Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Portuguese Journal of Nephrology & Hypertension
versão impressa ISSN 0872-0169
Port J Nephrol Hypert vol.26 no.4 Lisboa out. 2012
Isolated granulomatous interstitial nephritis and renal failure: an unusual presentation of sarcoidosis
Ana Farinha, José Assunção, Joana Felgueiras, José Vinhas
Department of Nephrology, Centro Hospitalar de Setúbal. Setúbal, Portugal.
ABSTRACT
Sarcoidosis is a multisystemic granulomatous disorder of unknown aetiology typically affecting the lungs and lymph nodes. Less frequently, the kidneys may also be affected. Postmortem analysis suggests that 20 percent of patients have histologic changes in the kidney. However, clinical involvement of the kidney is a relatively uncommon condition.
Renal failure may occur associated with hypercalcaemia, glomerular disease, or granulomatous interstitial nephritis. Renal failure associated with isolated granulomatous interstitial nephritis is an extremely rare entity, with only 57 cases reported until 1990, and the clinical presentation may be misleading.
We report a case of a 52-year-old man complaining of persistence of symptoms of lethargy and anorexia, admitted for hypercalcaemia and progressive renal failure. One year earlier, he presented to his primary care physician with a 3-month history of fatigue, anorexia and weight loss. At that time, laboratory findings showed renal failure with a raised serum creatinine of 2.8 mg/dL, and evidence of mesenteric lymphadenopathy on abdominal CT scan. However, as spontaneous regression of lymphadenopathy occurred, the clinical picture was attributed to a depression syndrome. During hospital stay, patient underwent a renal biopsy which showed a granulomatous interstitial nephritis with Schaumann bodies and led to a diagnosis of sarcoidosis. He was treated with steroids with disappearance of constitutional symptoms and partial recovery of renal function.
Renal sarcoidosis should be considered in the differential diagnosis of hypercalcaemia and renal failure. A raised serum angiotensin-converting enzyme may aid in making the diagnosis, but a renal biopsy is essential to confirm the diagnosis.
Timely diagnosis is critical to successful therapy, as the condition usually responds to early treatment with corticosteroids.
Key-Words:Chronic kidney disease; granulomatous interstitial nephritis; hypercalcaemia; sarcoidosis.
INTRODUCTION
Sarcoidosis is a multisystemic disorder characterized by an increased cellular immune response to an unknown antigen and the formation of noncaseating granulomas in affected tissues. Lungs and lymph nodes are the predominant sites affected (75 -90%) but other organs such as the eyes, skin, kidneys, liver and spleen may also be involved1. Postmortem analysis suggests that twenty percent of patients have histologic changes in the kidney2. Small published series of biopsy findings suggest that some degree of renal involvement occurs in approximately 35-50% of patients3-5. However, clinical renal involvement occurs in less than 5% of cases6 with most presenting as nephrocalcinosis or nephrolithiasis, but granulomatous interstitial nephritis, glomerular disease and obstructive uropathy may rarely occur7. Renal failure associated with granulomatous interstitial nephritis is an extremely uncommon manifestation.
We report a case of extra-pulmonary sarcoidosis presenting with renal failure and hypercalcaemia as initial manifestation, associated with granulomatous interstitial nephritis.
CASE REPORT
A 52-year-old white male was admitted for progressive renal failure in October 2010. Eighteen months earlier, he presented to his primary care physician with a three-month history of lethargy, anorexia, and weight loss (6kg, from 65 to 59kg).
At that time, he denied fever, sudoresis, and gastrointestinal, respiratory, cardiovascular, skin or urological symptoms. No family illnesses were reported. He worked as an electrician. He was a heavy smoker, having accrued a 35-pack-yr history of smoking. His physical examination was unremarkable. Significant laboratory findings showed renal failure with a raised serum creatinine of 2.8 mg/dL and urea of 88mg/dL, and abnormal liver function tests with a mildly elevated aspartate aminotransferase (AST 53U/L), alanine aminotransferase (ALT 81U/L) and gamma glutamyltransferase (GGT 96U/L). Chest X-ray was normal.
An abdominal ultrasound showed enlarged mesenteric lymph nodes, and the liver and spleen were normal. Renal ultrasound was unremarkable. An abdominal CT scan showed enlarged mesenteric lymph nodes. He underwent an upper gastrointestinal endoscopy which was unremarkable. As there was a spontaneous regression of mesenteric lymphadenopathy, he was diagnosed with a depression syndrome and medicated with Alprazolam 0,5mg id, Zolpidem 10mg id, Escitalopram 10mg id, Pentoxifylline 400mg id, Omeprazol 20mg id and vitamins.
In October 2010 he presented to his primary care physician complaining of persistence of symptoms of lethargy and anorexia, although his weight had been stable over the last eighteen months. Significant laboratory findings revealed deterioration of renal function with creatinine of 5.8 mg/dL. He was referred to our nephrology outpatient clinic and immediately admitted. His physical examination was unremarkable apart from his slim aspect. His blood pressure was 143-68 mm Hg.
Laboratory findings revealed anaemia, with haemoglobin 108 g/L (10.8 g/dL), impaired renal function with elevated serum creatinine and urea (5.8mg/dL and 132 mg/dL, respectively) and low eGFR (12.9ml/min/1.73 m2) and elevated serum calcium (12.9 mg/dL). Serum iPTH (12pg/mL) and 25(OH)D3 (19.8 ng/mL) were within the normal range. Urinalysis showed no proteinuria and normal sediment. The 24-hours urine volume was 2800ml and calciuria was 263mg (normal range: 100-250mg) with no other changes.
Serum protein electrophoresis was normal. Bence Jones protein was negative. There were no monoclonal protein bands by immunofixation electrophoresis in the urine. Serum complement levels were within the normal range. Serologies for ANCA, ANA, anti-DNA antibody levels, HIV and hepatitis B and C were unremarkable. Prostate-Specific Antigen (PSA) test was within the normal range (0.56 ng/mL). Serum angiotensin -converting enzyme (ACE) was raised at 91.2 U/L (normal range: 8-52 U/L). A renal ultrasound was normal. A chest CT scan showed the presence of bronchiectasis in the upper lobes. An abdominal and pelvic CT scan were unremarkable.
A bronchoscopy was normal. A bronchoalveolar lavage (BAL) showed no M. tuberculosis, and a ratio CD4:CD8 of 2.8 (normal range: <3.5).
He underwent a renal biopsy that revealed interstitial fibrosis with lymphocytic infiltrate, two noncaseous interstitial granulomas with epithelioid and giant cells containing characteristic Schaumann and asteroid bodies, with no significant glomerular or vascular lesions. Immunofluorescence study was negative. The biopsy was negative for mycobacterium and fungus.
He was initially treated with prednisone 1 mg/kg/day, with gradual dose tapering over subsequent months, with clinical improvement (increased 10kg over a six-month period), partial recovery of renal function (creatinine 2.4 mg/dL), and normalization of serum calcium levels (9.8mg/dL). Currently, he is taking 5 mg/day of prednisone, and laboratory findings show a serum creatinine of 2.5 mg/dL, and a proteinuria of 1.0 g/day.
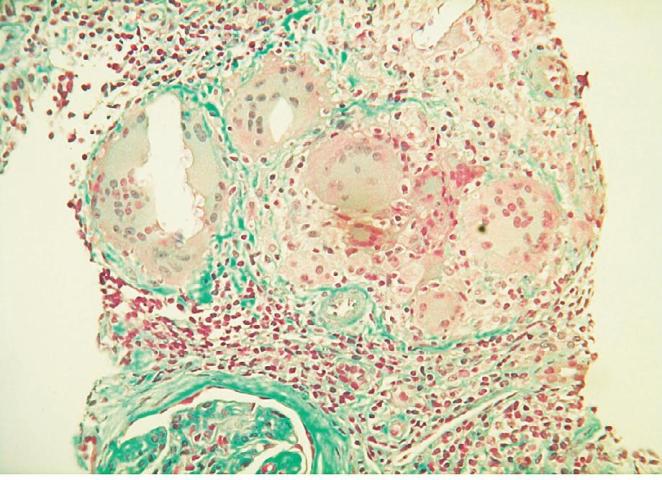
Figure 1
Langhans cells with oxalate calcium crystals, designated as Schaumann bodies (Trichrome staining x400)
DISCUSSION
The clinical presentation of sarcoidosis depends on the site and extent of organ involvement, duration of illness and activity of the disease. The usual modes of presentation include non-specific constitutional symptoms or symptoms related to organ-specific involvement8, with little or no abnormal findings in routine tests. The most common extra-pulmonary manifestations include lymphadenopathy, hepatomegaly and splenic enlargement.
Acute sarcoidosis is more common in whites than in blacks and usually is associated with spontaneous remission within two years. Abnormal calcium metabolism resulting in hypercalcaemia and/or hypercalciuria is often present in sarcoidosis, associated with increased absorption of dietary calcium9. Extrarenal synthesis of calcitriol [1,25(OH)2D3] is central to the pathogenesis of abnormal calcium homeostasis9,10. An elevated ACE level may provide additional diagnostic information although it lacks specificity. ACE levels are usually followed as a marker of disease activity rather than for diagnostic purposes.
In our patient, constitutional symptoms and evidence of mesenteric lymphadenopathy on abdominal CT scan prompted the diagnosis of lymphoma eighteen months earlier. Although lymphoma and metastatic disease are far more common causes of extensive abdominal lymphadenopathy, sarcoidosis should be considered. In this case, spontaneous regression of lymphadenopathy excluded the diagnosis of cancer.
This patient showed pulmonary bullous changes on chest CT scan. Bronchoscopy was unremarkable, and therefore a bronchial biopsy was not performed.
These changes have been attributed to the smoking history, although there were no previous symptoms of pulmonary disease. However, sarcoidosis has been reported to lead to bullous lung disease11. The condition was first reported in 1949 by Zimmerman and Mann12, and 17 additional case reports of bullous sarcoidosis have been reported since then11. In this case, the absence of a bronchial biopsy precludes the confirmation of the diagnosis of bullous sarcoidosis. In cases of pulmonary sarcoidosis, BAL fluid generally shows a predominance of CD4+ T cells and results in an elevated CD4+ to CD8+ ratio (>3.5)13. However, the diagnostic value of this ratio has been debated because of the high variability in sarcoidosis14,15. In this case the CD4+ to CD8+ ratio was within normal range.
We report a case of a predominantly extrapulmonary form of sarcoidosis, which had gone unrecognized for over a year. The patient presented with constitutional symptoms, elevated serum calcium and significant deterioration of renal function, and renal biopsy showed granulomatous interstitial nephritis, with Schaumann bodies, highly favouring the diagnosis of sarcoidosis. Renal failure associated with isolated granulomatous interstitial nephritis is an extremely uncommon manifestation of sarcoidosis.
Sarcoidosis should be considered in differential diagnosis of hypercalcaemia and renal failure, as it may reverse with prompt corticotherapy. Long-term therapy is often required to maintain normocalcaemia and renal function.
References
1. Rizzato G. Extrapulmonar presentation of sarcoidosis. Curr Opin Pulm Med 2001;7:295-297 [ Links ]
2. A study of sarcoidosis; based on a combined investigation of 160 cases including 30 autopsies from the Johns Hopkins Hospital and Massachusetts General Hospital. Cited on UpToDate (www.uptodate.com) [ Links ]
3. Lofgren, S, Snellman, B, Lindgren, AH. Renal complications in sarcoidosis; functional and biopsy studies. Acta Med Scand 1957;159:295-305 [ Links ]
4. Lebacq E, Desmet V, Verhaegen H. Renal involvement in sarcoidosis. Postgrad Med J 1970;46:526-529 [ Links ]
5. MacSearraigh ET, Doyle CT, Twomey M, OSullivan DJ. Sarcoidosis with renal involvement. Postgrad Med J 1978;54:528-532 [ Links ]
6. Baughman RP, Teirstein AS, Judson MA, et al. Clinical characteristics of patients in case control study of sarcoidosis. Am J Respir Crit Care Med 2001;164:1885-1889 [ Links ]
7. Casella FJ, Allon M. The kidney in sarcoidosis. J Am Soc Nephrol 1993;3:1555-1562 [ Links ]
8. Sharma OP. Fatigue and sarcoidosis. Eur Respir J 1999;13:713-722 [ Links ]
9. Muther RS, Mccarron DA, Bennett WM. Renal manifestations of sarcoidosis. Arch Intern Med 1981;141:643-645 [ Links ]
10. Inui N, Murayama A, Sasaki S, et al. Correlation between 25-hydroxyvitamin D3 1 alpha -hydroxylase gene expression in alveolar macrophages and the activity of sarcoidosis. Am J Med 2001;110:687-693 [ Links ]
11. Jeebun V, Forest IA. Sarcoidosis: an under -recognised cause for bullous lung disease. Eur Respir J 2009;34:999-1001 [ Links ]
12. Zimmerman, I, Mann, N. Boecks sarcoid: a case of sarcoidosis complicated by pulmonary emphysema and cor pulmonale. Ann Intern Med; 1949;31:153-162 [ Links ]
13. Göbel U, Kettritz R, Schmeider W, Luft FC. The protean face of renal sarcoidosis. J Am Soc Nephrol 2001;12:616-623 [ Links ]
14. Drent M, Mansour K, Linssen C. Bronchoalveolar lavage in sarcoidosis. Semin Respir Crit Care 2007;28:486-495 [ Links ]
15. Danila E, Jurgauskiene, Norkuniene J, Malickaite R. BAL fluid cells in newly diagnosed pulmonary sarcoidosis with different clinical activity. Ups J Med Sci 2009;114:26-31
Dr Ana Farinha
Department of Nephrology
Centro Hospitalar de Setúbal
Rua Camilo Castelo Branco
2910 Setúbal, Portugal
E-mail: alpfarinha@yahoo.com.br
Conflict of interest. None declared.
Received for publication: 10/06/2012
Accepted in revised form: 12/09/2012














