians is related to the overlap of symptoms and consequently to the under-diagnosis of OSA and other sleep disorders in depressed patients.10, 14 besides, this overlap of symptoms represents a challenge for correct diagnosis and management.15 This case report illustrates that the non-identification of OSA in a depressive patient can influence the process of treatment and/ or contributes to its antidepressant treatment failure, thus highlighting for the importance of assessment using a sleep study with polysomnography in a more regular basis.
CASE REPORT
Our patient is a 48-year-old woman, single, living with her two children, office assistant. She is the second of four sisters and a brother, in a family of middle socioeconomic status. She was born by eutocic birth and had a normal psychomotor development with no reports of relevant health problems. At the age of six, she enrolled in elementary school, completed the 4th grade when she was 11 years old and was a sociable girl. She began working at the age of 13 in a shoe factory till she was 26, when she started working as an office assistant. She had her first daughter when she was 28 years old and her second daughter five years later.
She has no personal history of smoking, alcohol or toxic substance misuse. She suffers from hypertension, being medically treated with losartan50mg/day. Concerning psychiatric antecedents, she had two previous reactive depressive episodes related to important life-events; the first one occurred when patient was 15 years old after her best friend suddenly died by a cerebral neoplasm, and the second depressive episode occurred at 34 years old when his brother suddenly hanged by suicide. Both episodes remitted following a brief course of antidepressant treatment of 9 months. The patient denied hypomanic or manic episodes.
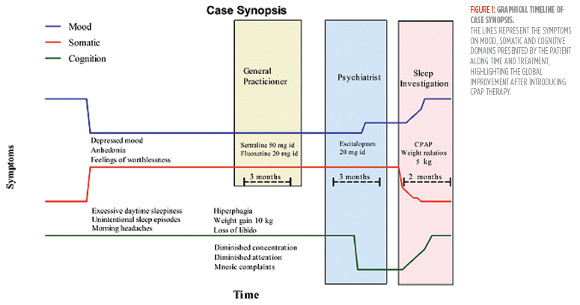
Recently, by the age of 46, she started feeling progressively sad, with anhedonia, fatigue, hyperphagia (with a weight gain of 10 kg in one year), leaden paralysis, dizziness with sensation of fainting, subjective experience of amnesia complains (she often forgot names and codes related to work), morning headaches and difficulties in attention and concentration at work. She also reported snoring (identified by her daughters), EDS and unintentional sleep episodes occurring while watching television, reading, or even when working. After beginning to miss days at work, she started complaining to her General Practitioner, who diagnosed a recurrence of her depression and started treatment, first with sertraline 50 mg/day and then with fluoxetine 20 mg/day. Because of symptoms unimprovement, she was sent to psychiatric ambulatory treatment by her General Practitioner (Figure 1).
On the mental examination, the patient was alert, cooperative and calm and showed time and space orientation. Her speech was coherent and logical. There was good emotional resonance but she had a depressive mood. She did not have any changes in thought content, such as suicidal or delusional ideas. No sense-perception changes were observed either. Insight and critical appraisal were preserved. She described herself as being shy, quiet, introverted and sensitive to interpersonal rejection.
The physical examination showed an overweight woman with a body mass index (BMI) of 31.3Kg/ m2. Neurological examination was normal, the same happening with blood investigations (hemogram, basic biochemical investigations, illicit drug screen and thyroid function). There were no relevant alterations in the electroencephalogram (EEG) and in cerebral magnetic resonance imaging (MRI) results, as well as in the mini-mental state examination (MMSE).
We switched the antidepressant treatment to escitalopram 20 mg/day. Although there was some slight improvement in sadness and anhedonia after three months, the patient maintained the symptoms of snoring, EDS, unintentional napping episodes, cognitive symptoms and morning headaches, and was referred for a sleep study. Here, on a more detailed physical examination, the patient revealed a partial obstruction of the nose and a Mallampati score of 4. She scored 23 on the Epworth sleepiness scale (ESS), had a desaturation index of 18.8/h on overnight pulse oximetry (min. of 84%, average of 95%), and had an apnea-hypopnea index (AHI) of 16.3/h on polysomnography. There were no reports of circadian rhythm alterations, nocturnal insomnia, sleep fragmentation or restless legs symptoms.
She started the treatment with nightly CPAP therapy (10cm of H20 pressure), and carried out lifestyle changes and weight-loss education and diet. Although patient had some initial difficulties in the adherence due to leakage and nocturnal awakenings (median use = 2 hours; use above 4 hours = 12%), a progressive and substantial improvement of depressive symptoms occurred during the next 8 weeks after ventilation mask readjustment (Figure 1). Sadness and anhedonia were now in remission. The patient had lost 5 kg (BMI of 29.3 Kg/m2) and there was also a symptomatic improvement in EDS (ESS = 12), snoring, nappings, morning headaches and also an increase in attention and concentration. The patient mentioned a better subjective quality of life and had now no work absence and after six months, our patient remained euthymic.
DISCUSSION
Our presumptive diagnosis is OSA, presenting as an atypical depression episode. Several studies have identified depressed mood has a symptom of untreated OSA. Although it has been documented higher prevalence of depression in patients with OSA, an etiological link between the two entities has not entirely demonstrated.10, 16, 17 OSA is a sleep-related breathing disorder and is one the most commonly diagnosed sleep problems (lifetime prevalence is between 4% and 9%),18 although still under-diagnosed.10 It is associated with several medical conditions19-21 and increases motor vehicle accidents.22 besides, it represents an important impact in terms of healthcare burden and also in morbidity and mortality.23-27 Severe and untreated OSA(AHI=30) can increase 3 to 6 times the risk of all-cause mortality, compared with individuals without OSA.26-28 Typically, a transient upper airway complete or partial occlusion occurs as sleep deepens, resulting in oxygen deprivation. the subsequent arousal prevents the deeper stages of slow wave sleep, a condition that may happen hundreds of times a night.29 The patient is usually unaware of snoring, respiratory pauses and their severity.24 Sometimes this information is provided by family orbed partners.7
Our patient had two previous episodes of major depression with characteristic mood reactivity for life-events that were successfully treated with antidepressants. In the present depressive episode, along with features of atypical depression (such as sadness, anhedonia, EDS, leaden paralysis, hyperphagia and oversensitivity to interpersonal rejection), she also showed snoring, unavoidable episodes of napping during the day, difficulties in attention and concentration and morning headaches. Although there was an improvement in some depressive clinical features with the escitalopram 20 mg/day treatment, the persistence of EDS associated with snoring, morning headaches, naps during the day and cognitive symptoms made us consider another possible aetiology or comorbid condition.
In the presence of EDS several common disorders must be considered, but the most frequent are sleep disorders.30 The first step towards the evaluation of a sleep disorder is a complete throughout physical, medical, psychiatric assessment and also a vigorous evaluation of sleep complaints.7 As leep diary can be useful in providing information about daily sleep patterns.31, 32
A polysomnography with respiratory variables is a first-line diagnostic approach when suspecting of a sleep disorder. OSA can be diagnosed in asymptomatic adults if the AHI is greater than 15 events per hour, and in symptomatic adults (loud snoring, daytime sleepiness, apneic episodes, frequent arousals, impaired cognition) if the AHI is greater than five events per hour. Subgroups based on OSA severity were categorized into three groups according to the AHI: AHI < 15/h (mild OSA), AHI < 30/h (moderate OSA) and AHI = 30/h (severe OSA).30, 33, 34 The patient had and an AHI of 16.3/h on polysomnography, corresponding to a moderate OSA.
Several signs in the patients physical examination were also suggestive of OSA, such as mouth breathing and partial nasal obstruction during inspiration, revealed by the bilateral collapse of the nasal rim. This is often a sign of OSA-associated nasal resistance, due to higher inspiratory upper airway pressure and increased collapsibility of pharyngeal walls,35 And a potential cause of sleep apnea due to a predisposition to mouth breathing and the downward and backward displacement of the mandible.36 The patient also had the Mallampatis score of 4, which is a classification system based on visualization of posterior or opharyngeal structures. The highest Mallampatis score of 4 indicates a not visible soft palate and a crowded oropharyngeal space, predisposing to obstruction during sleep.37, 38 The combination of nasal obstruction and a high Mallampatis score (3 or 4) is associated with an increased risk of sleep apnea.39, 40 She was also overweight (BMI of 31.3kg/m2), which is a predisposing factor for the development of OSA. Middle age, hypothyroidism, maleness, neurological conditions and malformations that impair upper airway muscle tone are other predisposing factors.41
The repeated periods of hypoxia, hypercapnia and sleep fragmentation of OSA can lead to cardiorespiratory complications, such hypertension, heart arrhythmias and sudden death,19, 42, 43 cerebrovascular disease and poor cognitive performance,44, 45 especially when AHI > 30 per hour of sleep.28 These events during sleep can also be an explanation to the EDS and the cognitive symptoms, as well as to the morning headaches reported by the patient. OSA can possibly represent an increased risk for the development of the patient´s hypertension.28 The variability of symptoms presentation does not necessarily reflect the duration and severity of OSA.10 The severity of EDS due to OSA does not necessarily reflect a high AHI either,10 but can be more associated with depressive symptoms.13 Also, although fatigue might be present in OSA or in depression, depressive symptoms have been independently associated with more expressive levels of fatigue in OSA patients.15, 46, 47
EDS can be assessed by a multiple sleep latency test, used to diagnose narcolepsy, or using questionnaire scales. Our patient had 23 on ESS (maximal value is 24 and a score > 10 is considered sleepy).48 This apparently severe EDS can be responsible for mood and behavioural consequences,14, 46 interpersonal difficulties,49 impaired driving ability,50 and lowered health-related quality of life (Qol).51-53 further, it has been found a positive association between depression and obesity with sleepiness and Qol scores in patients with OSA.54
OSA has been associated with depression and also to other psychiatric diagnosis.55-58 Emerging evidence points to a high prevalence of depressive symptoms in patients with OSA, suggesting a mutual relationship.11-13 According to recent revisions, it may ranges from 5 to 63%.10,11,59 Although male sex has been considered a predictor of OSA severity, together with older age and high BMI,60 in patients with depression and OSA the severity of depressive and anxiety symptoms seems to be higher in females than in males.61, 62 A higher frequency of OSA among patients diagnosed with major depression60 and a significant positive correlation between OSA severity and depressive symptoms severity have also been reported.63 Additionally, OSA seems to be higher in individuals presenting both depression and insomnia than in patients with depression or insomnia alone.60
An hypothetical link between OSA and depression is still not demonstrated55, 64 and, despite studies reporting a mutual connection,63, 65 the pathophysiological mechanisms of that relationship remain unclear and seem complex.10 Disturbance of the sleep/ wake cycle, wakefulness and regulation of mood in both entities can be interrelated with abnormalities in neurotransmitters (serotonin, norepinephrine and gamma-aminobutyric acid -GABA), neurotransmission, neuroplasticity and to inflammatory substances and cytokines.10 It has also been suggested that serotonin can influence upper airway patency through the hypoglossal nucleus.10
In our patient, depressive symptoms presented at the same time with other symptoms of OSA, and the overlapping symptoms of both entities, such as EDS, fatigue, poor concentration, psychomotor retardation and weight gain can represent a diagnostic challenge and lead to misdiagnosis.14 Due to the overlap of symptoms, we cannot affirm that OSA was solely the cause of the depressive mood itself, or that some symptoms of OSA were independent of the atypical depression. nevertheless, a hypothetical comorbid and synergistic action of both entities can be present.10 Moreover, it can be the result of repeated episodes of hypoxia or to fragmentation of sleep,66 or to multivariable confounding factors such as obesity, hypertension, cardiovascular disease and metabolic syndrome, associated with both entities.10 nevertheless, in this patient and after CPAP institution, the depressive symptoms and EDS, snoring, naps, morning headaches and cognitive symptoms had a great improvement. After eight weeks, depressive symptoms were in remission and the others have improved substantially, the patient returned to work at full time, suggesting that OSA could be the cause of previous antidepressant treatment failure and possibly contributed to exacerbate the depressive symptoms. Therefore, awareness of this relationship is still important for a better diagnosis and treatment in both entities. A study also reported that in depressed patients following an acute myocardial infarction (MI) and with OSA, cognitive behaviour therapy is less efficacious compared to patients whithout OSA, therefore highlighting that OSA could decrease the antidepressant treatment response.67
The subjective neurocognitive symptoms presented by the patient, such as impaired attention and memory together with poor concentration, reversed mostly after treatment. Deficits in executive functions in OSA patients are sometimes not completely reversed when sleepiness is relieved by treatment due to irreversible anoxic brain changes (neuronal cell injury, neurodegeneration, and cell death)68 and vasculopathy.69 This may be associated to hippocampus atrophy and abnormalities in white matter, particularly in frontal lobes.70,71 Cases of dementia due to grey-matter loss and alterations in markers of neuronal integrity were also evidenced by neuroimaging studies.72 It has been also documented that depression in OSA patients seems to add additional damage in affective, cognitive, respiratory, and autonomic control brain regions.73
Other conditions can be responsible for the EDS, which should be considered in the differential diagnosis. but, the normal findings on thyroid-stimulating hormone, ferritin, cobalamin, folate, full blood cell count, EEG, cerebral MRI and MMSE make a possible medical, neurological or substance abuse sleep related disorder less likely to be present. In this patient, the apneas or hypopneas could be a manifestation of central apnea, a condition involving impairment of the respiratory drive, but in this situation there is usually an absence of snoring, the respiratory pauses are not accompanied by respiratory efforts and insomnia is present more often than EDS.3 There is an absence of sleep attacks, cataplexy, hypnagogic hallucinations and sleep paralysis suggestive of narcolepsy,74 and an absence of an actual external oscillator, responsible for a circadian rhythm disorder. Besides, there are not clinical elements suggestive of parasomnias or of a psychophysiological, paradoxical andidiopathic hypersomnia, or restless legs syndrome.
TREATMENT
The treatment goals for OSA include measures towards reducing the number of apneic episodes, improvement of symptoms and oxygen saturation. night-time nasal CPAP, maintaining the patency of the oropharynx through an air stream under pressure, is the most successful treatment.75 It can greatly improve the patients functional status, providing efficient oxygenation and restorative sleep,76 reducing blood pressure,77 improving cognitive deficits78 and raising the number of years of good health by 5.5 quality-adjusted life-years.8 There is also evidence that positive pressure therapy may be an appropriate treatment for mood disorders when they are related to sleep disordered breathing.79-86 Some authors even suggest that CPAP should be tried first, before starting other treatment modalities for depression.87 nevertheless, there have also been trials, though with negative findings on the improvement of depression, with treatment of apnea, but CPAP adherence in these last studies was not monitored.88-91 In fact, high scores on depression and anxiety in OSA patients have been associated to non-compliance with CPAP therapy.92 Patients tend to abandon CPAP therapy early, so monitorization, support and mask education should be directed towards sustaining adherence,77 as occurred with this patient. Recent evidence shows that telemonitoring, in a self-management and self-behaviour approach93 can be effective by increasing adherence.
Apparently no pharmaco-therapy is consistently effective in normalizing sleep in these patients. Central nervous system depressants (alcohol, benzodiazepines, zolpidem) should be avoided, due to respiratory depression and weaker respiratory response to hypoxia.94, 95 Other measures such dental devices or oropharyngeal exercises have also been reported to be usefull, althouth with limited evidence.
The usefulness of antidepressants in patients with OSA and comorbid depression is not extensively studied. Nonetheless, the improvement of sleep apnea (reduction of the frequency of apneas and increase in oxygen saturation) with some antidepressants is related to their REM-suppressant activity, the sleep stage in which most apneas occur. Evidence of these properties was demonstrated with tricyclic antidepressants, protriptyline and imipramine. Fluoxetine and paroxetine (serotonin-specific reuptake inhibitors -SSRIs) have shown similar results, yet causing fewer adverse effects.24, 96 The treatment of EDS is better with more stimulating antidepressants, such as SSRIs, reboxetine or bupropion. Mirtazapine and trazodone are not recommended97because of their sedating properties.98
Because of their sedative effects, antihistamines should not be used either, but some non-sedating antihistamines, however, can be useful for allergic rhinitis and relieve obstruction.99 Modafinil, a wakefulness-promoting agent,100, 101 improves the quality of episodic memory and attention, but should be used only after CPAP has been instigated and maximized and after the exclusion of other causes of sleepiness.102 More recently, it has been also demonstrated the usefulness of armodafinil, another nonamphetamine wakefulness-promoting agent, for treating excessive sleepiness in patients with OSA and comorbid depression.103
Surgical procedures are reserved for CPAP treatment failures or anatomic correction of selected cases to increase posterior airway space (nasal reconstruction, tonsillectomy, uvulopalatopharyngoplasty, mandibular advance and rarely tracheostomy).104 Lifestyle changes, particularly weight loss, or avoidance of a supine sleeping position may affect the severity of OSA.105 Education about normal sleep and habits of good sleep hygiene are also important measures.106
CONCLUSION
Sleep disorders are not still well recognized and treated, representing important sources of disease, disability and even death. A case with an improvement in depressive symptoms after treatment with escitalopram but with the persistence of EDS, snoring, naps and cognitive symptoms led us to a careful evaluation of a possible sleep disorder. After the diagnosis of OSA, an additional treatment with CPAP was initiated. Then, the clinical picture ameliorated towards a full remission of depressive symptoms and a substantial improvement of the others, making us consider an OSA case with an atypical depressive syndrome presentation.
A detailed diagnostic interview and a physical examination, complemented with a polysomnography, were essential for diagnosis of OSA. Careful management of OSA together with depression should regard to sleep disorder itself but also to depressive symptoms. for that, CPAP is essential, but treatment requires particularly careful consideration, when choosing antidepressants. A behavioural approach, including lifestyle modifications (weight loss) and hygiene sleep measures must also be considered. Benzodiazepines and sedating antidepressants should be avoided. Other drugs such as modafinil may be a promise in the future. Surgery is used in special anatomical situations.
An early intervention and prevention are essential to an easier and well-succeeded recovery, as well as for costs reduction and improvement in life quality, avoiding undesirable medical and social consequences. In particular, the early recognition and assessment of atypical depressive symptoms refractory to different antidepressants, along with other symptoms suggesting the presence of an OSA should prompt to a sleep study investigation. This case highlights the relationship between OSA and depressive disorders, a field that needs more investigation and General Practitioners and Psychiatrists should be familiar with this health problem.
ACKNOWLEDGEMENTS
We would like to thank the patient for her collaboration. The authors also wish to thank Professor Leonor Duarte for her kind help in revising the english in the article.
REFERENCES
1. Stevens S, Henning WA. Sleep and Wakefulness. In: Goetz CG, ed. textbook of Clinical neurology. Philadelphia: Elsevier Saunders; 2007:20-33. [ Links ]
2.Krahnl E, Richardson JW. Sleep Disorders.In: Levenson Jl, ed. The American Psychiatric Publishing text book of Psychosomatic Medicine. Washington: American Psychiatric Publishing;2005:335-57. [ Links ]
3.Jackson CW,Curtis Jl. Sleep Disorders. In: DiPiro Jt, Talbert Rl,Yee GC, Matzke GR, Wells BG, Posey LM, eds. Pharmacotherapy: A Pathophysiologic Approach. Sixthed. New York: Mcgraw-Hill Medical Publishing Division; 2005:1321-2. [ Links ]
4. National Center on Sleep Disorders Research: 2003 national Sleep Disorders Research Plan. U.S. Washington: Department of Health and Human Services; 2003. [ Links ]
5. Bonjean M,StepnowskyC, Dang-vu Tt ,Sejnowski tJ, Maquet P. Sleep Medicine and Sleep Disorders. In: Carlstedt RA, ed. Handbook of Integrative Clinical Psychology, Psychiatry, and behavioral Medicine: Perspectives, Practices, and Research. New York: Springer Publishing Company; 2010:95-152. [ Links ]
6. Semple D, Smith R. Oxford Handbook of Psychiatry. 2nd ed: Oxford university Press; 2009. [ Links ]
7. Stores G. Sleep-wake disorders. In: Gelder MG, Andreasen NC, Jr JJl-I, Geddes JR, eds. New Oxford textbook of Psychiatry. 2nd ed. Oxford, New York: Oxford university Press; 2009:924-33. [ Links ]
8. Leger D. Public health and insomnia: economic impact. Sleep. 2000;23(Suppl 3):S69-76. [ Links ].
9. Guilleminault C, Eldridge Fl, Tilkian A, Simmons Fb, Dement WC. Sleep apnea syndrome due to upper airway obstruction: a review of 25 cases. Arch Intern Med. 1977;137(3):296-300. [ Links ]
10. Ejaz SM, Khawaja IS, Bhatia S, Hurwitz TD. Obstructive sleep apnea and depression: a review. Innov Clin neurosci. 2011;8(8):17-25. [ Links ]
11. Wheaton AG, Perry GS, Chapman DP, Croft Jb. Sleep disordered breathing and depression among U.S. adults: national Health and nutrition Examination Survey, 2005-2008. Sleep. 2012;35(4):461-7. [ Links ]
12. Deldin PJ, Phillips LK, Thomas RJ. A preliminary study of sleep-disordered breathing in major depressive disorder. Sleep Med. 2006;7(2):131-9. [ Links ]
13. Ishman Sl, Cavey RM, Mettel Tl, Gourin CG. Depression, sleepiness, and disease severity in patients with obstructive sleep apnea. Laryngoscope. 2010;120(11):2331-5. [ Links ]
14. Kryger MH, Roth t, Dement WC. Principles and Practice of Sleep Medicine. 5th ed. St. louis, Mo: Elsevier, Saunders; 2011. [ Links ]
15. Bardwell WA, Ancoli-Israel S, Dimsdale JE. Comparison of the effects of depressive symptoms and apnea severity on fatigue in patients with obstructive sleep apnea: a replication study. J Affect Disord. 2007;97(1-3):181-6. [ Links ]
16. Lang fu, Hosch H, Seibert H, Klug R, Koppler D, Jager M. [Obstructive sleep apnoea syndrome as the cause of atypical depression]. Fortschr neurol Psychiatr. 2011;79(9):531-4. [ Links ]
17. Krahn lE, Miller bW, Bergstrom LR. Rapid resolution of intense suicidal ideation after treatment of severe obstructive sleep apnea. J Clin Sleep Med. 2008;4(1):64-5. [ Links ]
18.Stepnowski C, Bonjean M.Ane-Health Approach to the Management of Chronic Sleep Disorders. In: Carlstedt RA, ed. Handbook of Integrative Clinical Psychology, Psychiatry, and behavioral Medicine Perspectives, Practices, and Research. New York: Springer Publishing Company; 2010:779-806. [ Links ]
19. Somers VK, White DP, Amin R, Abraham Wt, Costa F, Culebras A, Daniels S, Floras JS, Hunt CE, Olson LJ, Pickering TG, Russell R,Woo M, Young t. Sleep apnea and cardiovascular disease. Circulation. 2008;118(10):1080-111. [ Links ]
20. Valham F, Mooe T, Rabben T, Stenlund H, Wiklund U, Franklin KA. Increased risk of stroke in patients with coronary artery disease and sleep apnea: a 10-year follow-up. Circulation. 2008;118(9):955-60. [ Links ]
21. Yaggi HK, Concato J, Kernan Wn, Lichtman JH, brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353(19):2034-41. [ Links ]
22. George Cf. Sleep apnea, alertness, and motor vehicle crashes. Am J Respir Crit Care Med. 2007;176(10):954-6. [ Links ]
23. Day R, Gerhardstein R, Lumley A, Roth T, Rosenthal L. The behavioral morbidity of obstructive sleep apnea. Prog Cardiovasc Dis. 1999;41(5):341-54. [ Links ]
24. Grunstein RR, Hedner J, Grote L. Treatment options for sleep apnoea. Drugs. 2001;61(2):237-51. [ Links ]
25. Lavie P, Herer P, Peled R, Berger I, Yoffe N, Zomer J, Rubin AH. Mortality in sleep apnea patients: a multivariate analysis of risk factors. Sleep. 1995;18(3):149-57. [ Links ]
26. .Marshalln S, Wong KK, Liu PY, Cullen SR, Knuiman MW, Grunstein RR. Sleep apnea as an independent risk factor for all- cause mortality:the busselt on Health Study. Sleep.2008;31(8):1079-85. [ Links ]
27. Young T, Finn L, Peppard PE, Szklo-Coxe M, Austin D, Nieto FJ, Stubbs R, Hla KM. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep. 2008;31(8):1071-8. [ Links ]
28. Punjabi NM, Caffo BS, Goodwin Jl, Gottlieb DJ, Newman Ab, OConnor Gt, Rapoport DM, Redline S, Resnick HE, Robbins JA, Shahar E, Unruh Ml, Samet JM. Sleep-disordered breathing and mortality: a prospective cohort study. PlOS Med. 2009;6(8):e1000132. [ Links ]
29. Flemons WW. Clinical practice. Obstructive sleep apnea. N Engl J Med. 2002;347(7):498-504. [ Links ]
30. American Academy of Sleep Medicine. The International Classification of Sleep Disorders: Diagnostic and Coding Manual. 2nd ed. Westchester, Il: American Academy of Sleep Medicine; 2005. [ Links ]
31. Christodoulou C, Allister WSM, Krupp Lb. Fatigue. In: Jeste Dv, friedman JH, eds. Current Clinical neurology: Psychiatry for neurologists. totowa: Humana Press; 2006:295-306. [ Links ]
32. Mercer JD, Bootzin RR, Lack LC. Insomniacs perception of wake instead of sleep. Sleep. 2002;25(5):564-71. [ Links ]
33. George CFP. Screening and Case finding. In: Culebras A, Ivanenko A, Kushida CA, Watson nf, eds. Obstructive Sleep Apnea, Diagnosis and treatment. New York: Informa Healthcare USA; 2007:21-34. [ Links ]
34. American Academy of Sleep Medicine. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, terminology and technical Specifications. Westchester, Il: American Academy of Sleep Medicine; 2007. [ Links ]
35. Rombaux P, Liistro G, Hamoir M, Bertrand B, Aubert G, Verses T, Rodenstein D. Nasal obstruction and its impact on sleep-related breathing disorders. Rhinology. 2005;43(4):242-50. [ Links ]
36. Zonato AI, bittencourt LR, Martinho Fl, Junior Jf, Gregorio LC, Tufik S. Association of systematic head and neck physical examination with severity of obstructive sleep apnea-hypopnea syndrome. laryngoscope. 2003;113(6):973-80. [ Links ]
37. Zonato AI, Martinho Fl, Bittencourt LR, de Oliveira Campones Brasil O, Gregorio LC, Tufik S. Head and neck physical examination: comparison between nonapneic and obstructive sleep apnea patients. Laryngoscope. 2005;115(6):1030-4. [ Links ]
38. Friedman M, Tanyeri H, La Rosa M, Landsberg R, Vaidyanathan K, Pieri S, Caldarelli D. Clinical predictors of obstructive sleep apnea. Laryngoscope. 1999;109(12):1901-7. [ Links ]
39. Liistro G, Rombaux P, Belge C, Dury M, Aubert G, Rodenstein DO. High Mallampati score and nasal obstruction are associated risk factors for obstructive sleep apnoea. Eur Respir J. 2003;21(2):248-52. [ Links ]
40. Tsai WH, Remmers JE, Brant R, Flemons WW, Davies J, Macarthur C. A decision rule for diagnostic testing in obstructive sleep apnea. Am J Respir Crit Care Med. 2003;167(10):1427-32. [ Links ]
41. Young t, Palta M, Dempsey J, Skatrud J, Weber S, badr S. The occurrence of sleep-disordered breathing among middle-aged adults. n Engl J Med. 1993;328(17):1230-5. [ Links ]
42. Gottlieb DJ, Yenokyan G, Newman Ab, OConnor Gt, Punjabi NM, Quan Sf, Redline S, Resnick HE, Tong EK, Diener-West M, Shahar E. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation. 2010;122(4):352-60. [ Links ]
43. Redline S, Yenokyan G, Gottlieb DJ, Shahar E, OConnor Gt, Resnick HE, Diener-West M, Sanders MH, Wolf PA, Geraghty EM, Ali T, Lebowitz M, Punjabi NM. Obstructive sleep apneahypopnea and incident stroke: the sleep heart health study. Am J Respir Crit Care Med. 2010;182(2):269-77. [ Links ]
44. Shepard JW, Jr. Hypertension, Cardiac arrhythmias, myocardial infarction, and stroke in relation to obstructive sleep apnea. Clin Chest Med. 1992;13(3):437-58. [ Links ]
45. Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342(19):1378-84. [ Links ]
46. Jackson Ml, Stough C, Howard ME, Spong J, Downey lA, Thompson b. The contribution of fatigue and sleepiness to depression in patients attending the sleep laboratory for evaluation of obstructive sleep apnea. Sleep breath. 2011;15(3):439-45. [ Links ]
47. Bardwell WA, Moore P, Ancoli-Israel S, Dimsdale JE. fatigue in obstructive sleep apnea: driven by depressive symptoms instead of apnea severity? Am J Psychiatry. 2003;160(2):350-5. [ Links ]
48. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540-5. [ Links ]
49. Grunstein RR, Stenlof K, Hedner JA, Sjostrom l. Impact of self-reported sleep-breathing disturbances on psychosocial performance in the Swedish Obese Subjects (SOS) Study. Sleep. 1995;18(8):635-43. [ Links ]
50. Findley lJ, Suratt PM, Dinges Df. Time-on-task decrements in steer clear performance of patients with sleep apnea and narcolepsy. Sleep. 1999;22(6):804-9. [ Links ]
51. Flemons WW. Measuring health related quality of life in sleep apnea. Sleep. 2000;23 Suppl 4:S109-14. [ Links ]
52. Parish JM, Lyng PJ. Quality of life in bed partners of patients with obstructive sleep apnea or hypopnea after treatment with continuous positive airway pressure. Chest. 2003;124(3):942-7. [ Links ]
53. Vaughn Bv, Bazil CW. Sleep Disorders. In: Rowland LP, Pedley TA, eds. Merritts neurology. twelfth ed. Philadelphia: lippincott Williams & Wilkins Publishers; 2010:967-74. [ Links ]
54.Pamidi S, Knutson Kl, Ghod Sf, Mokhlesi B. Depressive symptoms and obesity as predictors of sleepiness and quality of life in patients with REM-related obstructive sleep apnea: cross-sectional analysis of a large clinical population. Sleep Med. 2011;12(9):827-31. [ Links ]
55. Baran AS, Richert AC. Obstructive sleep apnea and depression. CNS Spectr. 2003;8(2):128-34. [ Links ]
56. Sharafkhaneh A, Giray N, Richardson P, Young T, Hirshkowitz M. Association of psychiatric disorders and sleep apnea in a large cohort. Sleep. 2005;28(11):1405-11. [ Links ]
57. Andrews JG, Oei TP. The roles of depression and anxiety in the understanding and treatment of Obstructive Sleep Apnea Syndrome. Clin Psychol Rev. 2004;24(8):1031-49. [ Links ]
58. El-Ad B, lavie P. Effect of sleep apnea on cognition and mood. Int Rev Psychiatry. 2005;17(4):277-82. [ Links ]
59. Saunamaki T, Jehkonen M. Depression and anxiety in obstructive sleep apnea syndrome: a review. Acta neurol Scand. 2007;116(5):277-88. [ Links ]
60. Ong JC, Gress Jl, San Pedro-Salcedo MG, Manber R. frequency and predictors of obstructive sleep apnea among individuals with major depressive disorder and insomnia. J Psychosom Res. 2009;67(2):135-41. [ Links ]
61. Asghari A, Mohammadi f, Kamrava SK, tavakoli S, farhadi M. Severity of depression and anxiety in obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol. 2012. [ Links ]
62. McCall Wv, Harding D, ODonovan C. Correlates of depressive symptoms in patients with obstructive sleep apnea. J Clin Sleep Med. 2006;2(4):424-6. [ Links ]
63. Aloia MS, Arnedt Jt, Smith l, Skrekas J, Stanchina M, Millman RP. Examining the construct of depression in obstructive sleep apnea syndrome. Sleep Med. 2005;6(2):115-21. [ Links ]
64. Harris M, Glozier N, Ratnavadivel R, Grunstein RR. Obstructive sleep apnea and depression. Sleep Med Rev. 2009;13(6):437-44. [ Links ]
65. Peppard PE, Szklo-Coxe M, Hla KM, Young T. longitudinal association of sleep-related breathing disorder and depression. Arch Intern Med. 2006;166(16):1709-15. [ Links ]
66. Bardwell WA, Norman D, Ancoli-Israel S, Loredo JS, Lowery A, Lim W, Dimsdale JE. Effects of 2-week nocturnal oxygen supplementation and continuous positive airway pressure treatment on psychological symptoms in patients with obstructive sleep apnea: a randomized placebo-controlled study. behav Sleep Med. 2007;5(1):21-38. [ Links ]
67. Freedland KE, Carney RM, Hayano J, Steinmeyer BC, Reese Rl, Roest AM. Effect of obstructive sleep apnea on response to cognitive behavior therapy for depression after an acute myocardial infarction. J Psychosom Res. 2012;72(4):276-81. [ Links ]
68. Strohl KP. Obstructive sleep apnea syndrome. In: Pocota JS, Mitler MM, eds. Sleep Disorders: Diagnosis and treatment. Clifton: Humana; 1998:117-35. [ Links ]
69. Zimmerman ME, Aloia MS. Sleep-Disordered breathing and Cognition in Older Adults. Curr neurol neurosci Rep. 2012;12(5):537-46. [ Links ]
70. Macey PM, Woo MA, Kumar R, Cross Rl, Harper RM. Relationship between obstructive sleep apnea severity and sleep, depression and anxiety symptoms in newly-diagnosed patients. PloS One. 2010;5(4):e10211. [ Links ]
71. Zimmerman ME, Aloia MS. A review of neuroimaging in obstructive sleep apnea. J Clin Sleep Med. 2006;2(4):461-71. [ Links ]
72. Macey PM, Henderson LA, Macey KE, Alger JR, Frysinger RC, Woo MA, Harper RK, Yan-Go Fl, Harper RM. brain morphology associated with obstructive sleep apnea. Am J Respir Crit Care Med. 2002;166(10):1382-7. [ Links ]
73. Cross Rl, Kumar R, Macey PM, Doering Lv, Alger JR, Yan-Go Fl, Harper RM. Neural alterations and depressive symptoms in obstructive sleep apnea patients. Sleep. 2008;31(8):1103-9. [ Links ]
74. Mitler MM, Hayduk R. Benefits and risks of pharmacotherapy for narcolepsy. Drug Saf. 2002;25(11):791-809. [ Links ]
75. Loube DI, Gay PC, Strohl KP, Pack AI, White DP, Collop NA. Indications for positive airway pressure treatment of adult obstructive sleep apnea patients: a consensus statement. Chest. 1999;115(3):863-6. [ Links ]
76. McArdle N, Kingshott R, Engleman HM, Mackay TW, Douglas NJ. Partners of patients with sleep apnoea/hypopnoea syndrome: effect of CPAP treatment on sleep quality and quality of life. Thorax. 2001;56(7):513-8. [ Links ]
77. Pepperell JC, Ramdassingh-Dow S, Crosthwaite N, Mullins R, Jenkinson C, Stradling JR, Davies RJ. Ambulatory blood pressure after therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: a randomised parallel trial. lancet. 2002;359(9302):204-10. [ Links ]
78. Canessa N, Castronovo V, Cappa SF, Aloia MS, Marelli S, falini A, Alemanno F, ferini-Strambi L. Obstructive sleep apnea: brain structural changes and neurocognitive function before and after treatment. Am J Respir Crit Care Med. 2011;183(10):1419-26. [ Links ]
79.Habukawa M,Uchimura N,Kakuma T, Yamamoto K, Ogi K, Hiejima H,Tomimatsu K, Matsuyama S. Effect of CPAP treatment on residual depressive symptoms in patients with major depression and coexisting sleep apnea: Contribution of daytime sleepiness to residual depressive symptoms. Sleep Med. 2010;11(6):552-7. [ Links ]
80. Kawahara S, Akashiba T, Akahoshi T, Horie T. Nasal CPAP improves the quality of life and lessens the depressive symptoms in patients with obstructive sleep apnea syndrome. Intern Med. 2005;44(5):422-7. [ Links ]
81. Schwartz DJ, Kohler WC, Karatinos G. Symptoms of depression in individuals with obstructive sleep apnea may be amenable to treatment with continuous positive airway pressure. Chest. 2005;128(3):1304-9. [ Links ]
82. Engleman HM, Martin SE, Deary IJ, Douglas NJ. Effect of CPAP therapy on daytime function in patients with mild sleep apnoea/hypopnoea syndrome. Thorax. 1997;52(2):114-9. [ Links ]
83.Engleman HM, Martin SE, Deary IJ, Douglas NJ. Effect of continuous positive airway pressure treatment on day time function in sleepapnoea/hypopnoeasyndrome.Lancet.1994;343(8897):572-5. [ Links ]
84. Means MK, Lichstein Kl, Edinger JD, taylor DJ, Durrence HH, Husain AM, Aguillard Rn, Radtke RA. Changes in depressive symptoms after continuous positive airway pressure treatment for obstructive sleep apnea. Sleep breath. 2003;7(1):31-42. [ Links ]
85. McMahon JP, Foresman BH, Chisholm RC. The influence of CPAP on the neurobehavioral performance of patients with obstructive sleep apnea hypopnea syndrome: a systematic review. WMJ. 2003;102(1):36-43. [ Links ]
86. Schwartz DJ, Karatinos G. For individuals with obstructive sleep apnea, Institution of CPAP therapy is associated with an amelioration of symptoms of depression which is sustained long term. J Clin Sleep Med. 2007;3(6):631-5. [ Links ]
87. El-Sherbini AM, Bediwy AS, El-Mitwalli A. Association between obstructive sleep apnea (OSA) and depression and the effect of continuous positive airway pressure (CPAP) treatment. Neuropsychiatr Dis treat. 2011;7:715-21. [ Links ]
88. Yu bH, Ancoli-Israel S, Dimsdale JE. Effect of CPAP treatment on mood states in patients with sleep apnea. J Psychiatr Res. 1999;33(5):427-32. [ Links ]
89. Henke KG, Grady JJ, Kuna St. Effect of nasal continuous positive airway pressure on neuropsychological function in sleep apnea-hypopnea syndrome. A randomized, placebo-controlled trial. Am J Respir Crit Care Med. 2001;163(4):911-7. [ Links ]
90. Borak J, Cieslicki JK, Koziej M, Matuszewski A, Zielinski J. Effects of CPAP treatment on psychological status in patients with severe obstructive sleep apnoea. J Sleep Res. 1996;5(2):123-7. [ Links ]
91. Munoz A, Mayoralas LR, Barbe F, Pericas J, Agusti AG. Long-term effects of CPAP on daytime functioning in patients with sleep apnoea syndrome. Eur Respir J. 2000;15(4):676-81. [ Links ]
92. Kjelsberg Fn, Ruud EA, Stavem K. Predictors of symptoms of anxiety and depression in obstructive sleep apnea. Sleep Med. 2005;6(4):341-6. [ Links ]
93. Stepnowsky CJ, Jr., Moore PJ. Nasal CPAP treatment for obstructive sleep apnea: developing a new perspective on dosing strategies and compliance. J Psychosom Res. 2003;54(6):599-605. [ Links ]
94. Rosebush PI, MF MfM. Catatonia: Clinical features, Differential Diagnosis, and treatment. In: Jeste Dv, friedman JH, eds. Current Clinical neurology: Psychiatry for neurologists. totowa: Humana Press Inc; 2006:80-92. [ Links ]
95. Guilleminault C. Benzodiazepines, Breathing, and sleep. Am J Med. 1990;88(3A):25S-28S. [ Links ]
96. Kraiczi H, Hedner J, Dahlof P, Ejnell H, Carlson J. Effect of serotonin uptake inhibition on breathing during sleep and daytime symptoms in obstructive sleep apnea. Sleep. 1999;22(1):61-7. [ Links ]
97. Shatzberg Af. Mirtazapine.In: Shatzberg Af, nemeroff Cb, eds.The American Psychiatric Publishing text book of Psychopharmacology.4thed.Washington: American Psychiatric Publishing; 2009:429-37. [ Links ]
98. Kirkwood CK. Management of insomnia. J Am Pharm Assoc (Wash). 1999;39(5):688-696. [ Links ]
99. Lippmann S, Mazour I, Shahab H. Insomnia: therapeutic approach. South Med J. 2001;94(9):866-73. [ Links ]
100.Ballas CA, Evans Dl, Dinges Df. Psychostimulants and Wakefulness-Promoting Agents. In: Shatzberg Af, Nemeroff Cb, eds. American Psychiatric Publishing textbook of Psychopharmacology. 4th ed. Washington: American Psychiatric Publishing; 2009:843-60. [ Links ]
101. Robertson P, Jr., Hellriegel Et. Clinical pharmacokinetic profile of modafinil. Clin Pharmacokinet. 2003;42(2):123-37. [ Links ]
102. Pack AI, black JE, Schwartz JR, Matheson JK. Modafinil as adjunct therapy for daytime sleepiness in obstructive sleep apnea. Am J Respir Crit Care Med. 2001;164(9):1675-81. [ Links ]
103. Krystal AD, Harsh JR, Yang R, Rippon GA, Lankford DA. A double-blind, placebo-controlled study of armodafinil for excessive sleepiness in patients with treated obstructive sleep apnea and comorbid depression. J Clin Psychiatry. 2010;71(1):32-40. [ Links ]
104. Wise MG, Rundell JR. Anxiety and Insomnia. In: Wise MG, Rundell JR, eds. Clinical Manual of Psychosomatic Medicine: A Guide to Consultation-liaison Psychiatry: American Psychiatric Publishing; 2005:102-20. [ Links ]
105. Kribbs Nb, Pack AI, Kline LR, Getsy JE, Schuett JS, Henry Jn, Maislin G, Dinges Df. Effects of one night without nasal CPAP treatment on sleep and sleepiness in patients with obstructive sleep apnea. Am Rev Respir Dis. 1993;147(5):1162-8. [ Links ]
106. Espie CA. Insomnia: conceptual issues in the development, persistence, and treatment of sleep disorder in adults. Annu Rev Psychol. 2002;53:215-43. [ Links ]
Rui Lopes
Clinic of Psychiatry and Mental Health.
Centro Hospitalar de São João
Al. Prof. Hernâni monteiro 4200-319 porto
Email: rui.lopess@gmail.com














