INTRODUCTION
Coronavirus disease 2019 (COVID-19) due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection has affected millions worldwide, and in particular the care of patients on maintenance hemodialysis (HD). In Portugal, from March 2nd until the end of the year of 2020, a total of 413,678 people were infected, with up to 6,906 deaths.1 Several clinical studies and meta-analysis have demonstrated that the elderly and patients with comorbidities, such as diabetes mellitus, hypertension, cardiovascular
disease, pulmonary chronic disease, cancer and chronic kidney disease (CKD) are prone to develop severe disease and have poorer outcomes.2,3,4,5,6The earlier published reports found that HD patients presented with less symptoms and a milder course, often asymptomatic, whereas more recent papers have shown that clinical presentation is similar to the general population.2-4,7,8,9,10
Patients on HD are at particular high risk for severe COVID-19 infection due to their old age, multiple comorbidities, and relative immunosuppression due to uremia. Another contributor for the greater risk is inherent to the dialysis treatment, since there is frequent contact with other patients, even though preventive and isolation measures were implemented at the dialysis facilities at the beginning of the COVID-19 outbreak.7 In fact, the mortality rates that have been reported are far higher than in the general population, with the European Renal Association and Transplant Association Registry reporting 20% mortality rate among patients with end-stage kidney disease.7 However, evidence on particular features of COVID-19 as well as on predictors for mortality in HD patients is still lacking.
The aim of our study was to compare the clinical presentation, laboratory and radiology data, and outcomes between HD and nondialysis COVID-19 hospitalized patients and find possible risk factos for mortality in HD patients.
MATERIAL AND METHODS
Population Selection and Study Design
We conducted a single-center retrospective cohort study from 1st March 2020 to 31st December 2020 including all patients on maintenance HD admitted to Centro Hospitalar Vila Nova de Gaia/Espinho with a confirmed SARS-CoV-2 infection. Asymptomatic
patients and those admitted only for public health reasons were excluded. We used propensity score matching (without the use of a caliper width) to adjust for age and sex, to compare HD patients to a control group of non-dialysis patients hospitalized with a confirmed SARS-CoV-2 infection (1:1). All patients enrolled in this study had a confirmed SARS-CoV-2 infection diagnosed by real time PCR SARS-CoV-2 test.
Data Collection
Data regarding patients baseline characteristics, symptoms, laboratory, and radiology findings at presentation, length of hospital stay, treatment regimens (antimalarial and antiviral agents, glucocorticoids and ventilatory support), clinical outcomes, comorbidities and use of angiotensin converting enzyme inhibitor/angiotensin receptor blockers (ACEi/ARB) were collected by consulting electronic medical records. Obesity was defined as a body mass index superior to 30 Kg/m2. The Katz index was used to determine the degree of autonomy in activities of daily living based on data from the clinical process: a score of above 4 was “independent”, a score of 3 or 4 was “partially dependent” and below 3 “dependent”. Bacterial superinfection was defined as a positive bacterial culture from a lower respiratory tract specimen (sputum, bronchial/tracheal aspirates or bronchoalveolar lavage).
Clinical Management
In respect to therapy, from March to August 2020, hydroxychloroquine and lopinavir/ritonavir was given to patients with PaO2/FiO2 <300 or with radiological evidence of pneumonia unless they had prolonged QT on electrocardiography.
From September 2020 until December 2020, patients were treated with intravenous dexamethasone if they needed supplementary oxygen or ventilation or if they had acute respiratory distress syndrome or septic shock. COVID-19 patients were treated with remdesivir if they were within the first six days of symptoms and if they needed
supplementary oxygen and had no absolute contraindication (transaminases above 5 times the normal range and glomerular filtration rate inferior to 30 mL/min).
Ethical concerns
Our research was conducted in full accordance with the World Medical Association Declaration of Helsinki. Informed consent was waived as part of the public health outbreak investigation.
Statistical analysis
Categorical variables were presented as frequencies and percentages and were compared with the use of Fisher’s exact test or the chi-square test, as appropriate. Continuous variables were presented as means and standard deviations, or medians and 25th and 75th percentile for variables with skewed distributions. Normal distribution
was checked using Kolmogorov-Smirnov test or skewness and kurtosis.
Continuous normally distributed variables were compared with the use of Student’s t-test and continuous variables with non-normal distribution were compared with the Mann-Whitney test. Kaplan-Meier estimates were used to construct the survival curves. Bivariate logistic regression was used to find mortality predictors of HD patients. All reported p values are two-tailed, with a p value of 0.05 indicating statistical significance. Statistical analyses were performed by SPSS for Windows software version 23.0 (SPSS Inc., Chicago, IL).
RESULTS
In total, 34 maintenance HD patients were admitted at our center with COVID-19 and were age and gender matched to 34 non-dialysis patients. Median time on maintenance HD was 3.0 [0.5-23] years. Table I illustrates the comparison between maintenance HD patients and the control group. Baseline characteristics and comorbidities were similar between groups, except for peripheral arterial disease that was more frequent in HD patients (20.6% vs 2.9%, p=0.024) and cerebrovascular disease that was more common in the control group (17.6% vs 52.9%, p=0.002). There was no difference in the use of ACEi/ARB. COVID-19 symptoms were similar between groups, with fever the most frequent symptom, present in 67.6% of patients. However, more patients in the HD group presented with respiratory insufficiency and needed supplementary oxygen (50.0 % vs 8.8%, p<0.001).
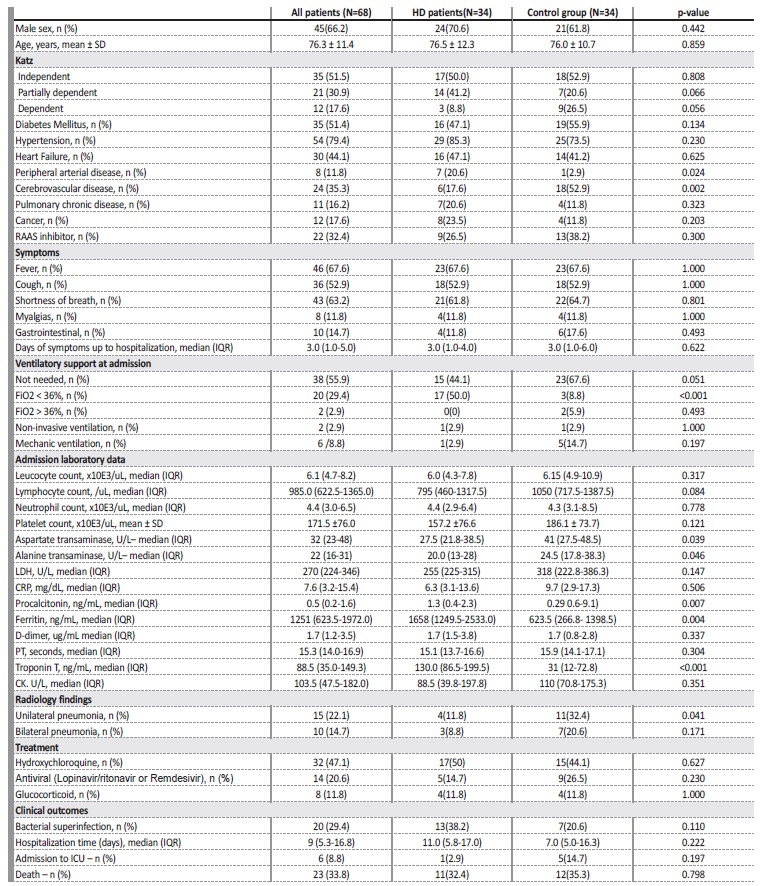
Table I Comparison between baseline characteristics, comorbidities, laboratory data and radiology findings and clinical outcomes between chronic hemodialysis and control group.
CK - creatinine kinase; CRP - C reactive protein; HD - hemodialysis; ICU - intensive care unit; IQR - interquartile range; LDH - lactate dehydrogenase; PT - prothrombin time; RAAS - renin angiotensin aldosterone; SD - standard deviation.
Patients in the HD group had higher procalcitonin (1.3 vs 0.3 p=0.007), ferritin (1658.0 vs 623.5, p=0.004) and troponin T (130.0 vs 31.0, p<0.001) levels versus the control group. Transaminases were higher in the control group (32.0 vs 27.5, p=0.039; 20.0 vs 24.5, p=0.046).
Unilateral pneumonia in the chest X-ray was more frequent in the control group (11.8% vs 32.4%, p=0.041).
Therapeutic options and clinical outcomes (hospital stay, bacterial superinfection, admission to intensive care unit (ICU) and mortality) were similar in both groups.
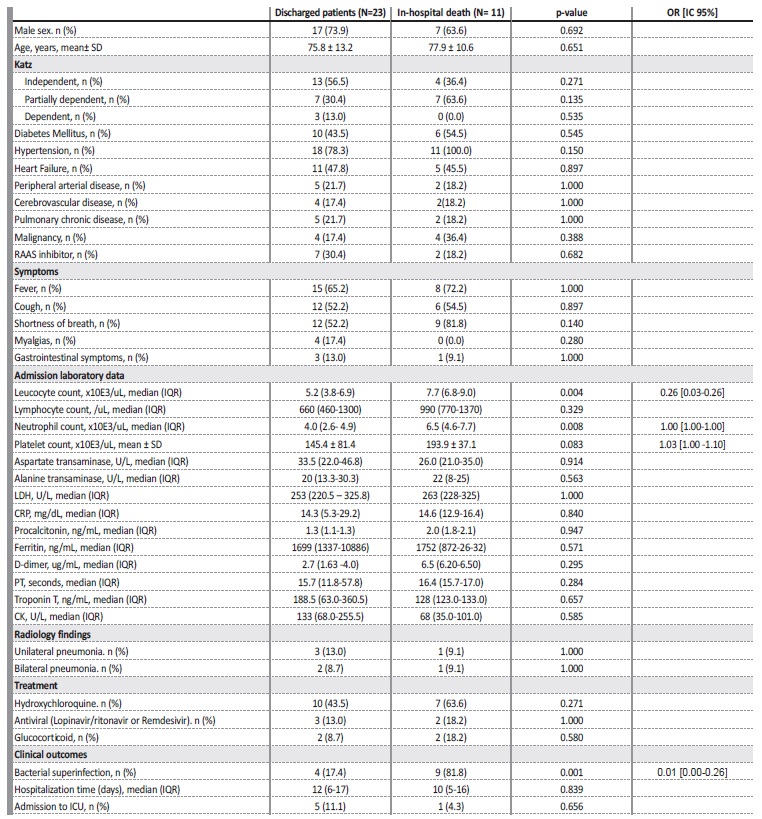
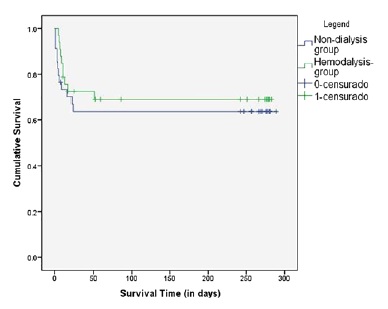
Maintenance HD and control group presented similar survival curves (log rank = 0.448. p=0.503) (Figure 1). Table IIcompares maintenance HD patients who died during the
hospitalization and discharged patients. The large majority (91.7%, n=11) of HD patients with an indication to ICU admission were refused. Leucocyte (5.2 vs 7.7, p= 0.004) and neutrophil (4.0 vs 6.5, p=0.008) count were higher in the mortality group. Bacterial superinfection was also more frequent in the in-hospital death group. After adjusting for covariables, only bacterial superinfection was a predictor of inhospital mortality for HD patients (OR 0.01 [0.00-0.26]).
CK - creatinine kinase; CRP - C reactive protein; HD - hemodialysis; ICU - intensive care unit; IQR - interquartile range; LDH - lactate dehydrogenase; PT - prothrombin time; RAAS - renin angiotensin aldosterone SD - standard deviation.
DISCUSSION
To our best knowledge, this is the first Portuguese study comparing outcomes of HD patients and propensity matched non-dialysis patients infected with COVID-19.
COVID-19 symptoms in the HD group were the same as in the control group. The earlier published reports found that HD patients presented with fewer symptoms and a milder course, whereas more recent studies have shown that clinical presentation is similar to the general population.2-4,7-10More patients in the HD group presented with respiratory insufficiency and needed supplementary oxygen. That could be explained by the contribution of hypervolemia, since acutely ill HD patients sometimes present weigh loss that could be not immediately noticed.
Comparing with the control group, patients in the HD group had higher procalcitonin, ferritin and troponin T levels. Procalcitonin is na early predictor of infection in HD patients and a predictor of bacterial infection.11,12Although median procalcitonin levels were higher in the HD patients, there was similar rates of bacterial superinfection between groups. Some reports showed that chronic HD per se may affect procalcitonin levels.11-13Ferritin could be a marker of systemic inflammation and higher levels are seen in chronic diseases.14
Therefore, basal levels of ferritin on HD patients could be higher and this could explain the difference between groups. Also, the finding of higher levels of T troponin in the HD group was not unexpected.
Baseline troponin T levels are higher in CKD patients, and when stable, do not signify acute myocardial infarction. Such elevations are thought to be related to the reduced clearance of such markers by the kidneys as well as due to chronic and persistent damage to cardiac myocytes via mechanisms associated with CKD.15 Transaminases were higher in the control group, also reported in another study.4 Serum aminotransferase levels are lower in HD patients, with or without viral hepatitis, compared to individuals with normal renal function.16
D-dimers and C reactive protein that are reported to be higher in HD patients were similar between groups.17,18These findings question whether regular criteria for defining high risk COVID-19 patients should be applied to HD patients.
Unilateral pneumonia in the chest X-ray was more frequent in the control group (11.8% vs 32.4%, p=0.041). These results may have some bias due to observer-dependent subjectivity on radiography observation.
There were no differences in both groups in terms of COVID-19 treatment and clinical outcomes. Glucocorticoid treatment was applied only to 11.8% of HD patients because the vast majority was admitted before the establishment of the dexamethasone protocol in our center.
Although the use of antiviral therapy in HD patients is controversial, the control group had equally elderly patients with multiple comorbidities, which may also have constituted contraindications to those therapies. We also report low rates of ICU admission and this as well could be explained by the advanced age and high prevalence of comorbidities of both groups.
We report a mortality rate of 32.4% on HD patients which is in line with other studies that report in-hospital mortality on HD COVID-19 patients of 27%-32%.2,8-10,19We did not find differences in mortality between HD and control group. Recent studies also reported that the degree of disease severity and the mortality rate of dialysis patients was similar to an age and gender matched control population.3,8
Leukocytosis, neutrophilia, and bacterial superinfection were more common in HD patients who died during hospitalization. Shang W et al. also reported that leucocytes and neutrophil count were predictive of a poor prognosis among maintenance HD patients infected with SARS-CoV-2.20Although some studies have shown that lymphopenia is a predictor of disease severity in the general population, our results were not consistent with that.21 After adjusting for other confounders, only bacterial superinfection was a risk factor for mortality among dialysis patients. Other established risk factors for mortality in COVID-19 patients, such as age, diabetes, heart disease, or chronic obstructive lung disease were not associated with higher mortality in HD patients.22,23
Several limitations of this study should be acknowledged. First, this is a single-center retrospective study with a small size sample, and some patients’ laboratory and clinical data were incomplete.
Second, we only included hospitalized patients and therefore patients with mild disease were excluded. A multi-center retrospective study should be conducted to include a larger sample size across multiple centers to better assess the effects of COVID-19 infections in HD patients.
CONCLUSION
Our study compared outcomes for COVID-19 patients on maintenance HD to non-dialysis patients with similar age, gender and comorbidities and showed no difference in hospital stay or death rate.
Despite these results, we must emphasize that mortality in the dialysis group was exceptionally high, with up to 32% of in-hospital mortality, and that bacterial superinfection has been shown to be an independente predictor of mortality. Hence, we intend to highlight the importance of interventions, such as full vaccination coverage, to mitigate the burden of COVID-19 in HD patients.