Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Portuguese Journal of Nephrology & Hypertension
versão impressa ISSN 0872-0169
Port J Nephrol Hypert vol.31 no.2 Lisboa jun. 2017
ORIGINAL ARTICLE
Recombinant tissue plasminogen activator plus citrate versus citrate alone as catheter lock for tunnelled catheters of haemodialysis
Rita Magriço1, José Paulo Santos1, Susana Colaço1, Sara Dias2,3, Aura Ramos1
1 Serviço de Nefrologia do Hospital Garcia de Orta, Almada, Portugal
2 UIS – Unidade de Investigação em Saúde, Escola Superior de Saúde de Leiria, Leiria, Portugal
3 Epidoc unit; CEDOC – NOVA Medical School, Universidade Nova de Lisboa, Lisboa, Portugal
ABSTRACT
Introduction: The solution used to fill the lumens of the tunnelled catheters for haemodialysis (lock) influences catheter‑related complications, such as inadequate blood flow and dialysis efficacy. It is unknown whether a lock strategy with weekly administration of Recombinant Tissue Plasminogen Activator (rt‑PA) and of citrate during the remaining dialysis sessions is associated with better catheter blood flow and increased dialysis dose compared with citrate alone. Methods: We performed a prospective cross‑over study in 16 patients to compare weekly administration of 1mg per catheter lumen of rt‑PA and citrate 4% in the remaining sessions with citrate 4% administration in all dialysis sessions. Each lock strategy was performed for 24 weeks, separated by a 4‑week wash‑out period. We performed a random effects model and two paired t‑tests (in each intervention group and in each patient) to compare the mean blood flow and single‑pool Kt/V (spKt/V) of each dialysis session. Results: In the 8 patients eligible for comparison, blood flow was higher in the rt‑PA group (380.73 ± 33.43 mL/min versus 368.86 ±34.86 mL/min; p‑value <0.001). The mean increase in the random‑effects model after adjustment for time was 13.79 mL/min (95% CI 10.23‑17.34 mL/min). There was a high variability between subjects on the difference in blood flow achieved with the two lock strategies (non‑significant in 4 subjects; from 8 to 51 mL/min in the remainder). Mean spKt/V value was 1.43 in the rt‑PA group and 1.39 in the citrate‑alone group. Conclusions: When compared with citrate alone, weekly administration of rt‑PA was associated with higher blood flow and spKt/V. The clinical benefit of this intervention is questionable, since the mean increase in blood flow was 13.79 mL/min and in 4 out of 8 patients was not significant. Dose of dialysis achieved the recommended target in both groups.
Keywords: Bacteraemia, Catheters, Citric Acid, Dialysis, Plasminogen Activators, Thrombosis
INTRODUCTION
Tunnelled catheters are used as vascular access for haemodialysis by 16.1% of Portuguese patients1. Patients who use a tunnelled catheter for dialysis are at a higher risk of death than patients who perform dialysis through an arteriovenous fistula or graft2. This is in part related to the high number of catheter‑related complications.
During their lifetime, 87% of tunnelled catheters for dialysis have at least one episode of dysfunction (defined by inability to obtain a blood flow equal or higher than 300 mL/min)3. Dysfunction episodes are associated with lower dialysis efficacy4 and higher risk of bacteraemia (both due to increased necessity of catheter manipulation to improve flow and due to formation of thrombus that harbour bacteria). Half of tunnelled catheters need replacement due to dysfunction within the first year5. In up to 19% of cases, catheter replacement can be complicated with bleeding, pneumothorax or pulmonary emboli6.
The solution that fills the catheter lumens from the end of one dialysis session until the beginning of the next (lock) impacts on the risk of catheter dysfunction.
Heparin and citrate are widely used lock solutions. In our haemodialysis centre, the lock used is heparin. In the private haemodialysis centres within the referral area of our hospital, more than 90% of the patients with a tunnelled catheter use citrate 4% as a lock solution. In cases of catheter dysfunction, the catheter lumens are filled with the fibrinolytic rt‑PA (recombinant tissue plasminogen activator) to restore blood flow.
A pilot study7 showed improved blood flow with the weekly use of rt‑PA compared with heparin. A subsequent randomized clinical trial8 also compared weekly administration of rt‑PA in association with heparin with the use of heparin alone. This trial showed superiority of rt‑PA measured by increased time until first episode of catheter dysfunction and decreased number of catheter‑related bacteraemia episodes. However, in this study, the mean follow‑up time was 115.5 days in the group on the lock strategy with rt‑PA and 89 days in the group on heparin alone. Since the administration of rt‑PA improves catheter function, it is unknown whether the weekly administration of rt‑PA prolongs the lifetime of the catheter when compared with the administration of rt‑PA only in episodes of catheter dysfunction. Moreover, this intervention would only be cost‑effective in dialysis centres with a rate of catheter‑related bacteraemia higher than 1 episode per 1000‑catheter days9.
In our centre, the cost of rt‑PA administration is 15 times higher than the use of citrate or heparin (the administration of 2mg of rt‑PA costs approximately 30 euros per session per patient while heparin or citrate cost less than 2 euros per session per patient).
Regarding the comparison between heparin and citrate as lock solutions, heparin was associated with increased rate of severe haemorrhage (13 vs 4%)10, while citrate was associated with lower development of biofilm11.
A Cochrane systematic review on agents used to prevent dysfunction of haemodialysis catheters was published in 201612. The authors state that the available evidence is still insufficient to conclude on the best agent available12. A direct comparison between citrate and rt‑PA has never been performed.
The aim of our study was to compare the catheter blood flow and dialysis efficacy using two different lock strategies: citrate after every dialysis sessions versus weekly administration of rt‑PA associated with citrate administration at the remaining dialysis sessions. We performed a prospective randomized crossover study.
SUBJECTS AND METHODS
Study design
The study was designed by the investigators and procedures were considered by the ethical committee of the hospital to be in accordance with the ethical standards on human experimentation and with the Helsinki Declaration. This was an independent study.
The drugs used were provided by the pharmacy of the hospital. All participants provided written informed consent. The team responsible for lock administration and for data registry was independent from the investigation team. The principal investigator trained the nursing and administrative staff to ensure that the protocol was being followed and that data was collected correctly. Data was collected via a registration system by the nurses assisting each dialysis session. This data was then transferred to a computer database located in a server of the hospital, accessible only in the Nephrology Department. Before delivering the database for statistical analysis, the data was encoded in order to prevent identification of the subjects and to blind the statistician to the intervention performed in each period of the study. The investigators vouched for accurate completion of the protocol. All subjects were monitored for adverse events, and it was not considered necessary to stop the study for safety reasons.
Study population
Prevalent subjects performing regular haemodialysis (three sessions per week) at Hospital Garcia de Orta who were expected to use a tunnelled haemodialysis catheter until study completion were included.
Catheter dysfunction (defined by Qb≤300 mL/min) during at least one dialysis session the week before recruitment was considered an exclusion criteria. Other exclusion criteria were antibiotic use for catheter‑associated infection (recruitment was allowed after completing the antibiotic); central nervous system bleeding or any major bleeding 4 weeks prior to study enrolment; cancer located in the central nervous system; pregnancy or breastfeeding; pericarditis.
Study protocol
We performed a prospective randomized crossover clinical trial to compare two lock strategies: 1) filling the lumens of the tunnelled catheter with citrate 4% after all dialysis sessions (strategy citrate alone) or 2) administrating 1mg of rt‑PA per catheter lumen weekly (at the end of the mid‑week dialysis session) and citrate 4% on the remaining sessions (strategy rt‑PA/citrate).
The total duration of the study was 52 weeks (13 months). All subjects underwent one lock strategy for 24 weeks and then switched to the alternative lock strategy for an additional 24‑week period. To decrease the influence of one lock strategy on the alternative strategy, the observation periods were separated by a 4‑week wash‑out period, in which the lock administered was heparin (5000 UI/mL). The 4 week duration of the wash‑out period was considered sufficient since the influence of the lock solution on the catheter flow is greatest during the first two weeks after lock administration8.
The order of lock administration (citrate alone on the first 24 weeks versus rt‑PA/citrate) was decided by simple randomization with a 1:1 ratio, in order to decrease the influence of time on the results.
If a catheter dysfunction episode occurred, additional administration of rt‑PA (on demand) was allowed, independent of the lock strategy the patient was on.
Catheter dysfunction with indication for rt‑PA administration was defined by the presence of at least one of three criteria: 1. inability to start dialysis due to low blood flow; 2. blood flow ≤ 200 mL/min for at least 30 minutes of the dialysis session; 3. mean blood flow ≤ 250 mL/min on two consecutive dialysis sessions.
After finishing the trial, the subjects continued to be followed. We present the number of patients whose catheters remained in useand the number who removed them as well as reasons for catheter removal.
Procedures
The citrate formulation used was IntraLock® (Fresenius Medical Care), available in 5 mL vials. The rt‑PA formulation used was Actilyse® (Boehringer Ingelheim Pharmaceuticals), available in vials with 2 mg of rt‑PA powder and a solvent solution. Immediately before administration, the nurse added the rt‑PA powder to the solvent solution and completed the syringe with NaCl 0.9% in order to obtain an amount equal to the sum of the volumes of both catheter lumens as defined by the catheter manufacturer. Therefore, 1 mg of rt‑PA was administered into each catheter lumen.
In cases of catheter dysfunction with inability to start dialysis, 2 mg of rt‑PA were administered and catheter patency was tested 30 minutes later. In the other cases of catheter dysfunction, rt‑PA was administered at the end of the session and remained in the catheter until the next dialysis session.
Variables
Age, sex, race and aetiology of the chronic kidney disease were registered. Time since dialysis was started, type of dialysis (high‑flux versus haemodiafiltration) and type of dialysis machine were also collected. Catheter brand, location and insertion date were registered, as well as the number of tunnelled catheters inserted previously in the same location. Use of anti‑coagulants or platelet aggregation inhibitors was registered.
To evaluate catheter flow, the arithmetic mean of the blood flow registered hourly during each dialysis session was considered.
To evaluate dialysis efficacy, the single pool Kt/V (spKt/V) was measured during every dialysis session with the Online Clearance Monitor (OCM®) integrated into the Fresenius 5008 dialysis machines used in our centre.
Sample size calculation
Based on the available literature7 and the crossover design, we estimated to require a sample of 7 subjects to have 80% power to detect a 24.7 mL/min difference on catheter blood flow with different lock strategies.
Since 50% of the tunnelled catheters are used for less than a year5, we anticipated a high drop‑out rate and aimed a minimum sample size of 14 in order to have a sufficient number of subjects completing the 13 months of the study.
Statistical analysis
Data were grouped by subject. Each dialysis session was numbered consecutively from the beginning of the study in order to account for the passage of time.
To compare catheter blood flow during each 24‑week period, we used a random effects model including the following variables: baseline blood flow (defined as mean blood flow in dialysis session number 1), mean blood flow in each dialysis session, session number and lock strategy used (citrate alone versus rt‑PA/ citrate).
We calculated the regression coefficient of each variable and the corresponding 95% confidence interval.
To calculate the difference in catheter blood flow and spKt/V, we performed a paired t‑test considering all subjects simultaneously. Additionally, we evaluated the difference on blood flow in each subject individually by a paired t‑test.
A p‑value < 0.05 was considered statistically significant.
RESULTS
Seventeen subjects were eligible for the study, one of whom refused to participate. Fifteen out of the 16 subjects enrolled started the study in September 2015 (1 started one month later). At the time the lock strategy was switched, only 8 out of the 16 subjects remained in the study and were therefore eligible for comparison of blood flow with both lock strategies.
In the subgroup of 8 subjects who did not start the second period of the study, 3 died from causes not related to the catheter (one from gastric cancer and two from infected pressure ulcers). The catheter was removed in 3 patients because either an arteriovenous fistula or a graft became available. Of these six patients, five were on the citrate‑alone lock strategy. The seventh subject, who was on the rt‑PA/ citrate lock strategy, had his catheter removed due to catheter‑related bacteraemia.
The eighth patient, who was on the citrate‑alone lock strategy, had an acute subdural haematoma and the investigation team decided not to continue the study into the rt‑PA/citrate strategy. There were no other cases of major bleeding or catheter‑associated infection in the remaining 14 subjects.
Subjects eligible for blood flow comparison with the two lock strategies
The 8 subjects who started the second period of the study completed the 13 months of the study. Their baseline characteristics are presented in Table I.
Subjects number 5 and 13 were black and the remainder were Caucasians. All subjects used Fresenius 5008® dialysis machines. Subjects number 6 and 13 were under haemodiafiltration (using CD‑FX600® dialysis filters) and the remainder used FX80® filters for high‑flux dialysis.
All subjects had a tunnelled catheter of the Mahurkar® brand (inserted in the right jugular vein in all except in subject number 5, who had the catheter in the left jugular vein). Arterial and venous lumen volumes of the catheters inserted in the right jugular vein were respectively 1.8 and 1.9 mL and for catheters placed in the
left jugular vein of 2.0 and 2.1 mL. Four subjects (numbers 1, 2, 6 and 7) had already had a tunnelled catheter placed in the same location. No subjects were under anti‑coagulants.
Subjects number 2, 8 and 9 were under platelet aggregation inhibitors.
Random effects model
The random effects model comparing blood flow between the two lock strategies in the 8 subjects who started the second observation period is presented in Table II. In the random effects model, the variable lock strategy used took the value 0 when citrate was administrated and 1 when the lock strategy was rt‑PA/citrate.
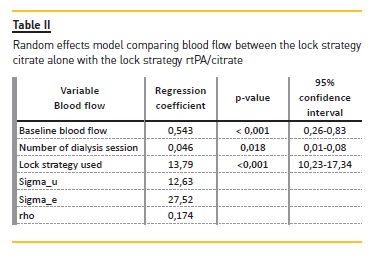
The blood flow was higher in the rt‑PA/citrate lock strategy than in the citrate‑alone
lock strategy (regression coefficient 13.79 mL/min, 95% confidence interval 10.23‑17.34 mL/min, p‑value <0.001). As the number of dialysis session was included in the random effects model, the regression coefficient was adjusted for the factor of time.
The blood flow distribution was normal and presented a standard deviation (sigma_u) of 12.63 mL/min. Importantly, a high variability in blood flow was detected (sigma_e 27.52) and 17.4% of the variability (rho) was due to differences between subjects.
Paired t‑test
In the global analysis, the mean blood flow was 368.86 mL/min (SD ± 34.86 mL/min) in the citrate‑alone strategy and 380.73 mL/min (SD ± 33.43 mL/min) in the rt‑PA/citrate strategy (mean difference 11.86mL/min, 95% confidence interval 8.56‑15.18mL/min, p‑value<0.001).
Since a high variability between subjects was detected, we performed a paired t test in each patient to assess individual blood flow difference with both lock strategies. There were no significant differences in blood flow in 4 out of the 8 subjects (Table III).
On demand administration of rt‑PA
On the 8 patients evaluated with the two lock strategies, there were 5 episodes of catheter dysfunction: 3 episodes occurred in patient number 1, one episode in patient number 6 and one episode in patient number 7.
All episodes occurred while patients were on the citrate‑alone lock strategy. In the five cases, 2mg of rt‑PA were administered at the end of the session and remained in the catheter until the next dialysis session.
Dialysis efficacy
The mean spKt/V of subjects while on the citrate‑alone lock strategy was 1.39 and 1.43 on the rt‑PA/citrate strategy (mean paired difference 0.04, 95% confidence interval 0.02‑0.06, p‑value 0.001).
Follow‑up of patients after finishing the trial
After the trial, the 8 patients were switched to the standard lock strategy of our dialysis centre: heparin 5000 UI/mL at every session and on demand rt‑PA administration in cases of catheter dysfunction. Four patients continue to use the catheter, which allows adequate blood flow and dialysis efficacy. Two patients continued to have an adequately functioning catheter until they died from causes unrelated to the catheter. Two patients obtained an alternative vascular access for dialysis.
DISCUSSION
Our study enrolled 16 subjects to compare two lock strategies for tunnelled catheters of dialysis (citrate alone versus rt‑PA/citrate) in a prospective randomized
crossover study. Three subjects died from causes unrelated with the dialysis catheter: 3 received a fistula or graft; 1 (who was on the rt‑PA/ citrate strategy) had a bacteraemia and catheter removal and 1 (who was on the citrate‑alone strategy) had a subdural haematoma and the investigators decided not to switch to the lock strategy with rt‑PA/citrate. The group of 8 subjects who switched to the second lock strategy completed the 13 months of the study and were eligible for blood flow comparison. Blood flow was higher on the rt‑PA/citrate strategy but the calculated mean difference between the two lock strategies was 13.79 mL/min (in the random effects model adjusted for the factor of time) and 11.86 mL/min (in the paired t‑test).
An important variability between subjects was detected and only 4 out of the 8 subjects had a higher blood flow in the individual paired t‑test.
The efficacy of dialysis (measured by spKt/V) reached the recommended minimal target13 with both lock strategies.
We acknowledge some limitations to our study, namely the fact that it is open‑label and the small number of subjects enrolled. Despite the patients being randomized, the number of subjects who reached the switch date was unbalanced (of the 8 patients eligible for blood flow and spKt/V comparison, six started on the rt‑PA/citrate lock strategy and two on the citrate‑alone strategy). Importantly, the study was not powered to evaluate difference in catheter‑related bacteraemia between the two lock strategies used.
Regarding the strengths of our study, this is a prospective independent study. Although citrate is frequently used to lock tunnelled dialysis catheters, as far as the authors are aware, no direct comparison with rt‑PA has been previously performed. A crossover study has two advantages over both a parallel study and a non‑crossover longitudinal study. First, the influence of confounding covariates is reduced because each crossover patient serves as his or her own control. Second, optimal crossover designs are statistically efficient and so require fewer subjects than do non‑crossover designs. The subjects were all from the same dialysis centre and were included within one month, which further reduces variability associated with different medical care in different centres or in different periods of time.
Only 8 out of the 16 subjects enrolled remained in the study at the time of lock strategy switch. This was expected because, both in our experience and in the published literature, 50% of the catheters placed are removed in the first year after the catheter is placed5.
Causes for removal were death unrelated with the catheter (3 subjects) and maturation of an alternative vascular access for dialysis (3 subjects).
The only patient who had a major bleeding was on the lock strategy with the lowest haemorrhagic risk (citrate alone). Additionally, the only patient who had a catheter‑related bacteraemia was on the lock strategy with weekly administration of rt‑PA, which was associated in previous studies with decreased risk of catheter‑related infection8. Therefore, it seems important not to overemphasize the benefits of each lock strategy.
Tunnelled catheters for dialysis are associated with increased risks independent of the lock strategy used, and must be reserved for subjects where a fistula or graft cannot be used.
The lock strategy rt‑PA/citrate was associated with higher blood flow. It should be considered whether this significant result from a mathematical point of view is significant from a clinical perspective. A previous pilot trial with methods very similar to our study compared rt‑PA/heparin with heparin alone and demonstrated increased blood flow with the rt‑PA/heparin lock strategy7. The magnitude of the increase was higher (24.7 mL/min)7 than the difference we detected in our study. In a subsequent randomized clinical trial also comparing rt‑PA/heparin with heparin alone, the use of rt‑PA/heparin was associated with increased time until first catheter dysfunction8. However, it is unknown whether rt‑PA administration can restore blood flow so that the lifetime of the catheter or the dialysis efficacy are unaffected. In our study, rt‑PA was administered regularly in the rt‑PA/ citrate lock strategy and on demand in cases of catheter dysfunction. Catheter dysfunction occurred only in subjects on the citrate‑alone lock strategy (5 episodes, 3 of which were in the same patient), but all catheters presented adequate patency and allowed delivery of an adequate dose of dialysis throughout the study. It is therefore possible that a lock strategy with on‑demand administration of rt‑PA in cases of catheter dysfunction is sufficient to prolong the catheter lifetime and deliver an adequate dose of dialysis.
The randomized controlled trial previously described also demonstrated a decreased incidence of catheter‑related bacteraemia8 with the lock strategy rt‑PA/heparin when compared with heparin alone (rate of 0.4 versus 1.37 episodes per 1000 catheter‑days).
A cost‑effectiveness analysis based on the results of this trial was presented posteriorly9. The authors concluded that the weekly administration of rt‑PA would only be cost effective in centres where the rate of catheter‑related bacteraemia is higher than 1 episode / 1000 catheter‑days.
All subjects of our unit eligible for the study except one agreed to enter the study, so we consider this sample to be representative of the reality in our centre. In our sample 1 episode of catheter‑related bacteraemia occurred in 16 subjects followed until the catheter was removed or until the end of 13 months of follow‑up.
The incidence of catheter‑associated bacteraemia in our centre is therefore lower than 1 episode/1000 catheter‑days.
The episode of catheter‑related bacteraemia occurred in a patient on the rt‑PA/citrate lock strategy, which was unable to prevent this infection.
It is surprising that there is a high variability between subjects regarding change in blood flow when comparing the use of citrate alone with the use of rt‑PA/citrate as a lock strategy. In some subjects, there is no effect on blood flow with the change of lock strategy and in others the blood flow is up to 51 mL/min higher with the strategy rt‑PA/citrate. If implemented, we consider that the routine weekly administration of rt‑PA as a lock strategy must be maintained only after confirmation of improvement in blood flow.
After the trial, patients were switched to a lock strategy with heparin and rt‑PA administration in cases of catheter dysfunction. This lock strategy seems adequate to maintain catheter blood flow and capacity to deliver an adequate dose of dialysis. In fact, 4 out of the 8 patients maintained the catheter while it was necessary (until an alternative vascular access was available or the patient died from causes unrelated with the catheter), and the other four continued to have a functioning catheter.
In conclusion, our study showed increased blood flow with the weekly administration of rt‑PA as a lock strategy compared with the use of citrate alone and on‑demand administration of rt‑PA.
The clinical significance of the difference achieved is questionable, since with the administration of citrate alone catheters remained patent and able to deliver an adequate dose of dialysis. We consider that the lock strategy with weekly administration of rt‑PA and of citrate in the remaining sessions of dialysis should be reserved for subjects where achieving a higher blood flow is considered clinically beneficial or in centres with an incidence of catheter‑related bacteraemia higher than 1 episode per 1000 catheter‑days.
Since the response in blood flow is highly variable between subjects, we suggest monitoring blood flow after change of the lock strategy, and maintaining weekly administration of rt‑PA only in cases where blood flow improves.
References
1. Substitutive Renal Therapy of Chronic Renal Disease in Portugal. Available at http://www.bbg01.com/cdn/clientes/spnefro/noticias/130/REGISTO_DRCV2016.pdf. Accessed May 16, 2017 [ Links ]
2. Belino C, Coelho A, Pereira S, Lopes D, Gomes AM, Ventura A. Survival of hemodialysis patients: A new reality? Port J Nephrol Hypert 2017; 31 3‑41 [ Links ]
3. Suhocki P, Conlon PJ, Knelson M. Silastic cuffed catheters for hemodialysis vascular access: thrombolytic and mechanical correction of malfunction. Am J Kid Dis. 1996; 28: 379‑386 [ Links ]
4. Rayner H, Pisoni R. The increasing use of hemodialysis catheters: evidence from the DOPPS on its significance and ways to reverse it. Semin Dial. 2010; 23: 6‑10 [ Links ]
5. Ponikvar R, Buturovic‑Ponikvar J. Temporary hemodialysis catheters as a long‑term vascular access in chronic hemodialysis patients. Ther Apher Dial. 2005; 9: 250‑253 [ Links ]
6. Lomonte C, Libutti P et al. Efficacy and Safety of a New Technique of conversion from Temporary to Tunneled Central Venous Catheters. Semin Dial. 2015; 28: 435‑438. [ Links ]
7. Schenk P, Rosenkranz A, Wölfl G. Recombinant tissue plasminogen activator is a useful alternative to heparin in priming quinton permcath. Am J Kid Dis. 2000; 35:130‑136 [ Links ]
8. Hemmelgarn B, Moist L, Lok C. Prevention of dialysis catheter malfunction with recombinant tissue plasminogen activator. N Engl J Med. 2011; 364:303‑312 [ Links ]
9. Manns BJ, Scott‑Douglas N, Tonelli M, et al. An economic evaluation of rt‑PA
Locking solution in dialysis catheters. J Am Soc Nephrol. 2014; 25:2887‑2895.
10. Stas KJ, Vanwalleghem J, De Moor B, Keuleers H. Trisodium citrate 30% vs heparin 5% as catheter lock in the interdialytic period in dialysis catheters for intermittent haemodialysis. Nephrol Dial Transplant 2001; 16:1521‑1522 [ Links ]
11. Shanks RM, Sargent JL, Martinez RM, Graber ML, OToole GA, Catheter lock solutions influence staphylococcal biofilm formation on abiotic surfaces. Nephrol Dial Transplant. 2006; 21:2247‑2255 [ Links ]
12. Wang Y, Ivany JN, Perkovic V, Gallagher MP, Woodward M, Jardine MJ. Anticoagulants and antiplatelet agents for preventing central venous haemodialysis catheter malfunction in patients with end‑stage kidney disease. Cochrane Database Syst Rev. 2016; 4:CD009631. [ Links ]
13. NKF‑KDOQI clinical practice guidelines; update 2006. Am J Kidney Dis. 2006; 48(Suppl1): S2‑S90. [ Links ]
Rita Magriço
Rua Luís Pastor de Macedo, Lote 17/18 3ºD 1750‑159 Lisboa
E-mail: rita.magrico@yahoo.com
Contributions of the authors to the article: All authors contributed to study design, interpretation and discussion of the results and drafting of the manuscript. RM and SD performed the statistical analysis.
ACKNOWLEDGEMENTS
The authors acknowledge the participation of the subjects enrolled and the help of the staff of the Nephrology Department, namely the administrative, nursing and medical teams. We also thank the cooperation of the Hospital Pharmacy for providing the drugs used, and of Centro Garcia de Orta, Ethical Committee and Administration Board of Hospital Garcia de Orta for approving the study protocol. Finally, we thank the Harvard Medical School and Dr Finnian McCausland for reviewing the protocol in the form of Capstone Project.
Disclosure of potential conflicts of interest: none declared.
Received for publication: May 23, 2017
Accepted in revised form: Jun 29, 2017














