INTRODUCTION
Socioeconomic status (SES) is an important health determinant encompassing several dimensions, namely education, occupation and income1,2. This study focuses on income. In Portugal, and similarly to other European Countries, a National Health Care System was created and implemented in 1979 in order to attenuate inequality and provide universal healthcare. Further support includes identification of patients with economic insufficiency by attributing Low-Income status (LIs). This exempts them from health-related taxes and grants other privileges related to healthcare3. To be eligible, the income per household member must be below a stipulated, and periodically updated, threshold3.
Low SES has long been associated with increased incidence of chronic diseases, risk factors4-9 and even poor disease management. In fact, this is well illustrated by worse glycemic control in low SES diabetic patients.10 Similarly, this population also shows increased incidence of Chronic Kidney Disease (CKD)11-17 and worse outcomes18,19. The mechanisms behind this association are multiple and include: health behavior (unhealthy habits and lack of information); access to healthcare (geographic or incomerelated); biological features (low birthweight, genetic predisposition, inadequate nutrition); and environmental factors (exposure to diseases, nephrotoxic agents or lack of sanitation).11 Regardless of economic constraints, the process leading up to dialysis in CKD patients respects several steps deemed fundamental in proper kidney care.
These include: 1) Referral to a Nephrologist for assessment, treatment of underlying reversible factors and follow-up; 2) Explanation of the multiple kidney replacement therapy (KRT) options in na appropriate environment and by specialized Nephrologists; 3) Choice, by the patient, of KRT; 4) Vascular mapping and timely vascular access evaluation and intervention if blood-based KRT was selected; 5) Initiation of dialysis. The purpose of this study is to evaluate the effects of low-income in referral and overall management of CKD in a Portuguese center cohort.
METHODS
We designed a retrospective cohort study involving maintenance dialysis patients (MDP) at a medium-sized public Nephrology center. Inclusion criteria included: a) undergoing at least three successive dialysis sessions between June/2017 and June/2021; and b) Endstage kidney disease (ESKD) resulting from progressive diseases (diabetes, hypertension, type 2 cardiorenal syndrome or multifactorial).
Exclusion criteria focused essentially on the etiology of ESKD, namely acute kidney injury, multiple myeloma or other malignancy, glomerulonephritis, polycystic kidney disease or another genetic disease and immunological disorders, such as vasculites or lupus.
Patients´ files and records were revised, and data was collected specifically for the aims of the study, with a database that excluded any information liable to identify any of the patients. Information was obtained from clinical records in accordance with the declaration of Helsinki. Variables included: 1. presence of LIs; 2. Sérum creatinine (sCr) and estimated glomerular filtration rate (eGFR) at referral; 3. presence of ambulatory KRT-options appointment (KRTOa), which does not include urgent or inpatient education/choice of KRT, but rather requires an appropriate scheduled specialized consult; 4. timely vascular access evaluation (defined as either initiation by arteriovenous fistulae or evaluation by vascular surgeon 8 weeks before dialysis start); 5. time to dialysis since referral.
STATISTICAL ANALYSIS
Statistical analysis was carried out using Microsoft Excel 2016 and IBM SPSS Statistics 25 software. Descriptive analysis was performed using frequencies and percentages for categorical variables, whereas continuous variables are presented using means with standard deviations, if normally distributed, or medians with interquartile range, for skewed distribution.
Differences in eGFR/Creatinine between groups were analyzed with Student’s t-test for means. Additionally, successive and progressive CKD staging at referral was submitted to Mantel-Haenzsel Chisquare test for linear trend. Presence of KRT appointment and timely vascular access were compared using measures of association with Fisher’s exact test and strength of association with Phi correlation coefficient. Time to dialysis was compared using Student’s t-test for means and computed for two-years from referral as survival analysis (with dialysis start as the event) using Kaplan Meier estimator, Cox regression and Log-Rank test. To better understand the results, further exploratory analysis was performed using eGFR adjusted Cox regression for time to dialysis and Pearson’s correlation test for a relation between eGFR at referral and time to dialysis. Tests were considered significant for p below 0.05.
Table 1 Relevant descriptive and comparative analysis
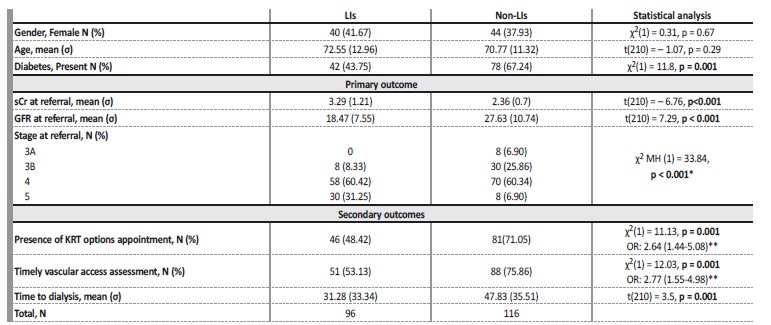
*Mantel-Haenzsel test for linear trend; ** Odds Ratio presented as negative outcomes (absence of KRTOa and untimely assessment) for LIs group, with 95% Confidence Intervals for LIs - Low-Income status; non-LIs - Not Low-Income status; X2 - Chi-square; σ - Standard deviation; t - t value for Student’s t-test for difference in means; sCr - serum creatinine; GFR - glomerular filtration rate; MH - Mantel-Haenzsel; KRT - kidney replacement therapy
RESULTS
A total of 212 participants were evaluated, 96 of whom with LIs. When comparing LIs and non-LIs for demographic variables, there was no difference between ages (72.6 vs. 70.8, p = 0.29) or genders (41.7 vs. 37.9 % Female, p = 0.67). There was, however, significant difference between diabetes prevalence rates, which were weakly associated with non-Lis (43.8 vs. 67.2 %, p = 0.001, Phi = -0.236).
Primary outcome: LIs presented higher sCr (3.29 vs. 2.35 mg/dl, t = - 6.76, p<0.001) and, consequently, lower eGFR (18.47 vs. 27.63ml/min/1.73 m2, t = 7.29, p<0.001) at time of referral (Table 1). Secondary outcomes: a) LIs group was weakly associated with the absence of KRTOa (48.1 vs. 25.5 %, Phi = 0.23, p = 0.003). For this sample, patients without KRTOa were 2.64 times (OR) more likely to belong to the LIs group (95% CI: 1.44-5.08). Independently of the presence of LIs, patients without a KRTOa had lower eGFR at referral, though the difference was not significant (22.0 vs 24.6 ml/min/1.73 m2, p = 0.1); b) Regarding timely vascular access creation, LIs weakly associated
with late vascular management (46.9 vs. 24.1 %, Phi = 0.24, p= 0.001). Patients that had a delayed evaluation and vascular management were 2.8 times (OR) more likely to belong to the LIs group (95% CI: 1.55-4.98). Independently of the presence of LIs, late vascular access management group showed significantly lower eGFR at referral (21.1 vs 24.5 ml/min/1.73 m2, p = 0.01); c) Overall, LIs group showed a shorter time to dialysis (31.3 vs. 47.8 mo, t (202) = 3.41, p = 0.001).
Survival analysis for dialysis-free time from referral was computed for 24 months. Firstly, Kaplan Meier estimator (Figure 1A) revealed a mean time to dialysis that persisted significantly different (15.77 vs 20.71 months, Log-R test: ꭓ2(2) = 13.04, p < 0.001). In an unadjusted model using Cox regression (Figure 1B), LIs patients were more likely to start dialysis during the 24 months from referral (HR: 2.11, 95% CI: 1.39-3.21, p<0.001). However, when adjusted for eGFR at referral (Figure 1C), the difference was not significant (HR: 1.16, 95 % CI: 0.74 - 1.80, p = 0.53). Further analysis using Pearson’s test revealed a correlation between eGFR and time to dialysis from referral, r(210) = 0.52, p<0.001.
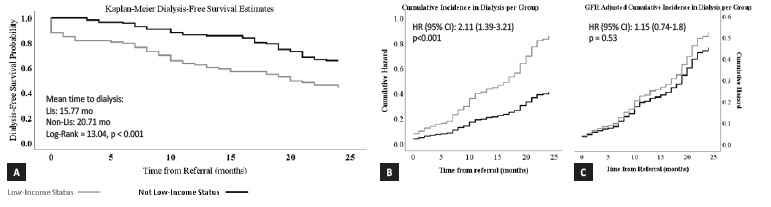
Figures 1A, 1B and 1C. Dialysis-free survival analysis at 24 months from referral. (A) Kaplan-Meier estimates plot reveals a higher probability of incident dialysis in the LIs group, corroborated by a statistically significant Log-Rank Test (p < 0.001). (B) Cox Regression reveals an increased cumulative incidence in the LIs. (C) After adjusting for GFR at referral, Lis patients no longer show increased cumulative incidence or statistically significant hazard ratio for dialysis start.
DISCUSSION
This is a positive study suggesting important differences in kidney care depending on Portuguese CKD patients SES. Firstly, demographic data shows no difference between ages or genders, but there is na increased rate of diabetes among non-LIs group. This was unexpected since low-SES is a known risk factor for metabolic syndrome and poor
health choices.7,8 Regarding the primary outcome, sCr values are high and, consequently, eGFR is low (18.47 vs. 27.63 ml/min/1.73m2). The inclusion criteria, namely the referral date starting in 2010, along with being on regular dialysis from 2017 to 2021 influences these values, as it excludes patients on MDP at the same period of time but whose referral was earlier (before 2010), who may have had better eGFR at referral. However, this is a limitation that is transversal to both groups and does not benefit neither, therefore the eGFR difference remains significantly high and worrisome. KDIGO guidelines support an eGFR under 30 ml/min/1.73m2 as an absolute indication for Nephrology referral regardless of etiology or the presence of proteinuria.20 In this study, we see that the non-LIs group is close to this premise (27.63 ml/min/1.73m2), whereas the LI group is not only lower, but already approaching stage 5 (18.47 ml/min/1.73m2). Numerous studies have reported a relationship between late referral and worse outcomes21-24, including increased mortality25 and reduced access to transplantation26.
When approaching the secondary outcomes, LIs group is both significantly associated with untimely vascular access assessment and lack of KRTOa. Furthermore, untimely vascular access assessment and lack of KRTOa both show a lower eGFR at referral, although not significant for the second of these outcomes. This only reinforces the relationship between late referral and the skipping of fundamental steps in pre-dialysis kidney care. Regarding time to dialysis, it was shorter in the LIs, and patients from this group were more likely to be in dialysis at 24 months from referral. This outcome is expected, since higher eGFR correlate with more time to dialysis. To further understand the effect of LIs, Cox regression was performed for incidence in dialysis in both groups but adjusted for eGFR. Since the adjusted function was not significantly different between the groups, we assume the eGFR declining rate after referral is similar and independente of income.
By combining these results, this study supports the hypotheses that there is an increased risk of late Nephrology referral among Portuguese CKD LIs patients, which may be associated with worse outcomes and leads to less time to dialysis and also less time to prepare the patient’s KRT transition and increasing the likelihood of being deprived of a KRTOa, timely vascular access assessment and, consequently, lowering overall kidney care quality.
We would like to point out that this study has some limitations. A retrospective analysis is inherently flawed as it requires the presence of consistent medical records. This limits the inclusion criteria due to lack of digital and physical records in this Nephrology Center before 2010, only allowing the analysis of Nephrology referral after that year.
Another important concern is the attribution of LIs. This process is patient-dependent and it is necessary that patients file for it at the social security services. As discussed before, patients with low SES have less access to information and may lack the initiative to file for LIs.
Finally, the understanding of underprivileged CKD patients as those at higher risk of late referral and, hence, worse outcomes, suggests that our focus and intervention should aim specifically at this factor.
A national coverage of primary care doctors with the appropriate basic education about CKD’s natural evolution, staging and essential steps in proper KRT transition care are key to attenuate these differences.
We also suggest widespread population-based education on the basics of CKD, including diagnosis, as a method to increase patient initiative among low socioeconomic patients in seeking primary care.
CONCLUSION
LIs Portuguese CKD patients are at higher risk of late Nephrology referral and overall worse kidney care, particularly when compared to their non-LIs counterparts. Low eGFR at referral is suggested as the main factor in this difference, leading to shorter time to dialysis, which decreases time for adequate KRT preparation, namely through omission of KRTOa and timely vascular access assessment.
To promote early Nephrology referral, and diminish this difference, we propose increasing primary care awareness for CKD through education for the natural history of this disease, along with the institution of policies that facilitate healthcare access to low socioeconomic stratums. Additionally, widespread population-based education in health is also key to foment individual decision and initiative in healthcare seeking.















