INTRODUCTION
Allergic hypersensitivity to meat is rare, despite both its incidence and prevalence are not known with precision. Among patients with food allergies, allergy to meat has been reported in 3 to 15% of pediatric cases1 and 3% in adulthood2.
The main allergens in meat are serum albumins and immunoglobulins, both significantly altered by cooking, which may partially explain the low prevalence of meat allergy. The type of meat-causing allergy seems to be associated with its diet prevalence, thus geographical variations are evident 3. Cow´s beef allergy is the most frequently reported, and allergy to mammal meat is more prevalent than allergy to poultry meat and that of other birds 3.
Risk factors for the development of meat allergy have not been clearly defined, but there is growing evidence that, in susceptible individuals, multiple tick bites can result in sensitization to galactose-α-1,3-galactose (α-gal), an oligosaccharide abundantly expressed in nonprimate-mammal-tissues-and cells (red meat) but not in poultry (white meat). Therefore, patients sensitized to α-gal report late-onset symptoms after the consumption of a large variety of red meats (beef, pork, lamb, horse, venison, among others) and entrails such as liver or kidney 4.
Meat allergy caused by sensitization to α-gal has been reported in several parts of the world, including the United States of America (USA), Australia, Spain, Germany, Japan, and Sweden 5. α-gal is present in the gastrointestinal tract of at least one tick species and when a bite occurs, the tick´s gastric content is regurgitated onto the skin. Many patients report that meat allergic symptoms started after several tick bites, being plausible that α-gal would be the allergen responsible for primary sensitization. Tick species more frequently involved in meat allergy are Lxodes ricinus in Europe, Amblyomma americanum in the southwest of the USA, and other species (Lxodes holocyclus, Amblyomma cajennense, Amblyomma sculptum, and Haemophysalis longicornis) in the rest of the world 5.
Sensitization to α-gal can unchain crossed-reactions with cetuximab, gelatines of animal origin, vaccines, vaginal capsules, intravenous colloid serums, heparin, cardiac valves of bovine and swine origin, and eventually other hemostatic agents derived from animal products 6. Reactions to cetuximab, an anti-EGFR (epidermal growth factor receptor) monoclonal antibody, occur immediately upon first administration due to previous hypersensitivity to the α-gal epitope 6.
The diagnosis of red meat allergy related to α-gal involves a detailed clinical history and a full physical examination. As for any food allergy, an oral food challenge is the golden standard for diagnosis. The usefulness of prick tests in commercial extracts is limited due to their low sensitivity 7. Nevertheless, the measurement of α-gal specific serum immunoglobulin E (IgE) confirms the diagnosis and allows to monitor the evolution of the disease 6.
CASE DESCRIPTION
62-year-old male patient with a personal history of allergic rhinitis, nasal polyposis, and hypersensitivity to acetylsalicylic acid (ASA) - Widal syndrome, as well as coronary heart disease (with a positive cardiac stress test for myocardial ischemia), who works as a roadman in Madeira Island, Portugal.
The patient was referred to an Immunoallergology outpatient clinic for elective ASA desensitization due to the need for double platelet antiaggregant therapy after cardiac catheterization with coronary stent placement.
The patient undertook a desensitization protocol for 100mg of ASA with no occurrence of immediate or late-onset reactions and thus maintained the 100mg daily dose.
During the follow-up, the patient mentioned an “allergy to meat with fur” (sic), referring to reproducible episodes of urticaria, angioedema, and difficulty breathing, starting 3 hours after red meat ingestion. In the course of the latest episodes, these symptoms were also accompanied by lipothymia, which corresponds to a clinical presentation compatible with anaphylaxis. The physical examination did not present any relevant findings, except for the presence of exuberant hypertrophy of the lower nasal turbinates shown in the anterior rhinoscopy.
Since the last allergic reaction, the patient strictly avoids red meat and tolerates the ingestion of white meat.
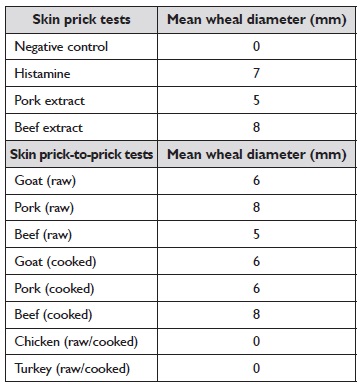
Skin prick tests were conducted, with positive results for pork and beef extracts. Skin prick-to-prick tests were also performed, with positive results for goat meat (raw and cooked), pork (raw and cooked), and beef (raw and cooked). Skin prick-to-prick tests for chicken and turkey meat were negative (Table 1).
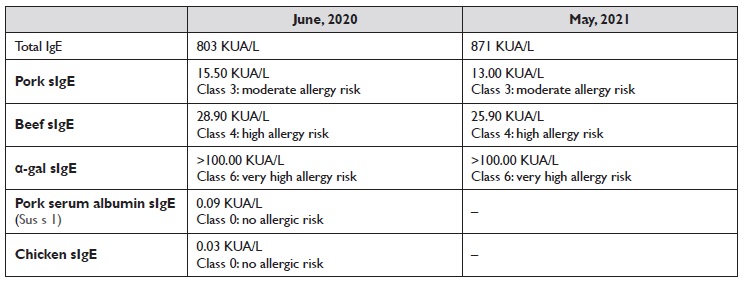
Standard tests for in vitro allergy diagnostics were carried out, specifically ImmunoCAP® (Thermo Fisher Scientific), for the quantitative measurement of total IgE and specific IgE in human serum via an ELISA-based fluoro immuno-enzymatic method. Total IgE level was 803.0 kU/L, and specific IgE was also augmented for pork (15.50 kU/L), beef (28.90 kU/L) and α-gal (>100.00 kU/L). Approximately one year after the initial assessment, all levels remained high. Specific IgE was negative for pork sérum albumin (0.09 kU/L) and chicken (0.03 kU/L) (Table 2).
The serologic study confirmed sensitization to red meat and excluded sensitization to white meat. During the diagnostic investigation, taking into account the previous history of anaphylaxis after meat ingestion, an oral food challenge was not performed.
It was recommended to the patient to avoid red meat and tick bites strictly. The patient was also instructed on how to auto-administrate adrenaline in case of acidental exposure and anaphylactic reactions.
DISCUSSION/CONCLUSION
Red meat allergy related to α-gal is rare and has only been described recently. This type of allergy presents several uncharacteristic traits, such as the trigger being an oligosaccharide instead of a protein and the fact that it is an IgE-mediated reaction with late-onset anaphylactic reactions.
Hypersensitivity reactions to α-gal have a significantly later onset, starting 3 to 6 hours after exposure, compared to typical IgE-mediated reactions 6. The late onset of symptoms seems to be related to the binding of α-gal to lipids, leading to slower intestinal absorption. Na in vitro model showed that the binding of α-gal to lipids facilitates the passage through intestinal epithelial cells, leading to the activation of basophils in patients with α-gal allergy, thus highlighting the importance of the basophil activation test (BAT) in this clinical entity 8.
The predominant symptom seems to be pruritus, but patients can also develop urticaria, angioedema, nausea, diarrhea, or even anaphylaxis 6. As usual in anaphylaxis, the organs involved include skin and mucosa (80-90% of cases), the respiratory system (70%), the gastrointestinal system (30-40%), the cardiovascular system (10-45%), and the central nervous system (10-15%) 9.
Patients frequently present a previous history of tick bites. Something important to highlight in this clinical case is the high probability of the patient being bitten multiple times due to his professional occupation, which could explain the initial sensitization to α-gal.
The treatment is based on avoiding the consumption of red meat and entrails of non-primate mammals 6. Tick bites should also be avoided by using repellents, appropriate clothing, and verification of ticks in clothing or the skin after outdoor activities or contact with animals. In respect to cetuximab, a desensitization protocol should be implemented if the patient has a therapeutic recommendation.
Furthermore, providing the patient with a detailed written emergency plan, including an adrenalina autoinjector, is crucial in case of accidental exposure. α-gal specific IgE levels tend to decrease if there is no new exposition to tick bites. The patients who avoid new tick bites can become once again tolerant to red meats.
The monitorization of α-gal specific IgE levels may predict the risk of a new allergic reaction. Unfortunately, up to date, neither skin prick tests, quantification of α-gal specific IgE, nor the ratio of specific IgE/total IgE allow the differentiation between patients presenting sensitization and patients who are clinically reactive.
There have been articles published reporting successful protocols for desensitization to α-gal, both in childhood and adulthood. Nevertheless, having into account the absence of new tick bites, the allergy to α-gal tends to dissipate over time 10. Therefore, it is unclear if the risk/benefit relationship related to desensitization is favourable when compared to the natural course of the disease.