Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Portuguese Journal of Nephrology & Hypertension
versão impressa ISSN 0872-0169
Port J Nephrol Hypert vol.29 no.2 Lisboa jun. 2015
CASE REPORT
Ultrasound-guided angioplasty, a suitable alternative in some patients
Angioplastia guiada por eco-doppler, uma alternativa adequada para alguns doentes
Maria Guedes Marques, Pedro Maia, Carlos Barreto, Telmo Carvalho, Pedro Ponce
Centro de Acessos Vasculares Nephrocare Lumiar, Lisboa, Portugal
ABSTRACT
Introduction and Objectives: Percutaneous transluminal angioplasty has been the central therapeutic modality used to treat dialysis vascular access (VA) dysfunction. The gold standard imaging modality is digital subtraction angiography. Some centers recently reported their technical success with ultrasound-guided angioplasty. Material and Methods: The authors report their first case experience with this modality. A 73 -year -old, diabetic male, on hemodialysis through a brachiocephalic fistula for 4 years, was referred to consultation due to increase of aneurisms, prolongation of haemostasis, recirculation increase and access blood flow (ABF) decrease > 25% from the baseline (1300 ml/min). Regarding the patients history, there was a mild degree of steal syndrome after the fistula surgery, which improved over time. Doppler ultrasound was successfully used to evaluate VA, characterize stenosis, and guide endovascular procedure. Results: Three haemodynamic significant stenosis were diagnosed; BF 650 ml/min; resistance index 0.62. The guidance of an eight mm diameter angioplasty balloon allowed a successful dilation of the stenoses. The first angioplasty was performed in the cephalic arch stenosis, which increased the ABF to 802 ml/min. Then, the middle stenosis was dilated with a post -procedure ABF of 930 ml/min. Finally, the post -aneurism stenosis was also dilated with a final result of 1195 ml/min, and clinical improvement without any sign of steal syndrome recurrence or procedure-related complications. Monitoring and surveillance after first trimester show a well-functioning fistula with stable flow rates. Conclusion: Doppler ultrasound has a key role in the VA surveillance, because it is the only exam that bases decisions on a morphologic and haemodynamic assessment. More than a diagnostic exam, ultrasound guidance may provide a valid and safe tool in the treatment of peripheral VA stenosis. Main advantages of this modality include lack of radiation and contrast; lower costs; and possible future procedures in the dialysis chair. Furthermore, patients with high risk of steal syndrome or heart failure would benefit from a controlled procedure with real time evaluation, not only based on their anatomy, but mainly on haemodynamic features.
Key-Words:Angioplasty; blood flow; Doppler ultrasound; stenosis vascular access.
RESUMO
Introdução e Objectivos: A angioplastia percutânea transluminal tem sido a modalidade central no tratamento do acesso vascular (AV) disfuncionante. A modalidade de imagem gold standard utilizada é a angiografia digital de subtracção. Alguns centros publicaram recentemente a sua experiência com a angioplastia guiada por eco-doppler. Material e Métodos: Os autores reportam a sua primeira experiência com a modalidade ecográfica. Um doente do sexo masculino, diabético, em programa de hemodiálise através de uma fistula braquiocefálica desde há 4 anos, foi referenciado à consulta por aumento de aneurisma, hemostase prolongada, aumento da recirculação e redução do débito do acesso (Qa) > 25% ao seu valor de base (1300 ml/min). De salientar antecedente de síndrome de roubo ligeiro, após a construção de fistula, que melhorou com o tempo. O eco–doppler foi utilizado com sucesso para avaliação inicial do acesso, caracterização das estenoses e orientação do procedimento endovascular. Resultados: Foram identificadas 3 estenoses hemodinamicamente significativas; Qa 650 ml/min; índice resistência 0.62. A selecção de um balão de 8 mm de diâmetro permitiu uma dilatação adequada das estenoses. O Qa foi avaliado em tempo real, após cada uma das dilatações, para prevenir a sobrecorrecçao. A primeira angioplastia foi realizada na estenose da crossa cefálica, o que aumentou o Qa para 802 ml/min. A dilatação da estenose do terço médio originou um Qa de 930 ml/min. Finalmente, a dilatação da estenose pós-aneurisma resultou num último Qa de 1195 ml/min, com melhoria clínica, e sem recorrência do S. roubo ou qualquer complicação associada ao procedimento. Monitorizaçao após o primeiro trimestre revelou uma fistula funcionante com débitos estáveis. Conclusão: O eco -doppler tem um papel fundamental na monitorizaçao do AV, porque é o único exame cuja decisão se baseia numa avaliação morfológica e hemodinâmica. Mais do que diagnóstica, a ecografia pode ser uma ferramenta útil e segura no tratamento das estenoses periféricas. As suas principais vantagens incluem a ausência de radiação e contraste; menores custos; e possibilidade futura de realizar procedimentos na sala de diálise. Além do mais, doentes com elevado risco de S. roubo e insuficiência cardíaca poderão beneficiar de um procedimento controlado através de uma avaliação em tempo real, não apenas baseada em critérios anatómicos, mas sobretudo hemodinâmicos.
Palavras-Chave: Acesso vascular; angioplastia; débito do acesso; eco-doppler; estenose.
INTRODUCTION
Properly functioning of vascular access (VA) is mandatory for haemodialysis. Unfortunately, VA function is often disrupted. Aetiology for VA dysfunction is mainly attributed to the development of neointimal hyperplasia that determines flow limiting stenosis1.
Percutaneous transluminal angioplasty (PTA) has been the central therapeutic modality used for treatment, and the gold standard imaging modality for performing it is fluoroscopy and digital subtraction angiography2,3.
In the recent years some authors published their experience on the use of ultrasonog raphy as a reliable method of imaging dur ing intravascular procedures4-7.
CASE REPORT
The authors report their first case experience with ultrasound guided angioplasty modality. A 73-year-old, diabetic male with end -stage kidney disease on haemodialysis for 5 years, and a brachiocephalic fistula for 4, was referred to the vascular access centre due to increase of an aneurisms size and tension, prolongation of haemostasis time, increase of recirculation and access blood flow (ABF) decrease of 40% from the baseline (1300 ml/min to 650 ml/min). Regarding the patients history, it should be highlighted a moderate degree of steal syndrome after the fistula creation, which improved over time. Physical examination revealed presence of thrill in the anastomosis and initial vein, which was pulsatile, especially in the aneurism segment, with lack of collapse with arm elevation.
There were no collaterals or oedema. Doppler ultrasound (DU) was first used to evaluate the VA, identify stenosis, and characterize them according to morphologic and haemodynamic criteria. Anastomosis was normal, with a moderately elevated diameter of 5.4 mm. Immediately after the anastomosis a first venous segment with 3.2 – 4.0 mm was seen, but without significant elevation of the velocities. After this segment, an aneurism was measured with 32.3 mm (Figs.1 and 2). Three venous stenoses were diagnosed with haemodynamic significance (Fig. 2). The first with post -anastomosis location, immediately after the aneurism, with a diameter of 3.2 mm (> 50% reduction); maximum systolic peak velocity (SPV) of 380 cm/s and a stenosis/pre -stenosis SPV ratio > 2.5 (Figs. 2 and 3).
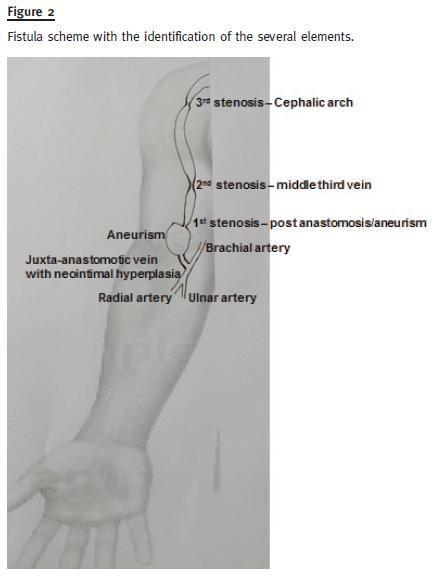
The second stenosis located in the middle third of the vein was characterized by a diameter of 2.0 mm (> 50% reduction); maximum SPV of 420 cm/s and a SPV ratio > 2.5 (Figure 2 and 4). The third stenosis was in the cephalic arch, had a diameter of 2.5 mm (> 50% reduction), maximum SPV of 400 cm/s and SPV ratio > 2.5 (Figs. 2 and 5). The brachial artery had no relevant morphologic abnormalities beside a mild calcification of the wall. Brachial BF was 650 ml/min and resistance index (RI) in the same artery was 0.62 (Fig. 6).
Because we are in an early phase, fluoroscopic guidance was initially used to bailout central stenosis and finally to confirm anatomical results, however, the procedure was done completely under ultrasound guidance.
The guidance of the placement of an 8.0 mm diameter angioplasty balloon allowed a successfully dilation of the stenoses (Fig. 5). To prevent overcorrection and steal syndrome recurrence, BF was evaluated immediately after each dilation. The first angioplasty was performed in the cephalic arch stenosis that increased the ABF to 802 ml/min. Then, the middle stenosis was Finally, the post -aneurism stenosis was dilated with a final result of 1195 ml/min, (Fig. 6) and clinical improvement of the aneurism tension without any sign of steal syndrome or any complications related to the procedure.
After the procedure, the final angiography performed to exclude complications showed a mild residual stenosis in the second location (middle third).
Benefits and risks of a higher ABF were weighted taking into account the clinical improvement and the baseline ABF of 1300 ml/min when the patient had steal symptoms. The final decision was to finish the procedure without more aggressive approaches. The three-month clinical follow-up and surveillance show a well -functioning fistula with stable flow rates.
DISCUSSION
The KDOQI guidelines state that any stenosis > 50% in relation to a normal appearing adjacent venous segment in conjunction with clinical or physiological symptoms be treated with PTA or surgical revision1. As stated above, since the eighties, angiography has been the standard of care in maintaining luminal patency by treating venous stenosis2,3.
Some of the drawbacks of this modality are the exposure of patient and personnel to ionizing radiation; exposure to iodinated contrast agents; and high costs associated with fluoroscopic imaging hardware; as well as additional technicians requirement8-12.
At first, the use of ultrasonography allows for the initial evaluation and identification of the cause of dysfunction. It eliminates unnecessary angiographies when a stenosis is not the main cause of dysfunction18,19 or does not have the haemodynamic criteria recommended to demand an endovascular dilation20.
For example, regarding our patient, the post-anastomotic segment was not touched because its measures did not meet the criteria for a haemodynamically significant stenosis. This is defined by a diameter reduction of the lumen vessel > 50%; ABF < 600 ml/minute, or a decrease > 25% from previous measurements; and a maximum stenosis PSV > 400 cm/s associated with a > two -fold increase of PSV (ratio > 2)20. In practice, this significant change in velocities can be first seen in the ultrasound colour mode, with the aliasing phenomenon (high velocities correspond to yellow and green colours) and then confirmed in the doppler mode, that objectively measures the velocity. Adding to this, some authors, like Malik21, have established additional criteria to distinguish true stenosis (that compromises ABF and raises the risk of thrombosis) from borderline stenosis (that does not compromise significantly VA function, and where an angioplasty may not be beneficial because it increases restenosis mechanisms). An absolute vessel diameter < 2.0 mm is one of the most encouraged. Moreover, post–anastomosis venous segment stenosis is mostly defined by neointimal hyperplasia related to the shear stress, which is more likely to restenosis, so angioplasty indications should be carefully selected.
Adding to this powerful role in surveillance and diagnosis of true ABF limiting stenosis, some published reports demonstrated very good results of ultra sound- guided angioplasty. Effectiveness ranged between 92% and 97% depending on indications and location of the lesion13,14. Due to this evidence, advances in ultrasonography have provided an alternative tool to offer patient specific treatment according to several VA criteria (morphologic and haemodynamic), as well as the patients clinical condition.
Because ultrasound has major limitations in visualizing the central venous system, this type of guidance is indicated when the dialysis fistula stenosis is located periph erally to the clavicle15. However, application of ultrasound imaging during endovascular procedures on the the subclavi an vein and brachiocephalic trunk has also been described7.
Another advantage of this modality is the lack of radiation exposure for both patients and healthcare professionals. Patients that could also benefit from this technique are the ones allergic to iodinated contrast agents, in the pre-dialysis period, and in those with good residual renal function5,16,17.
Toward the procedure itself, the heavy hardware used for fluoroscopy, as well as the radiology technicians, can be substituted for a portable device that allows possible future development of performing the procedures in the dialysis chair at a lower cost15.
It allows an accurate characterization of the stenosis for the exact choice of balloon size according to the diameter of the vessel. Proper choice of puncture site is one of the most impor tant elements that determine the success of the procedure. Small distance between fistula puncture site and the stric ture may cause significant difficulty during intravascular intervention.
Adding to this, the puncture of an immature fistula can be difficult and increases the risk of thrombosis due to damage of an insufficiently thickened vessel wall and greater pro pensity to haematoma formation22. In this setting, ultrasound guides a precise and ideal puncture site, making it easier to conduct the procedure, avoiding complications and minimizing waste of material. After the angioplasty, the result can be immediately assessed through measuring BF changes, in addition to the luminal diameter improvement. Complications such as rupture, thrombosis or spasm may also be ruled out and managed with this technique23.
Patients with diabetes, high risk of steal syndrome and heart disease, have increased risk of cardiovascular complications related to haemodynamic outcome and may benefit from a procedure which is haemodynamically controlled in real time, being future candidates to this modality. In a practical way, until now, a successful angioplasty has been defined as residual stenosis < 30% with acceptable resolution of clinical parameters1. However, according to several studies, the degree of stenosis evaluated through angiography is not associated with patency outcomes.
This result is probably due to the fact that the conventional definition of stenosis expressed as a percentage is inaccurate in the venous circuit because the adjacent vein may be small, dilated after stenosis, or aneurysmal. Large differences in the degree of stenosis can be calculated depending on which venous segment is used as a reference point24. On the other hand, recommendations to avoid complications due to overcorrection in selected patients have not been established. In this setting, the ultrasound evaluation allows a haemodynamic and objective evaluation that could overcome subjectivity respecting both over - and under-treatment25.
It is true that ultrasonography evaluation is operator-dependent, however, like in many techniques, a careful personnel training enables reliable professionals with good skills. In the current time, there is no published experience regarding any critical target limits for ABF to prevent overcorrection and steal syndrome recurrence or other related complications.
To the best of our knowledge, this value may vary mainly according to VA location and to the arterial territory distally to the anastomosis, among other factors. In this case, the baseline value was a useful reference value. Long-term follow-up and future trials will clarify about these approaches.
CONCLUSION
Doppler ultrasound has a key role in the vascular access surveillance, because it is the only exam that bases decisions on a complete assessment (morphologic and haemodynamic). Additionally, ultrasound guidance may provide a valid and safe tool in locating and treating peripheral VA stenosis. We share our first case experience, not to show it as a substitute technique of digital subtraction angiography but as a suitable alternative for patients with contrast allergy, pre-dialysis with good residual renal function in which contrast avoidance is crucial. Furthermore, patients with high risk of steal syndrome and severe heart failure may benefit from a controlled procedure with real time anatomical and haemodynamic evaluation to avoid some complications related to higher blood flows.
References
1. Navuluri R, Regalado S. The KDOQI 2006 Vascular access update and fistula first program synopsis. Semin Intervent Rad 2009; 26(2): 122-124. [ Links ]
2. Glanz S, Bashist B, Gordon DH, Butt K, Adamsons R. Angiography of upper extremity access fistulas for dialysis. Radiology 1982; 143(1): 45-52. [ Links ]
3. Gordon DH, Glanz S, Butt KM, Adamsons RJ, Koenig MA. Treatment of stenotic lesions in dialysis access fistulas and shunts by transluminal angioplasty. Radiology 1982; 143(1): 53-58. [ Links ]
4. Marks N, Ascher E, Hingorani AP. Duplex -guided repair of failing or nonmaturing arterio -venous access for hemodialysis. Perspect Vasc Surg Endovasc Ther 2007; 19(1): 50-55. [ Links ]
5. Ascher E, Hingorani A, Marks N. Duplex -guided balloon angioplasty of failing or nonmaturing arterio -venous fistulae for hemodialysis: a new office -based procedure. J Vasc Surg 2009; 50(3): 594-599. [ Links ]
6. Fox D, Amador F, Clarke D, et al. Duplex guided dialysis access interventions can be performed safely in the office setting: techniques and early results. Eur J Vasc Endo Vasc 2011; 42(6): 833-841. [ Links ]
7. Wakabayashi M, Hanada S, Nakano H, Wakabayashi T. Ultrasound -guided endovascular treatment for vascular access malfunction: results in 4896 cases. J Vasc Access 2013; 14(3): 225-230. [ Links ]
8. Weisbord SD, Palevsky PM. Radiocontrast -induced acute renal failure. J Intensive Care Med 2005; 20(2):63-75. [ Links ]
9. Ramaswami G, al-Kutoubi A, Nicolaides AN, Dhanjil S, Griffin M, Ryan MF. Peripheral transluminal angioplasty under ultrasound guidance: initial clinical experience andprevalence of lower limb lesions amenable to ultrasound -guided angioplasty. J Endovasc Surg 1995; 2(1):27-35. [ Links ]
10. Lipsitz EC, Veith FJ, Ohki T, et al. Does the endovascular repair of aortoiliac aneurysms pose a radiation safety hazard to vascular surgeons? J Vasc Surg 2000; 32(4):704-710. [ Links ]
11. Ascher EA, Hingorani AP, Marks NA. Duplex -guided angioplasty of failing or non-maturing arteriovenous dialysis access. Touch Brief 2007; 19(1):41-43. [ Links ]
12. Bacchini G, Cappello A, La Milia V, Andrulli S, Locatelli F. Color Doppler ultrasonography imaging to guide transluminal angioplasty of venous stenosis. Kidney Int 2000;58(4):1810-1813. [ Links ]
13. Ferring M, Claridge M, Smith SA, Wilmink T. Routine preoperative vascular ultrasound improves patency and use of arteriovenous fistulas for hemodialysis: a randomized trial. Clin J Am Soc Nephrol 2010; 5(12): 2236-2244. [ Links ]
14. Chandra A, Mix D, Varble N. Hemodynamic study of arteriovenous fistulas for hemodialysis access. Vascular 2013; 21(1):54-62. [ Links ]
15. Kumbar L, Li J, Alsmaan H, Besarab A. Novel therapeutic paradigms to treat hemodialysis access dysfunction. The Open Urology & Nephrology Journal 2014; 7(Suppl1):45-51. [ Links ]
16. Matthews R, Thomas J. Intravascular ultrasound -guided central vein angioplasty and stenting without the use of radiographic contrast agents. J Clin Ultrasound 2008; 36(4):254-256. [ Links ]
17. Gallagher JJ, Boniscavage P, Ascher E, et al. Clinical experience with office –based duplex-guided balloon -assisted maturation of arteriovenous fistulas for hemodialysis. Ann Vasc Surg, 2012; 26(7):982-984. [ Links ]
18. Guedes Marques M, Ibeas J, Botelho C, Maia P, Ponce P. Doppler ultrasound: a powerful tool for vascular access surveillance. Semin Dial 2015;28(2):206 -210. [ Links ]
19. Wang J, Blebea J, Kennedy T, Salvatore M, Kelly P. Technical aspects of duplex ultrasound-guided angioplasty of arteriovenous fistulae. J Vasc Ultrasound 2009; 33:150-154. [ Links ]
20. Ibeas -Lopez J, Vallespín -Aguado J: Ecografıa del acceso vascular para hemodialisis: conceptos teóricos, prácticos y criterios. Nefrologia 2012; 3(6):21–35. [ Links ]
21. Malik J, Kudlicka J, Novakova L, Adamec J, Malikova H, Kavan J: Surveillance of arteriovenous accesses with the use of duplex Doppler ultrasonography. J Vasc Access 2014;15(Suppl 7):S28–S32. [ Links ]
22. Lok CE, Allon M, Moist L, Oliver MJ, Shah H, Zimmerman D. Risk equation determining unsuccessful cannulation events and failure to maturation in arteriovenous fistulas (REDUCE FTM I). J Am Soc Nephrol, 2006; 17(11):3204–3212. [ Links ]
23. Gorin DR, Perrino L, Potter DM, Ali TZ. Ultrasound -guided angioplasty of autogenous arteriovenous fistulas in the office setting. J Vasc Surg 2012; 55(6):1701-1705. [ Links ]
24. Fahrtash F, Kairaitis L, Gruenewald S, et al. Defining a significant stenosis in an autologous radiocephalic arteriovenous fistula for hemodialysis. Semin Dial 2011;24(2):231–238. [ Links ]
25. Macsata RA, Scanlon J, Sidawy AN. Commentary on Duplex -guided repair of failing or nonmaturing arterio -venous access for hemodialysis. Perspect Vasc Surg Endovasc Ther 2007;19(1):56 -57. [ Links ]
Drª Maria Guedes Marques
Centro de Acessos Vasculares Nephrocare Lumiar
Rua José da Costa Pereira, nº 8
1750 -130 Lisboa, Portugal
E-mail: mariaguedesmarques@gmail.com
Conflict of interest statement: None declared.
Received for publication: 10/03/2015
Accepted in revised form: 06/05/2015














