Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Nascer e Crescer
versão impressa ISSN 0872-0754
Nascer e Crescer vol.22 no.3 Porto set. 2013
ARTIGO ORIGINAL / ORIGINAL ARTICLE
Antenatal detection of single umbilical artery: what does it mean?
Deteção pré-natal de artéria umbilical única: qual o seu significado?
Vânia FerreiraI; Inês VazI; Ana Paula ReisI; Maria José MendesI; Maria do Céu RodriguesI
IU. diagnóstico Pré-Natal, S. Obstetrícia, Maternidade Júlio Dinis, CH Porto, 4050-371 Porto, Portugal. vania_ferreira@hotmail.com; inesvaz@hotmail.com; a.paulinha82@gmail.com; mjosemendes688@gmail.com; mcpprodrigues@gmail.com
ABSTRACT
Introduction:The presence of a single umbilical artery (SUA) is recognised as a soft marker for congenital anomalies, aneuploidy, earlier delivery and intra-uterine growth restriction and/or low birth weight. The aim of this study was to assess the incidence of SUA in a selected population. And secondly, to examine the clinical significance of this soft marker.
Material and methods: A retrospective analysis, over a 36-month period, of all cases of pregnancy interruption due to medical causes, up to 16 weeks of gestation, with prenatal diagnosis of SUA; cases of live born with a prenatal diagnosis of SUA or after delivery, at the routine examination of the placenta. Fetal growth and the risk of preterm labor are also to consider in the surveillance of these pregnancies.
Results: Thirty nine cases of SUA were identified during the study period. Incidence of SUA in live born was 0.32% (n=30) and in pregnancy interruption due to medical causes was 12.9% (n=9). The antenatal detection rate was 77%. This ecographic soft marker was an isolated finding in 27 live born (90%). In live born with SUA and associated malformations (13.3%), urinary abnormalities were identified in three cases (75%), and a skeletal with esophageal malformation was identified in one case (25%). Preterm birth occurred in seven cases (23.3%) and birth weight below 10th percentile in four cases (13.3%).
Discussion and conclusions: The presence of SUA in antenatal period should alert the sonographer and clinician for the need of a detailed examination of the fetus to exclude other anomalies. Fetal growth and the risk of preterm labor are also to consider in the surveillance of these pregnancies.
Keywords: Congenital malformation, prenatal diagnosis, single umbilical artery, ultrasonography.
RESUMO
Introdução: A presença de artéria umbilical única (AUU) é um marcador ecográfico associado a malformações, aneuploidias, parto pré-termo e restrição de crescimento intra-uterino e/ou baixo peso ao nascimento. Este estudo tem como objetivo determinar a incidência de AUU numa população selecionada e verificar qual o significado clínico deste marcador ecográfico.
Material e métodos: Análise retrospetiva, durante um período de 36 meses, dos casos de interrupção médica da gravidez, acima das 16 semanas, com diagnóstico pré-natal de AUU; casos de recém-nascidos com diagnóstico pré-natal de AUU ou após o parto, através do exame da placenta.
Resultados: Foram identificados 39 casos de AUU durante o período de estudo. A incidência de AUU nos recém-nascidos e nos casos de interrupção médica da gravidez foi de 0,32% e 12,9%, respetivamente. A taxa de deteção pré-natal foi de 77%. Este achado ecográfico ocorreu isoladamente em 27 casos de recém-nascidos (90%). Nos recém-nascidos com AUU e outras malformações associadas (13,3%), foram identificadas malformações do sistema urinário em três casos (75%) e malformação esquelética associada a malformação esofágica em um caso (25%). Ocorreu parto pré-termo em sete casos (23,3%) e peso ao nascimento abaixo do percentil 10 em quatro casos (13,3%).
Discussão e conclusão: A deteção pré-natal de AUU deve alertar o ecografista e o clínico para o fato do feto necessitar de uma avaliação ecográfica detalhada a fim de excluir outras anomalias. O crescimento fetal e o risco de parto pré-termo, são também de considerar na vigilância destas gestações.
Palavras-chave: Artéria umbilical única, diagnóstico prénatal, ecografia, malformações congénitas.
INTRODUCTION
Single umbilical artery (SUA) is the most common developmental abnormality of the umbilical cord.(1) The incidence of this malformation varies significantly in large series of newborns, though a range of 0.2 to 1.5% is most widely accepted.(2)
The etiopathogenesis, although, not definitively clarified, has been attributed to primary agenesis of umbilical cord, secondary atrophy or atresia of a previously normal umbilical artery or persistence of the original allantoic artery of the body stalk.(3)
A SUA is likely due to secondary atresia or atrophy rather than primary agenesis of the artery. The left umbilical artery is absent more often than the right. One series detected an absent left umbilical artery 73% of the time vs an absent right umbilical artery 27% of the time.(4,5)
The side of absence can be determined by evaluating the umbilical arteries as they course around the fetal urinary bladder laterally. In fact, this is the best place to evaluate these vessels as they may fuse at the region of the umbilical cord insertion into the placenta.(6-8)
There are reports, however, in which two umbilical arteries were seen around the urinary bladder with only a single umbilical artery seen in the free floating cord. In the series by Bornemeier et al this occurred in 14% of their cases.(9)
Although the absence of one umbilical artery was first reported a century ago by Hyrtl(10), the significance of a SUA has only been realized since a retrospective study by Benirschke and Brown(11) showed it was associated with increased incidence of congenital anomalies.
30%-60% of fetuses with single umbilical arteries will have associated anomalies or chromosomal abnormalities.(6,12-19)
Virtually any organ system can be involved with an anomaly in fetuses with a single umbilical artery, however, genitourinary, cardiac and central nervous system abnormalities are the most common.(2,18,20-25)
Although this has not been true at all centers, a study by Abuhamad et al(26) found complex congenital and chromosomal abnormalities exclusively when the left umbilical artery was absent. In a study by Nyberg et al(24), fetuses with a known central nervous system abnormality and a single umbilical artery were found to have a significantly higher frequency of extra-CNS malformations, fetal mortality and chromosomal abnormalities than fetuses with two umbilical arteries.
A SUA in the second trimester of pregnancy has a high association with Trisomy 18, 13, 21 and other chromosomal defects, but all chromosomally abnormal fetuses had associated malformations detected by ultrasound(5).Trisomy 21 is not commonly associated with a single umbilical artery. In addition to malformations and karyotypic abnormalities, infants with a single umbilical artery have an increased incidence of prematurity, low birth weight and intrauterine growth retardation.(2,14,27-32)
The remaining single artery is often quite large approaching the size of the umbilical vein. Sonography is often able to accurately diagnose this condition, especially with the use of colour Doppler flow imaging. There are reports however, of sensitivities and positive predictive accuracies of only 65%. In addition, in one report obstetricians and paediatrician missed the diagnosis at delivery as often as 24% and 16% of cases.(9,25)
With this study we pretend to determine the association between diagnosis of SUA and perinatal outcome (malformations, prematurity, low birth weight, intrauterine growth retardation, delivery type) as well as to determine the clinical significance of antenatal detection of a single umbilical artery.
MATERIAL AND METHODS
For the purpose of this study were considered all cases of pregnancy interruption due to medical cases, up to 16 weeks of gestation, with prenatal diagnosis of SUA; all newborns with prenatal diagnosis of SUA and those who were identified at the routine examination of the placenta after delivery, over a 36 month period.
Pregnancy data (maternal age, parity, gestational age at diagnosis of SUA, adverse pregnancy outcomes, prenatal diagnosis of other anomalies, gestational age at delivery), perinatal outcome (delivery mode, gestation weeks, birthweigth, postnatal anomalies) were reviewed.
A variety of methods, previously described(6-9,25), were employed by different sonographers to detect the presence of a single umbilical artery. In some cases, a free loop of the umbilical cord was viewed in cross-section and the vessels were counted. In other cases, the umbilical cord insertion at the abdominal wall or the umbilical arteries, as they traverse either side of the fetal bladder, was viewed with colour power angiography. The methodology used was not recorded by the sonographer at the time of the examination.
Fetuses were evaluated in posnatal period with transfontanelar ultrasound, echocardiography, and bladder-kidney ultrasound.
The data were analysed in SPSS19.
RESULTS
During the study period there were 9518 fetuses delivered after 24 weeks gestation and 70 pregnancy interruption due to medical causes. 39 cases of SUA were identified, nine from pregnancy interruption and thirty newborns with SUA. The incidence of SUA in live born was 0.32% (n=30) and 12.9% (n=9) in pregnancy interruption due to medical causes.
The presence of only one umbilical artery was detected antenatally in 30 of the 39 cases with SUA, representing a detection rate of 77%. One of the nine cases with a single umbilical artery not recognised antenatally was diagnosed by the routine examination of the placenta after delivery. It was a delivery at 31 weeks and the newborn presented unilateral renal agenesis.
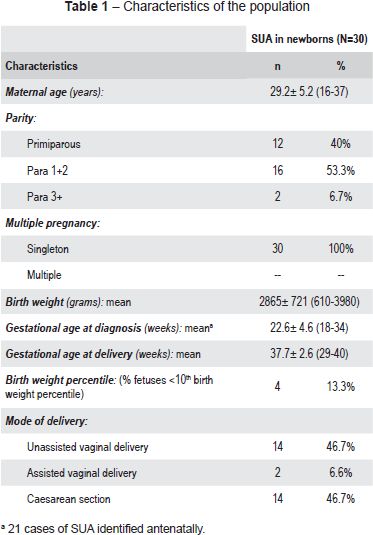
The maternal and pregnancy characteristics of live borne cases with SUA are shown in Table 1.
Of the total cases with SUA detected antenatally, 12 had suspicious malformations associated. Nine of those cases (75%) went to termination of pregnancy and three (25%) were born. Of these three live born, two presented associated malformations and in one case the malformation recognized antenatally was not confirmed in postnatal period. The description of cases with a SUA and other anomaly recognised antenatally are shown in Table 2.
The principal complications of pregnancy were: preeclampsia (one case), oligoamnios (three cases) and intrauterine growth restriction with oligoamnios (four cases).
Preterm birth occurred in seven cases (23.3%) and birth weight below 10th percentile in four cases (13.3%).
Ecocardiography and transfontanelar ultrasound in postnatal period did not revealed alterations. Bladder-kidney ultrasound revealed a horseshoe kidney in one case (recognized in prenatal period) and unilateral renal agenesis de novo (not recognised in prenatal period).
SUA was an isolated finding in 27 liveborns (90%). In live born with SUA and associated malformations (n=4; 13.3%), urinary abnormalities were identified in three cases (75%) and in one case (25%) a skeletal with esophageal malformation was identified.
DISCUSSION
There are two main sources of data on SUA and its association with other abnormalities: 1) abortuses, cases of fetal death, and terminations of aneuploid or anomalous fetuses, and 2) live births(12). The first source of data produces a higher incidence of SUA, as well as more frequent association with structural and genetic abnormalities and perinatal mortality. The second data set suggests a lower incidence and frequency of associated anomalies, as many of the most severely affected infants have aborted or been voluntarily terminated early in pregnancy. A meta analysis of these data highlights the differences: the autopsy data estimate the incidence of single umbilical artery at 0.34-7% and the associated malformations at 0.25-81.8% (generally 20-50%).(15,26,33-35) Live born data estimate the incidence of single umbilical artery at birth at 0.2-1.13% and anomalies at 8.7-66%.(9)
Estimates of the frequency of aneuploid range widely, between 4-50% in cases of SUA with other anomalies.(15-19,26) With isolated SUA, the rate of aneuploidy is not known; however, most authors do not recommend routine karyotype.(15,9,26)
Reports of association between SUA and other anomalies have created an imperative to identify or exclude the presence of such anomalies and detailed sonography is advised for all fetuses with SUA.(15,21,26,27) It is therefore not clear not how a couple with this sonographic finding should be counseled and what further management should be offered.(14)
In our study, we found that a SUA was present in 0.32% of live born and in 12.9% of the cases of interruption of pregnancy due to medical causes. This is similar to published data.(9,12,15,26,33-35)
The antenatal detection rate of a SUA in this population presents a value quite acceptable, with only one-quarter of cases not identified. There are possible explanations for this, including technical difficulties or lack of training; failure by the sonographers to spend much time examining the cord vasculature because of a lack of understanding of the implications of the presence of a SUA and due to the fact that other anomalies are noted with ultrasonography before the presence of a SUA is confirmed and examination of the cord then becomes lower in priority.
The presence of malformations was identified in four cases of live born with SUA (13.3%), which is similar to the published data.(9)
Among the 30 live born with SUA, seven (23,3%) were born before 37 weeks, which means that the proportion of premature infants in this group was twice that in the general institution (11,5%). Four of the 30 live born with SUA were born below tenth percentile, contrastating well with the proportion of live born in global sample (3.92%). These findings were similar to previous reports of an increased risk of prematurity as well as birth weight below the tenth percentile in live born with single umbilical artery.(2,14,27-32) However, future studies with larger number of patients and adequate power analysis are required to confirm this regard.
In this study only one chromosomal abnormality established by fetal karyotyping was found (2,6%) and it occurred in a fetus with multiple malformations, which went to termination of pregnancy.
Our results indicate that the identification of a SUA should be regarded as a significant finding associated with other congenital anomalies and a poorer perinatal outcome. The detection rate, despite having an acceptable value, should be improved. Further training is required together with rising the awareness of the implications of this finding. When identified at a routine antenatal scan, the presence of a SUA should alert the sonographer and clinician of the fact that the fetus requires a more detailed examination to exclude other anomalies. If other anomalies are detected, then the case should be managed according to the type and severity of the abnormalities. Since the presence of a SUA with an associated anomaly carries an aneuploidy risk(5,15-19,26), karyotyping should be advised if another anomaly is detected. However, advice regarding karyotyping in the presence of an isolated SUA is more difficult.
Any advice should be tailored to the particular pregnancy, taking into account other factors such as age, but we would not strongly recommend karyotyping in agreement with other authors.(19,29)
In light of the poorer perinatal outcome in fetuses with an apparently isolated single umbilical artery, further ultrasound scans in the third trimester to examine growth and continuous fetal-heart-rate monitoring during labour should be offered. Parents should be advised of the increased risks associated with the presence of a SUA and the need for extra surveillance, and it may also be advisable to counsel parents of the possibility of an associated abnormality that may only be detectable after delivery.
REFERENCES
1. Peckham CH, Yerushalmy J. Aplasia of one umbilical artery: incidence in race and certain obstetric factors. Obstet Gynecol 1965; 26:359-66. [ Links ]
2. Heifetz SA. Single umbilical artery: a statistical analysis of 237 autopsy cases and review of literature. Perspect Pediatr Pathol 1984; 8:345-78. [ Links ]
3. Persutte WH, Hobbins J. Single umbilical artery: a clinical enigma in modern prenatal diagnosis. Ultrasound Obstet Gynecol 1995; 6:216-29. [ Links ]
4. Bernischke K, Kaufmann P. Pathology of the human placenta. 2nd Ed. New York: Springer-Verlag, 1990. [ Links ]
5. Lubusky M, Dhaifalah I, Prochazka M, Hyjanek J, Mickova I, Vomackova K, et al. Single umbilical artery and its siding in the second trimester of pregnancy: relation to chromosomal defects. Prenat Diagn 2007; 27:327-31. [ Links ]
6. Weissman A, Jakobi P, Bronshtein M, Goldstein I. Sonographic measurements of the umbilical cord and vessels during normal pregnancies. J Ultrasound Med 1994; 13:11-4. [ Links ]
7. Sepulveda W, Peek MJ, Hassan J. Umbilical vein to artery ratio in fetuses with single umbilical artery. Ultrasound Obstet Gynecol 1996; 8:23-6. [ Links ]
8. Persutte WH, Lenke RR. Transverse umbilical arterial diameter: techniques for the prenatal diagnosis of single umbilical artery. J Ultrasound Med 1994; 13:763-6. [ Links ]
9. Bornemeier S, Carpinito LA, Winter TC. Sonographic evaluation of the two vessel umbilical cord: A comparison between umbilical arteries adjacent to the bladder and cross-sections of the umbilical cord. J Diag Med Sono 1996; 12:260-5. [ Links ]
10. Hyrtl J. Die Blutgefässe der menschlichen Nachgeburt in normalen und abnormen Verhältnissen. Vienna: W. Braumüller; 1870. [ Links ]
11. Benirschke K, Brown WH. A vascular anomaly of the umbilical cord; the absence of one umbilical artery in the umbilical cords of normal and abnormal fetuses. Obstet Gynecol 1955; 6:399-404. [ Links ]
12. Thummala MR, Raju TN, Langenberg P. Isolated single umbilical artery anomaly and the risk for congenital malformations: a meta-analysis. J Pediatr Surg 1998; 33:580-5. [ Links ]
13. Abuhamad AZ, Shaffer W, Mari G, Copel JA, Hobbins JC, Evans AT. Umbilical artery: does it matter which side is missing? Am J Obstet Gynecol 1995; 173:728-32. [ Links ]
14. Gornall AS, Kurinczuk JJ, Konje JC. Antenatal detection of a single umbilical artery: does it matter? Prenat Diagn 2003; 23:117-23. [ Links ]
15. Chow JS, Benson CB, Doubilet PM. Frequency and nature of structural anomalies in fetuses with single umbilical arteries. J Ultrasound Med 1998; 17:765-8. [ Links ]
16. Khong TY, George K. Chromosomal abnormalities associated with a single umbilical artery. Prenat Diagn 1992; 12:965-8. [ Links ]
17. Saller DN, Keene CL, Sun CJ, Schwartz S. The association of single umbilical artery with cytogenetically abnormal pregnancies. Am J Obstet Gynecol 1990; 163:922-5. [ Links ]
18. Nyberg DA, Mahony BS, Luthy D, Kapur R. Single umbilical artery: prenatal detection of concurrent anomalies. J Ultrasound Med 1991; 10:247-53. [ Links ]
19. Parilla BV, Tamura RK, MacGregor SN, Geibel LJ, Sabbagha RE. The clinical significance of a single umbilical artery as an isolated finding on prenatal ultrasound. Obstet Gynecol 1995; 85:570-2. [ Links ]
20. Byrne J, Blanc WA. Malformations and chromosome anomalies in spontaneously aborted fetuses with single umbilical artery. Am J Obstet Gynecol 1985; 151:340-2. [ Links ]
21. Jones TB, Sorokin Y, Bhatia R, Zador IE, Bottoms SF. Single umbilical artery: accurate diagnosis? Am J Obstet Gynecol 1993; 169:538-40. [ Links ]
22. Froehlich LA, Fujikura T. Follow-up of infants with single umbilical artery. Pediatrics 1973; 52:22-9. [ Links ]
23. Benirschke K, Bourne GL. The incidence and prognostic implication of congenital absence of one umbilical artery. Am J Obstet Gynecol 1960; 79:251-4. [ Links ]
24. Nyberg DA, Shepard T, Mack LA, Hirsh J, Luthy D, Fitzsimmons J. Significance of a single umbilical artery in fetuses with central nervous system malformations. J Ultrasound Med 1988; 7:265-73. [ Links ]
25. Jeanty P. Fetal and funicular vascular anomalies: identification with prenatal ultrasound. Radiology 1989; 173:367-70. [ Links ]
26. Abuhamdad AZ, Shaffer W, Mari G, Copel JA, Hobbns JC, Evans AT. Single umbilical artery: does it matter which artery is missing? Am J Obstet Gynecol 1995; 173:728-32. [ Links ]
27. Catanzarite VA. The clinical significance of a single umbilical artery as an isolated finding of prenatal ultrasound. Obstet Gynecol 1995;86:155-6. [ Links ]
28. Farrel T, Leslie J, Owen P. Accuracy and significance of prenatal diagnosis of single umbilical artery. Ultrasound Obstet Gynecol 2000; 16:667-8. [ Links ]
29. Geipel A, Germer U, Welp T, Schwimger E, Gembruch U. Prenatal diagnosis of single umbilical artery: determination of the absent side, associated anomalies, Doppler findings and perinatal outcome. Ultrasound Obstet Gynecol 2000; 15:114-17. [ Links ]
30. Volpe G, Volpe P, Boscia FM, Volpe N, Buonadonna AL, Gentile M. Isolated single umbilical artery: incidence, cytogenetic abnormalities, malformation and perinatal outcome. Minerva Ginecol 2005; 57:189-98. [ Links ]
31. Lacro RV, Jones KL, Benirschke K. The umbilical cord twist: origin, direction, and relevance. Am J Obstet Gynecol 1987; 157:833-8. [ Links ]
32. Raio L, Ghezzi F, Di Naro E, Franchi M, Brühwiler H, Lüscher KP. Prenatal assessment of Whartons jelly in umbilical cords with single artery. Ultrasound Obstet and Gynecol 1999; 14:42-6. [ Links ]
33. Leung AK, Robson WL. Single umbilical artery: a report of 159 cases. Am J Dis Child 1989; 143:108-11. [ Links ]
34. Tortora M, Chevernak FA, Mayden K, Hobbins JC. Antenatal sonographic diagnosis of single umbilical artery. Obstet Gynecol 1984; 63:693-6. [ Links ]
35. Gosset DR, Lantz ME, Chisholm CA. Antenatal diagnosis of single umbilical artery: is fetal echocardiography warranted. Obstet Gynecol 2002; 100:903-8. [ Links ]
Vânia Gisela Costa Arcanjo Ferreira
Centro Hospitalar do Porto – Maternidade Júlio Dinis
Serviço de Obstetrícia – Unidade de Diagnóstico Pré-Natal
Largo da Maternidade Júlio Dinis
4050-371 Porto, Portugal
E-mail: vania_ferreira@hotmail.com
Recebido a 14.05.2013 | Aceite a 25.08.2013














