Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Nascer e Crescer
versão impressa ISSN 0872-0754
Nascer e Crescer vol.23 no.3 Porto set. 2014
ARTIGO ORIGINAL / ORIGINAL ARTICLE
Oesophageal atresia: a 10-year experience of a Paediatric Intensive Care Unit
Atrésia esofágica: 10 anos de experiência de um serviço de cuidados intensivos pediátricos
Liliana PinhoI; Maristela MargathoI; Andrea DiasI; Carla PintoI; Maria Francelina LopesII; Farela NevesI
IS. Cuidados Intensivos Pediátricos, H Pediátrico Carmona da Mota, CH e Universitário de Coimbra. 3000-602 Coimbra, Portugal. E-mail: liliana.pinho@gmail.com; margatho1979@gmail.com; sofia.andrea@gmail.com; carla.regina.pinto@gmail.com; farela@chc.min-saude.pt
IS. Cirurgia Pediátrica, H Pediátrico Carmona da Mota, CH e Universitário de Coimbra, 3000-602 Coimbra, Portugal. E-mail: mfrancelina@yahoo.com
ABSTRACT
Background/Purpose: Oesophageal atresia (OA) is a congenital malformation with a variable prognosis. The aims were to establish OA’s incidence in the central region, to characterize infants with OA admitted and to compare its clinical outcome after surgical repair, according to OA classification.
Methods: A retrospective review of infants with OA admitted to a PICU, after surgical repair, between 2002 and 2011. Patient characteristics, OA’s classification, surgery, morbidity and mortality were analyzed. Two groups were compared according to OA classification.
Results: Thirty-four infants were admitted, out of which 65% were male, with a median gestational age of 36 weeks and birth weight of 2310g. Nineteen of them presented other malformations, mainly cardiac. Nine cases were classified as long-gap OA. Fistula ligation and primary oesophageal anastomosis was the most common surgical option (n=27). Early complications occurred in 13 infants (38%), mostly anastomotic leak, and were similar according to gap length (p=0.704). PICU stay and mechanical ventilation were longer in long-gap OA patients (p=0.009 and p<0.001 respectively) and in infants with other malformations (p=0.027 and p=0.003 respectively). There was no mortality.
Conclusions: The frequency of OA associated malformations implies a systematic screening of these patients. Gap length and presence of associated malformations were the major determinants of length of intensive care stay and ventilation days in OA patients.
Key-words: Complications, oesophageal atresia, outcome, surgery.
RESUMO
Introdução/Objetivos: A atrésia esofágica (AE) é uma malformação congénita com prognóstico variável. Os objetivos do estudo foram estabelecer a incidência de AE na região centro, caracterizar os lactentes com AE admitidos e comparar a evolução após cirurgia, atendendo ao tipo de AE.
Métodos: Estudo descritivo com colheita retrospetiva de dados dos lactentes admitidos no Serviço de Cuidados Intensivos (CIPE) no pós-operatório de AE, entre 2002 e 2011. Foram analisados os seguintes parâmetros: características dos doentes, classificação da AE, tipo de cirurgia, morbilidade e mortalidade. Comparação dos dois grupos de acordo com a classificação da AE.
Resultados: Foram admitidas 34 crianças, 65% do sexo masculino. A mediana da idade gestacional foi 36 semanas e do peso ao nascer 2310g. Foram detetadas malformações associadas em 19 crianças, sobretudo cardíacas. Nove casos foram classificados como hiato longo (HL). A opção cirúrgica mais frequente foi laqueação de fístula e esófago-esofagostomia primária (n=27). Registaram-se complicações precoces em 13 lactentes (38%), sobretudo deiscência da anastomose, não se registando diferença em relação ao tamanho do hiato (p=0.704). A duração do internamento em cuidados intensivos e o tempo de ventilação mecânica foram superiores nas situações de HL (p=0.009 e p<0.001 respetivamente) e na presença de malformações associadas (p=0.027 e p=0.003 respetivamente). Não se registaram óbitos.
Conclusões: A frequência de malformações associadas obriga a um rastreio sistemático. A presença de HL e malformações associadas foram os principais determinantes da duração de internamento em cuidados intensivos e do período de ventilação mecânica nos doentes com AE.
Palavras-chave: Atrésia esofágica, cirurgia, complicações, evolução.
BACKGROUND
Oesophageal atresia (OA) is a congenital anomaly that occurs in approximately 1 in 2500 to 4500 live births. It is characterized by complete interruption in the continuity of the oesophageal lumen which is usually associated to a persistent communication with the trachea(1-3).
Its etiology is thought to be complex and multifactorial with involvement of both genetic and environmental factors. In a small percentage of patients (6-10%), a well-defi genetic syndrome can be diagnosed, leaving the majority of cases with unknown cause. There are associated anomalies in half of the cases, often as part of the VACTERL association (vertebral, anorectal, cardiac, tracheo-oesophageal, renal and limb defects)(4,5).
OA is generally classified according to its anatomic configuration (Gross, 1953): type A – isolated OA without fistula, type B – OA with proximal tracheo-oesophageal fistula (TOF), type C – OA with distal TOF, type D – OA with proximal and distal TOF and type E – isolated fistula without atresia (or H-type). Almost all cases correspond to type C OA(3).
The diagnosis of OA may be suspected around the 18th week of gestation, based on the presence of polyhydramnios associated with a small or absent stomach on fetal ultrasound. Infants with OA become symptomatic soon after birth with feeding difficulties, drooling, choking and respiratory distress. If present, a distal TOF may lead to gastric distension. Aspiration pneumonia may result from gastric content reflux and contributes to morbidity. The diagnosis can be made by attempting to insert a gastric tube into the stomach that will not pass beyond 10-15 cm from the lips. Chest radiography will confirm this diagnosis by demonstrating the tube curled in the upper oesophageal pouch. If TOF is present, the radiograph film reveals a gas-filled gastrointestinal tract(1,3).
Survival with OA is only possible with surgical correction which consists in anastomosis of the oesophageal segments and fistula ligation when a TOF is present. Primary repair is generally not possible in long-gap OA which is usually defined by a gap greater than 2 cm or 2-3 vertebral bodies between the two oesophageal pouches(1,6-8).
Outcome depends mainly upon associated anomalies. Birth weight and OA gap length also may determine the prognosis. The Spitz classification for survival in OA is based on birth weight and presence of cardiac defects which were identified as the main responsible for the mortality (group I: birth weight over 1500g without major cardiac defect defined as either cyanotic congenital heart disease that required palliative or corrective
METHODS
A longitudinal observational study from newborns with OA admitted to a PICU of a tertiary care Portuguese Pediatric Hospital between 2002 and 2011 (10 years) was performed. This hospital is the reference for all paediatric surgical patients from central region of Portugal. Patients with isolated TOF (type E or H-type TOF) were not included in this study.
Data collection was retrospective, through consultation of clinical files and PICU database. Data items included in this analysis were: prenatal evaluation, gender, gestational age and birth weight, age at diagnosis, associated malformations, type of corrective surgery, age at corrective surgery, presence of anastomotic tension, length of ventilation after surgery and length of PICU stay. Early complications during PICU stay, after corrective surgery, were also recorded. Gastroesophageal reflux was not considered as an early complication because it is usually associated with OA.
OA was classified according to gap length (long and nonlong) and Gross classification (types A, B, C and D; H-type was not considered in the scope of this study). Since there is no precise definition of long-gap OA, in this study, it was defined as a distance greater than 2 cm or 2-3 vertebral bodies between the two oesophageal ends. We did not distinguish between longgap and ultra-long gap. Non long-gap includes OA with short and intermediate gap. Patients were classified according to the risk categorization and prognosis using the Spitz classification. Sepsis was defined according to International Pediatric Sepsis Consensus Conference(10).
Statistical analysis was carried out with SPSS® version
19.0. It included descriptive statistics with absolute and relative frequencies and central trend and dispersion measures. Length of PICU stay, duration of ventilation after surgery and complications according to different OA classification systems were compared through the application of adequate statistical tests (Mann-Whitney U test for quantitative variables; chisquare and Fisher exact test for qualitative variables). Statistical significance was assigned to a p value < 0.05 with a confidence interval of 95%.
RESULTS
Between 2002 and 2011, thirty-four infants with OA were included. According to data collected in the study, during this period, the incidence of OA in the central region of Portugal was 1.8 in 10000 live births. The terminated pregnancies were not included. Twenty two (65%) infants were male. The median gestational age was 36 weeks (P25: 33.75; P75: 38) and 19 (56%) infants were preterm (<37 weeks of gestation). The median birth weight was 2310g (P25: 1740; P75: 2691) with 21 (62%) low-birthweight newborns (< 2500g) and 5 (15%) very-low-birth-weight newborns (<1500g). OA was suspected in 7 (21%) infants based on antenatal ultrasound. Definitive diagnosis was made in the first day of life in 29 (85%) infants, in the second in 3 (9%) and in the third in 2 (6%). All patients underwent echocardiography before surgery. Nineteen infants (56%) presented congenital malformations other than OA. Cardiovascular defects were the most frequent associated malformations (n= 12), followed by anorectal (n=4), vertebral (n=3) and renal defects (n=2). Five infants (15%) met diagnostic criteria for VACTERL association. Chromosomal abnormalities were detected in 2 of the 9 patients (22%) who underwent karyotype analysis (deletion 11q; partial monosomy 2q and partial trisomy 3p).
Most of the patients (n=27; 79%) were classified in group I of Spitz classification, while the remaining seven were included in group II.
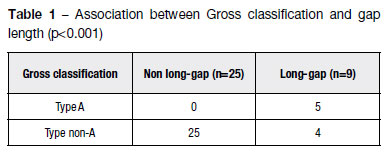
According to the Gross classification the patients on this study were classified in three types of OA: 5 (15%) were type A, 27 (79%) were type C and 2 (6%) were type D. There were 9 cases of long-gap OA (26%). OA other type than A were mostly non long-gap (p<0,001) (Table 1).
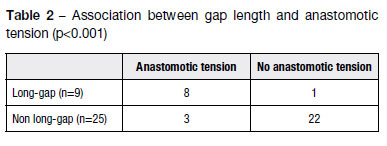
Until surgical correction a Replogle® suction tube was placed. Fistula ligation and primary oesophageal anastomosis was the most frequent surgical option (n=27), followed by Foker procedure with delayed oesophageal anastomosis (n=4) and delayed oesophageal anastomosis with no previous Foker (n=3). All patients were submitted to an open repair through thoracotomy and extrapleural was the preferred surgical approach. Median age at corrective surgery was 1.5 days (P25: 1; P75: 4). Surgical repair was performed earlier in patients with non long-gap OA with a median of 1 day in this group (minimum 1; maximum 4 days) vs. a median of 105 days in long-gap OA (minimum 1, maximum 165 days), p=0.002. Anastomotic tension was described in 11 patients (32%), more often in long-gap OA group (89% patients with long-gap OA vs. 12% patients with non long-gap OA, p <0.001) (Table 2).
The median length of ventilation after surgery was 4 days (P25: 2; P75: 5), being longer in long-gap OA patients (2 days in non long-gap OA vs. 7 days in long-gap OA, p<0.001), in cases with anastomotic tension (6 days in the presence of anastomotic tension vs. 2 days when anastomotic tension was not present, p<0.001) and in infants with associated malformations (2 days in patients without other defects vs. 4 days when other malformations were present, p=0.003).
Early postoperative complications occurred in 13 patients (38%). The most frequent were anastomotic leak (n=8) followed by sepsis (n=5) and pneumothorax (n=5). Table 3 shows each early complication distribution in non long-gap and long-gap OA patients. Early complications were slightly more common in longgap OA patients: 4 of the long-gap OA patients (44%) presented early complications, while 9 of the non long-gap OA patients (36%) suffered from this type of complication, however this association failed to achieve statistical significance (p=0.704).
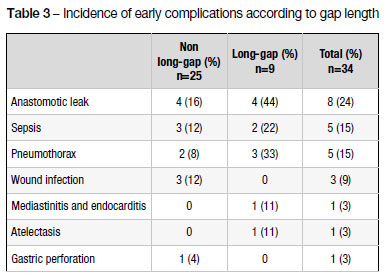
The proportion of early complications was similar in both groups of Spitz’s classification (41% in group I vs. 29% in group II, p=0,682) and was not related with the presence of other malformations (42% when other malformations were present vs. 33% in patients without other defects, p=0.601). The median of PICU length of stay was 12 days (P25: 1; P75: 81), being longer in long-gap OA patients (10 days in non longgap OA vs. 23 days in long-gap OA, p=0.008) and in infants with associated malformations (10.5 days in patients without other defects vs. 15 days when other malformations were present; p=0.027). Birth weight and gestational age were not associated with PICU length of stay. There was no mortality during PICU stay.
DISCUSSION
Between 2002 and 2011, the incidence of OA in the Central Region of Portugal was 1.8 in 10000 live births, lower than the overall incidence recently reported by EUROCAT in 23 European regions (2.43 in 10000 live births). It could be related to the small size of our sample that represents only the central region of Portugal. In our study, there was a male predominance which was also shown by EUROCAT Working Group(6). There is no apparent explanation for this, but a similar pattern is also seen in other congenital anomalies(11). More than half of the patients were preterm, what could be related to the associated polyhydramnios.
Less than a quarter of the cases had a prenatal diagnosis. The diagnosis of oesophageal atresia may be suspected prenatally by the finding of a small or absent stomach bubble on ultrasound. In combination with polyhydramnios the sensitivity is higher, but isolated polyhydramnios is a weak signal for OA. Given this, the accuracy of antenatal ultrasound appears to be greater in isolated OA(3), what could explain the low prenatal detection rate verified in our study with a predominance of OA with TOF. Nevertheless, an early postnatal diagnosis, in the first 72 hours of life, was made in all cases. An attempt to introduce a gastric tube immediately after birth might be made if any antenatal suspicion was present.
As described in literature, additional malformations were detected in more than half of the cases, mostly cardiac defects. As recommended, all patients had an echocardiogram prior to surgery. Besides allowing detection of a cardiac defect that may need intervention, the echocardiogram also defines any structural anomaly of the heart or great blood vessels like a right-sided aortic arch which determinates the side for surgical approach(1,3). Some authors recommend performing a preoperative bronchoscopy to exclude an upper pouch fistula which is 3-4 times more common in the gasless abdomen OA(3).
Type C OA was the most common, followed by type A, which is in agreement with literature(12,13). We found an association between isolated OA and presence of a long-gap which may alert physicians at the time of diagnosis: when the radiography fi does not reveal a gas-fi gastrointestinal tract, there is a high probability of being a type A and as consequence a longgap OA.
Primary oesophageal anastomosis with fistula ligation was the most common surgical option, reflecting the higher prevalence of type C and non long-gap OA. Long-gap OA correction is a major surgical and medical challenge and there are many treatment options described in literature. In this study, delayed oesophageal anastomosis was often preceded by Foker procedure (application of graduated tension on the oesophageal ends)(1,3,8,14,15). Consequently, the age at corrective surgery was different according to gap length and it was lower in the group of non long-gap OA. As we report, a primary surgical repair in neonatal period is possible in the majority of patients with type C OA, including the ones with long-gap OA. In opposition to that, primary anastomosis in neonatal period is exceptional in type A OA. In our study, only one type A OA was submitted to a primary repair, but after an awaiting period of time.
Median length of ventilation after surgery was higher in longgap OA patients, which was related to an higher frequency of anastomotic tension in this group. The gap between the two ends of the oesophagus is a critical factor in determining tension at the anastomotic point as it has been shown in some studies(16). When the oesophageal anastomosis is performed under tension, many centers recommend that the infant should be electively paralyzed and mechanically ventilated for a variable period of time(3). According to our experience, this time should be as shorter as possible in order to protect both, the anastomosis and the lung.
Early postoperative complications were common, especially anastomotic leak, sepsis and pneumothorax, what may reflect the complexity of the surgery performed. The Spitz classification has proved to be a useful tool in determining long-term outcome(3), but it seems not to influence the risk of early complications in our study. Shortly after corrective surgery, gap length and associated malformations seemed to be a better predictor of PICU length of stay than the Spitz classification, probably due to improvement of care of low birth weight neonates. Our study failed to achieve statistically significant difference in occurrence of early complications according to gap length. Recently, other authors concluded that long-gap was a major predictor of post-repair complications(13). It should be noted that this is a retrospective study, with its subjacent limitations, and the sample is small. Nevertheless, as far as we know, it is the first analysis on the outcome of OA patients during PICU stay.
Low mortality rates were also recently reported by other studies that considered a longer period follow-up.(12,13)
In conclusion, the frequency of OA associated malformations implies a systematic screening of these patients. Gap length and the presence of associated malformations were the major determinants of PICU length of stay and ventilation in OA patients, in our study.
REFERENCES
1. Holland AJA, Fitzgerald DA. Oesophageal atresia and trachea-oesophageal fistula: current management strategies and complications. Paediatric Respiratory Reviews 2010; 11:100-7. [ Links ]
2. Kovesi T, Rubin S. Long-term complications of congenital oesophageal atresia and/or tracheo-oesophageal fistula. Chest 2004; 126:915-25. [ Links ]
3. Spitz L. Oesophageal atresia. Orphanet J Rare Dis 2007; 2:24. [ Links ]
4. Jong EM, Felix JF, Klein A, Tibboel D. Etiology of oesophageal atresia and tracheooesophageal fistula: mind the gap. Curr Gastroenterol Rep 2010; 12:215-22. [ Links ]
5. Solomon BD. VACTERL/VATER association. Orphanet J Rare Dis 2011; 6:56. [ Links ]
6. Pedersen RN, Calzolari E, Husby S, Garne E; EUROCAT Working group. Oesophageal atresia: prevalence, prenatal diagnosis and associated anomalies in 23 European regions. Arch Dis Child 2012; 97:227-32. [ Links ]
7. Aslanabadi S, Ghabili K, Rouzrokh M, Hosseini MB, Jamshidi M, Adi FH, et al. Associated congenital anomalies between neonates with short-gap and long-gap oesophageal atresia: a comparative study. Int J Gen Med 2011; 4:487-91. [ Links ]
8. Hunter CJ, Petrosyan M, Connelly ME, Ford Hr, Nguyen NX. Repair of long-gap oesophageal atresia: gastric conduits may improve outcome – a 20-year single center experience. Pediatr Surg Int 2009; 25:1087-91. [ Links ]
9. Driver CP, Shankar KR, Jones MO, Lamont GA, Turnock RR, Lloyd DA, et al. Phenotypic presentation and outcome of oesophageal atresia in the era of the Spitz classification. J Pediatr Surg 2001; 36:1419-21. [ Links ]
10. Goldstein B, Giroir B, Randolph A. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med 2005; 6:2-8. [ Links ]
11. Krogh C, Gørtz S, Wohlfahrt J, Biggar RJ, Melbye M, Fischer TK. Pre and perinatal risk factors for pyloric stenosis and their influence on the male predominance. Am J Epidemiol 2012; 176:24-31. [ Links ]
12. Burge DM, Shah K, Spark P, Shenker N, Pierce M, Kurinczuk JJ, et al. Contemporary management and outcomes for infants born with oesophageal atresia. Br J Surg 2013; 100:515-21. [ Links ]
13. Koivusalo AI, Pakarinen MP, Rintala RJ. Modern outcomes of oesophageal atresia: Single centre experience over the last twenty years. J Pediatr Surg 2013; 48:297-303. [ Links ]
14. Lopes MF, Botelho MF. Midterm follow-up of esophageal anastomosis for esophageal atresia repair: long-gap versus non long-gap. Dis Esophagus 2007; 20:428-35. [ Links ]
15. Lopes MF, Reis A, Coutinho S, Pires A. Very long gap esophageal atresia successfully treated by esophageal lengthening using external traction sutures. J Pediatr Surg 2004; 39:1286-7. [ Links ]
16. Mansur SH, Talat N, Ahmed S. Oesophageal atresia: role of gap length in determining the outcome. Biomedica 2005; 21:125-8. [ Links ]
Correspondence to
Andrea Dias
Serviço de Cuidados Intensivos Pediátricos
Hospital Pediátrico Carmona da Mota
Av. Afonso Romão, Santo António dos Olivais
3000-602 Coimbra, Portugal
E-mail: sofia.andrea@gmail.com
Recebido a 03.02.2014 | Aceite a 10.04.2014














