Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Portuguese Journal of Nephrology & Hypertension
versão impressa ISSN 0872-0169
Port J Nephrol Hypert vol.28 no.4 Lisboa dez. 2014
CASE REPORT
MPO-ANCA-positive crescentic glomerulonephritis superimposed on a mesangial proliferative glomerulonephritis in a patient with mixed cryoglobulinemia due to hepatitis C infection: a case report
Glomerulonefrite crescêntica ANCA-MPO positiva sobreposta em glomerulonefrite mesangioproliferativa num doente com crioglobulinémia mista secundária a infecção por hepatite C: um caso clínico
Luís Rodrigues1, Brigite Aguiar1, Marta Neves1, Tânia Santos1, Telma Santos1, Jose Gago1, Helena Sá1, Mário Campos1, Carol Marinho2
1Department of Nephrology – Centro Hospitalar e Universitário de Coimbra.Coimbra, Portugal.
2Department of Histopathology – Centro Hospitalar e Universitário de Coimbra.Coimbra, Portugal.
ABSTRACT
Renal involvement of antineutrophil cytoplasmic antibodies (ANCA) associated vasculitis typically occurs in the form of a pauci-immune crescentic glomerulonephritis. The finding of some immune complex deposits in these glomerulonephritis is not unusual, but the cases with greater than mild deposition suggest the presence of a second and immune complex related glomerular disease. The significance of the immune complex deposits and their role in ANCA associated vasculitis is still a topic of debate, but higher levels of proteinuria and worse prognosis with respect to renal function have been described in these patients.
We report a case of a patient with a known mesangial proliferative glomerulonephritis related to a mixed cryoglobulinemia secondary to a chronic hepatitis C infection that later developed a rapidly progressive glomerulonephritis due to a superimposed anti-myeloperoxidase ANCA positive glomerulonephritis.
Key-words: ANCA-associated vasculitis; immune complex deposits; mesangial proliferative glomerulonephritis; rapidly progressive glomerulonephritis.
RESUMO
O atingimento renal nas vasculites associadas aos anticorpos anticitoplasma de neutrófilo (ANCA) traduz-se, tipicamente, por uma glomerulonefrite crescentica pauci-imune. O achado de alguns depósitos de imunocomplexos nestas glomerulonefrites nao e incomum, mas os casos em que esta deposição e mais acentuada, sugerem a presença de uma segunda doença glomerular mediada por imunocomplexos. O significado dos depósitos de imunocomplexos e o seu papel nas vasculites associadas a ANCA e ainda um tema de debate, contudo, nestes doentes foram descritos niveis superiores de proteinuria e um pior prognostico em relação a preservação da função renal. Descrevemos o caso clinico de um doente com uma glomerulonefrite mesangioproliferativa em relação com uma crioglobulinemia mista secundaria a uma infeção cronica pelo vírus da hepatite C, que desenvolve posteriormente uma glomerulonefrite rapidamente progressiva associada a vasculite com ANCA anti-mieloperoxidase positivo.Palavras chave: Depósito de imunocomplexos; glomerulonefrite mesangioproliferativa; glomerulonefrite rapidamente progressiva; vasculite ANCA-associada.
INTRODUCTION
Antineutrophil cytoplasmic antibodies (ANCA) associated vasculitis have similar characteristics on renal histology and usually present as a pauciimmune crescentic glomerulonephritis (GN)1. The finding of some immune complex (IC) deposits in these GN is not unusual, and the majority are typically mild (≤ 2+on a 0 to 4+ scale)2,3. The cases of ANCA-associated GN with greater than mild IC deposition suggest the presence of a second and IC-related glomerular disease. IgA nephropathy, post-infectious GN, lupus nephritis, hepatitis C virus (HCV) associated glomerulopathy and membranous nephropathy have already been described in situations with a superimposed ANCA GN3-8. The significance of the IC deposits and their role in ANCA associated vasculitis is still a topic of debate.
We report the case of a patient presenting with a rapidly progressive (RPGN) MPO-ANCA-positive GN superimposed on a known mesangial proliferative GN related to a mixed cryoglobulinemia secondary to a chronic HCV infection.
CASE REPORT
A 35-year-old Caucasian man was admitted to our hospitals emergency room due to marked asthenia and polyarthralgias of inflammatory rhythm affecting the shoulders, elbows, wrists, metacarpophalangeal and proximal interphalangeal joints, knees and ankles with a few weeks of evolution. The patient also complained of diminished urinary output and slight oedema of his lower limbs. He had a known history of chronic HCV infection, type III mixed cryoglobulinaemia, hypertension (known for ten years) and additive symmetric polyarthritis (known for 2 years) being treated by a rheumatologist with 500 mg of naproxen and 5 mg of prednisone daily. During the initial investigation of this polyarthritis, an active urinary sediment was found with microscopic haematuria (437.99 erythrocytes/uL with dysmorphic features) and 24 hour proteinuria of 870 mg. By that time, additional laboratory results showed negative anti-nuclear antibodies, negative anti-double stranded DNA (anti-dsDNA), negative ANCA and normal C3 and C4. This led to the execution of a renal biopsy six months prior to his admission. Light microscopy (LM) showed 13 glomeruli with diffuse mesangial matrix expansion and hypercellularity. The interlobular arteries showed some intimal hyalinization and the interstitium was normal. The silver methenamine–stained section showed a normal glomerular basement membrane. Immunofluorescence (IF) microscopy contained ten glomeruli showing strong diffuse and segmental staining in the mesangium and less on the capillary walls of IgG (3+ on a 0 to 4+ scale), IgM (2+) and C3 (3+) and C1q (1+) staining.
The final histopathological diagnosis was a mesangial proliferative GN in the context of a type 3 mixed cryoglobulinaemia associated with a HCV infection.
The patient had also known significant alcoholic habits (heavy drinking, usual consumption of more than 15 units of alcohol per week) and a high tobacco exposure with 20 pack-years of smoking. Despite these addictions, he denied recent alcohol abuse or previous consumption of recreational drugs. He mentioned a car accident when he was 13 years old with a resultant exposed tibia fracture and the need for a blood transfusion (before 1992), the probable cause of his chronic HCV infection.
On admission, physical examination revealed a reasonable performance status, (karnofsky performance status scale of 80 %) with apparent age slightly superior to real age, a body mass index of 26.1 Kg/m2, and an elevated blood pressure (150/100 mmHg). A slight pain on active and passive movement of his shoulders and metacarpophalangeal joints was perceived, but with no signs of stiffness, tenderness, swelling or deformity of these or other affected joints. No purpura, petechiae, ecchymoses or other dermatologic signs were observed. His neurologic, cardiac, pulmonary and abdominal examinations were normal. He had a slight pitting oedema on both ankles and his urinary output in the first hours under observation was of 40 ml/h. Laboratory results at admission were as follows: haemoglobin 9.9 g/dL (normal range, 12.5-17.0 g/dL), mean corpuscular volume 92 fL (normal range, 80–100 fL), white blood cell count 5.9 x 109/L (normal range, 3.8-10.5 × 109/L), platelets 207 × 103 per mm3 (normal range, 150-300 103 per mm3), prothrombin time and partial thromboplastin time within the normal range, serum creatinine (SCr) 7.2 mg/dL (normal range, 0.72-1.18 mg/dL), blood urea nitrogen 110 mg/dL (normal range, 7.94-20.9 mg/dL), potassium 6.1 mmol/L (normal range, 3.5-5.1 mmol/L), albumin 3.8 g/dL (normal range, 3.5-5.2 g/dL), total cholesterol 177 mg/dL, HDL cholesterol 22 mg/dL, triglycerides 163 mg/dL, aspartate aminotransferase 23 U/L (normal range, < 38 U/L), alanine aminotransferase 18 (normal range, <41 U/L), alkaline phosphatase 62 U/L (normal range, 30-120 U/L), gamma-glutamyl transpeptidase 62 U/L (normal range, < 38 U/L) and C-reactive protein 2.39 mg/dL (normal range, < 0.05 mg/dL). The urinary sediment analysis showed 12.8 leucocytes/uL and 547 erythrocytes/uL with dysmorphic features. The spot urine protein-to-creatinine ratio was 2190 mg/g. A renal ultrasound was performed revealing normal sized kidneys with good corticomedullary differentiation and increased parenchymal echogenicity. His chest radiography was normal. There was deemed no need for emergency haemodialysis. He was admitted to our nephrology department with the diagnosis of a non-oliguric severe acute kidney injury and further investigation ensued. We obtained routine blood biochemistry from the patient, dated 3 months before this episode, that showed normal renal function and an active urinary sediment (9.5 leucocytes/uL and 79 erythrocytes/uL with dysmorphic features) and mild proteinuria (urine protein-to-creatinine ratio of 470 mg/g) with no other significant abnormalities. Additional diagnostic tests included: C3 1.45 g/L (normal range, 0.9-1.8 g/dL), C4 0.31 g/L (normal range, 0.1-0.4 g/dL), perinuclear ANCA (p-ANCA) strongly ositive (++++) with a myeloperoxidase (MPO) titer of > 600 U/ml. His anti-nuclear antibodies were slightly positive (+) with a diffuse granular pattern, the antidsDNA antibodies had a level of 3.9 IU/ml (normal range < 4.2 UI/ml) and the rheumatoid factor, anticyclic citrullinated peptide (CCP), anti-Smith (Anti-Sm), anti-Scl-70, anti-Ro/SS-A, anti-La/SS-B, and anti-GBM antibodies all were negative. The hepatitis C antibody (Anti-HCV) was positive but HCV-RNA was undetectable in the serum. The remaining viral screening for hepatitis B and the human immunodeficiency virus (HIV) 1 and 2 was negative. The known type III mixed cryoglobulinaemia was once again found (total concentration of polyclonal cryoprecipitate IgG, IgM and IgA: 0.028 g/L). The HCV-RNA in the cryoprecipitate was undetectable. The serum protein electrophoresis (SPEP) showed a slightly elevated level of the alpha-2 zone and no monoclonal spike. The immunoglobulin levels were normal and the serum and urinary immunofixation found no monoclonal protein.
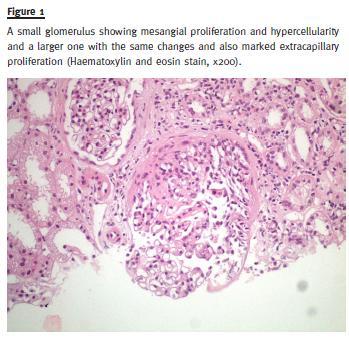
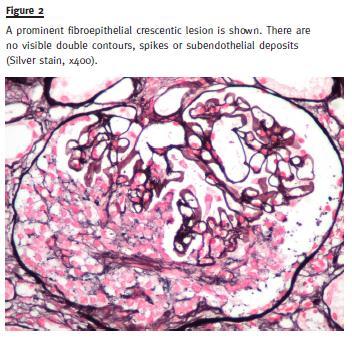
A second renal biopsy was performed and two fragments were collected for LM and IF. The LM showed a cortico-medullary fragment with sixteen glomeruli. Twelve glomeruli (75 %) showed extracapillary proliferation with fibroepithelial crescents (Fig. 1). A diffuse mesangial matrix expansion and hypercellularity was also present. The silver methenamine–stained section showed a normal glomerular basement membrane, with no double contours, spikes or subendothelial deposits (Fig. 2). Moderate chronic tubulointerstitial nephritis was present. The interlobular arteries showed lesions of atherosclerosis with intimal hyalinization and irregular narrowing of their lumen. The IF fragment contained ten glomeruli and revealed strong diffuse and segmental staining in the mesangium and capillary walls of IgG (3+), IgA (3+) and C3 (3+), with weaker IgM (1+) and C1q (1+) staining.
On the second day of admission, the patient started treatment for a crescentic GN with 3 pulses of 500 mg of methylprednisolone followed by 150 mg of oral cyclophosphamide (2 mg/Kg per day) and 80 mg of prednisone (1 mg/Kg/dia). Prophylaxis against opportunistic infections was used with daily 480 mg trimethoprim-sulfamethoxazole. During the following days, his renal function progressively improved and the sCr stabilized at 3.5 mg/dL. He was discharged on the tenth day with significant clinical improvement and good blood pressure control with an angiotensinconverting-enzyme (ACE) inhibitor. At this point, the urinary sediment showed signs of lesser activity (110 erythrocytes/uL), but significant proteinuria was still present (spot urine protein-to-creatinine ratio: 3910 mg/g). One month later, in a routine follow-up consultation, the patient had no complaints, showed stable renal function and a MPO titer of 85 U/ml.
Three months after discharge, the patient was diagnosed with pneumonia and severe leucopenia and readmitted to the nephrology department. Oropharyngeal candidiasis was present and reinforced the idea of a high immunosuppression state. A chest computed tomography scan (CT scan) showed consolidation areas in the posterior segment of the right superior lobe and on both lower lobes. Cyclophosphamide was stopped and the patient remained on 20 mg of prednisone. A multi-drug-resistant Pseudomonas aeruginosa was isolated from a bronchoalveolar lavage (BAL) and the patient was started on intravenous (IV) colistin, which he maintained for ten consecutive days. Renal function remained stable.
Twenty days after being discharged, he was admitted with a recurrence of the pneumonia. Severe respiratory insufficiency developed and orotracheal intubation was required for the institution of mechanical ventilation.
A new CT scan showed various areas of consolidation with cavities in both lungs. The biggest cavitation was found in the right superior lobe and was 7.8 cm in diameter. A multi-drug-resistant Pseudomonas aeruginosa was again isolated, this time from a sputum culture and a BAL. Blood cultures were negative.
After five days in an intensive care unit, he was again transferred to our department. Due to recurrent fever and other signs of treatment resistance, amikacin was associated with colistin for the approach of the isolated multi-drug-resistant Pseudomonas aeruginosa.
An upper gastro-intestinal endoscopy was performed due to epigastric pain and dyspepsia showing extensive esophageal candidiasis, which was treated with fluconazol. A multi-disciplinary approach to this clinical picture was used and an infectologist, a pneumologist and pulmonary surgeon were consulted. The hypothesis that the pulmonary disease was ANCA-associated was considered and two lung biopsies of the cavitations were performed: a transbronchial biopsy with flexible bronchoscopy and a second one with thoracoscopy.
Both showed unspecific inflammatory findings without signs of small vessel vasculitis or granulomatous inflammation in the surrounding tissues.
Despite his severe inflammatory state his renal function remained stable. The ANCA-MPO titer was repeated and a level of 25 U/ml was found. His clinical condition progressively deteriorated with multi-organ failure and the patient died six months after the diagnosis of RPGN was made.
DISCUSSION
Our patient presented a typical RPGN overlapping with a known mesangial proliferative GN. The RPGN is a syndrome currently categorised into one of four disorders, which reflect different mechanisms of glomerular injury: Anti-glomerular basement membrane (GBM) antibody disease (Type 1), immune complex deposition (Type 2), pauci-immune (Type 3) and double-antibody positive disease (Type 4), which has features of both types 1 and 39. Looking at the differential diagnosis of our case we would essentially have to consider either a type 3 RPGN with pauciimune ANCA associated vasculitis or a type 2 RPGN with a cryoglobulinemic associated vasculitis. The histological and laboratory findings suggest a MPOANCA-positive GN superimposed on a mesangial proliferative cryoglobulinemic GN. Renal involvement in type III mixed cryoglobulinemia is variable and usually non-specific, contrary to the type II mixed cryoglobulinemia, in which the IgMk monoclonal component is related to a specific well-characterised pattern of a glomerular disease, the membranoproliferative GN. [10-12] Our patient´s history of active urinary sediment and mild proteinuria together with his chronic complaints of arthralgias, especially those affecting the metacarpophalangeal, knees and ankles, are common manifestations of type III mixed cryoglobulinemia13.
We believe that the acute crescentic activity in this RPGN is in association with the ANCA.
The high ANCA-MPO titer associated with normocomplementemia at diagnosis and the simultaneous fall in the ANCA-MPO titer with treatment and clinical improvement favour this hypothesis. Chronic kidney insufficiency, significant proteinuria and microscopic haematuria ensued despite this improvement in renal function. This is in agreement with the trend towards a worse outcome with respect to renal function, higher serum creatinine levels at the time of biopsy, greater percentage of crescents and higher levels of proteinuria, as described by Neumann et al. and Haas et al. in their studies concerning IC deposits in ANCA-associated crescentic GN2,3. Pulmonary involvement is common in ANCA associated vasculitis and our CT scan findings with areas of consolidation and cavitations are, therefore, not an unusual type at presentation14,15. Despite this, we consider that the aggravated immunosuppression status of the patient and the persistent isolation of Pseudomonas aeruginosa manifestly point to a central infectious explanation for these radiologic findings.
The superimposition of the MPO-ANCA-positive crescentic GN on a mesangial proliferative GN may be coincidental or reflect a common pathophysiological process in both diseases. Some authors suggest an interaction between IC and ANCA in producing GN, especially in the beginning of the pathological process2,16-18. An animal model developed to produce ANCA GN and vasculitis showed that the process was not truly pauci-immune and that the IC played a role in its pathophysiology19. There is also experimental evidence suggesting that the alternative pathway of complement is involved in the pathogenesis of ANCAassociated glomerulonephritis and that its inhibition might be a potential therapeutic approach20-22.
Our case report illustrates a unique MPO-ANCApositive GN superimposed on a mesangial proliferative cryoglobulinemic GN with two renal biopsies performed at distinct times. Of interest is the absence of IgA deposition on the first biopsy and strongly positive on the IF of the second one, relating to the ANCA associated vasculitis. The RPGN with positive MPO ANCA associated IgA nephropathy was already described by other authors and the role of the IC deposition is still to be determined4,23. We hypothesize that a conjugation of factors took place in the pathophysiological subset of the ANCA GN of this patient, including a pre-existing pro-inflammatory environment, the glomerular IC deposition and a possible subsequent complement activation.
References
1. Jennette JC, Falk RJ, Bacon PA, et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum 2013;65(1):1-11. [ Links ]
2. Neumann I, Regele H, Kain R, Birck R, Meisl FT. Glomerular immune deposits are associated with increased proteinuria in patients with ANCA-associated crescentic nephritis. Nephrol Dial Transplant 2003;18(3):524-531. [ Links ]
3. Haas M, Eustace JA. Immune complex deposits in ANCA-associated crescentic glomerulonephritis: a study of 126 cases. Kidney Int 2004;65(6):2145-2152. [ Links ]
4. Haas M, Jafri J, Bartosh SM, Karp SL, Adler SG, Meehan SM. ANCA-associated crescentic glomerulonephritis with mesangial IgA deposits. Am J Kidney Dis 2000;36(4):709-718. [ Links ]
5. Haas M. Incidental healed postinfectious glomerulonephritis: a study of 1012 renal biopsy specimens examined by electron microscopy. Hum Pathol 2003;34(1):3-10. [ Links ]
6. Nasr SH, DAgati VD, Park HR, et al. Necrotizing and crescentic lupus nephritis with antineutrophil cytoplasmic antibody seropositivity. Clin J Am Soc Nephrol 2008;3(3):682-690. [ Links ]
7. Igaki N, Nakaji M, Moriguchi R, Akiyama H, Tamada F, Goto T. A case of hepatitis C virus-associated glomerulonephropathy presenting with MPO-ANCA-positive rapidly progressive glomerulonephritis. Nihon Jinzo Gakkai Shi 2000;42(4):353-358. [ Links ]
8. Tse WY, Howie AJ, Adu D, et al. Association of vasculitic glomerulonephritis with membranous nephropathy: a report of 10 cases. Nephrol Dial Transplant 1997;12(5):1017-1027. [ Links ]
9. Couser WG. Rapidly progressive glomerulonephritis: classification, pathogenetic mechanisms, and therapy. Am J Kidney Dis 1988;11(6):449-464. [ Links ]
10. Barsoum RS. Hepatitis C virus: from entry to renal injury–facts and potentials. Nephrol Dial Transplant 2007;22(7):1840–1848. [ Links ]
11. Roccatello D, Fornasieri A, Giachino O, et al. Multicenter study on hepatitis C virusrelated cryoglobulinemic glomerulonephritis. Am J Kidney Dis 2007;49(1):69-82. [ Links ]
12. Fabrizi F. Hepatitis C virus, cryoglobulinemia, and kidney: novel evidence. Scientifica (Cairo) 2012;2012:128382. [ Links ]
13. Monti G, Galli M, Invernizzi F, et al. Cryoglobulinaemias: a multi-centre study of the early clinical and laboratory manifestations of primary and secondary disease. GISC. Italian Group for the Study of Cryoglobulinaemias. QJM 1995;88(2):115-126. [ Links ]
14. Gomez-Puerta JA, Hernandez-Rodriguez J, Lopez-Soto A, Bosch X. Antineutrophil cytoplasmic antibody-associated vasculitides and respiratory disease. Chest 2009;136(4):1101-1111. [ Links ]
15. Specks U. Pulmonary vasculitis. In: Interstitial Lung Disease, 4th, King TE, Schwarz MI. BC Decker, 2003: 615.
16. Ardiles LG, Valderrama G, Moya P, Mezzano SA. Incidence and studies on antigenic specificities of antineutrophil-cytoplasmic autoantibodies (ANCA) in poststreptococcal glomerulonephritis. Clin Nephrol 1997;47(1):1-5. [ Links ]
17. Brouwer E, Huitema MG, Klok PA, et al. Antimyeloperoxidase-associated proliferative glomerulonephritis: an animal model. J Exp Med 1993;177(4):905-914. [ Links ]
18. Yang JJ, Jennette JC, Falk RJ. Immune complex glomerulonephritis is induced in rats immunized with heterologous myeloperoxidase. Clin Exp Immunol 1994;97(3):466-473. [ Links ]
19. Xiao H, Heeringa P, Hu P, et al. Antineutrophil cytoplasmic autoantibodies specific for myeloperoxidase cause glomerulonephritis and vasculitis in mice. J Clin Invest 2002;110(7):955-963. [ Links ]
20. Gou SJ, Yuan J, Wang C, Zhao MH, Chen M. Alternative complement pathway activation products in urine and kidneys of patients with ANCA-associated GN. Clin J Am Soc Nephrol 2013;8(11):1884-1891. [ Links ]
21. Kettritz R. With complements from ANCA mice. J Am Soc Nephrol 2014;25(2):207-209. [ Links ]
22. Van Timmeren MM, Chen M, Heeringa P. Review article: Pathogenic role of complement activation in anti-neutrophil cytoplasmic auto-antibody-associated vasculitis. Nephrology (Carlton) 2009;14(1):16-25. [ Links ]
23. Allmaras E, Nowack R, Andrassy K, Waldherr R, van der Woude F, Ritz E. Rapidly progressive IgA nephropathy with anti-myeloperoxidase antibodies benefits from immunosuppression. Clin Nephrol 1997;48(5):269-273. [ Links ]
Dr. Luis Miguel Amaral Rodrigues
Department of Nephrology – Centro Hospitalar e Universitario de
Coimbra Praceta Prof. Mota Pinto, 3000-075 Coimbra, Portugal.
E -mail: luis.arodrigues@hotmail.com
Conflict of interest statement: None declared.
Received for publication: 27/07/2014
Accepted in revised form: 13/08/2014














