Serviços Personalizados
Journal
Artigo
Indicadores
Links relacionados
Compartilhar
Nascer e Crescer
versão impressa ISSN 0872-0754versão On-line ISSN 2183-9417
Nascer e Crescer vol.26 no.4 Porto 2017
CASE REPORTS | CASOS CLÍNICOS
Lumbar tattoo and labour analgesia: a case of surgical approach
Tatuagem lombar e analgesia de trabalho de parto: um caso de abordagem cirúrgica
Mélanie DuqueI, José LopesI, Sandy RibeiroI, Isabel AraújoI
I Department of Anesthesiology, Hospital de São Teotónio, Centro Hospitalar Tondela-Viseu. 3504-509 Viseu, Portugal. melanieduque@gmail.com; jduartecl@gmail.com; sandy.ribeiro@sapo.pt; isabelguedesaraujo@hotmail.com
ABSTRACT
Introduction: Pregnant women with lumbar tattoo presenting for labour analgesia are currently increasing in number. Many anaesthesiologists are hesitant in placing an epidural catheter over a lumbar tattoo based on a theory that tissue coring of fragments of tattoo pigment into the epidural, subdural or subarachnoid space, could lead to epidermoid tumours or arachnoiditis. For these reasons, it has been recommended to avoid the introduction of epidural needle directly through skin with tattoo pigments.
Case Report: We describe a case where the placement of the epidural catheter was made after a surgical incision of the skin to obtain a puncture field free from ink pigment.
Conclusion: Surgical approach to epidural catheter placement reduces the risk of the pigment-entrainment phenomenon from the skin to the epidural space.
Keywords: Epidural; pregnant; skin incision; tattoo
RESUMO
Introdução: As mulheres grávidas para analgesia de parto com tatuagem lombar estão atualmente a aumentar em número. Muitos anestesistas são hesitantes em colocar um cateter epidural através da tatuagem lombar com base na teoria de arrastamento de tecidos e fragmentos de pigmento da tatuagem para o espaço epidural, subdural ou subaracnóide. Este arrastamento pode levar ao desenvolvimento de tumores epidermóide ou aracnoidites. Por estas razões, tem sido recomendado evitar a introdução de agulha epidural diretamente através da pele com pigmentos de tatuagem.
Relato de Caso: Descrevemos um caso em que a colocação do cateter epidural foi feita após uma incisão cirúrgica na pele para obter um campo de punção livre de pigmento de tinta da tatuagem.
Conclusão: A abordagem cirúrgica para a colocação do cateter epidural reduz o risco de arrastamento do pigmento da pele para o espaço epidural.
Palavras-chave: Epidural; grávida; incisão da pele; tatuagem
INTRODUCTION
Pregnant women with lumbar tattoo presenting for labour analgesia are currently increasing in number.1 This is mainly due to the fact that the group with the highest percentage of individuals having a tattoo was born between 1977 and 1986 and about one third of the individuals with any form of body art (tattoos or piercings) are women.2 Epidural is the gold standard technique for labour analgesia.3 Many anaesthesiologists are hesitant in placing an epidural catheter over a lumbar tattoo based on a theory that tissue coring of fragments of tattoo pigment into the epidural, subdural or subarachnoid space, could lead to epidermoid tumours or arachnoiditis.4-6
A Medline search of English literature using the key words: spinal, epidural, tattoos, tattooing, skin incision, did not find any reports describing the execution of neuroaxial anaesthesia through a skin incision in tattooed areas. We present a case report where the placement of the epidural catheter was made after a surgical incision of the skin to obtain a puncture field free from ink pigment.
CASE DESCRIPTION
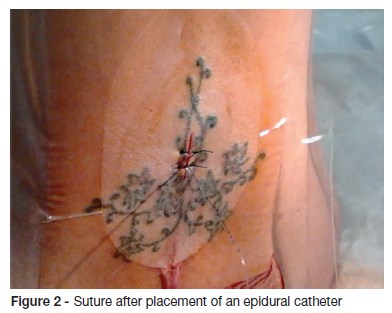
A 26-year-old woman, ASA physical status II, 39 weeks into her first pregnancy, entered our hospital in active phase of labour. She had a lower back midline tattoo extending from L1 to L5. The woman requested epidural analgesia and refused alternative methods of analgesia like intravenous remifentanil. In face of that, a surgical skin incision for placement of the epidural catheter was proposed, to which the pregnant woman consented. The lumbar intervertebral space between L3 and L4 was selected and anaesthesia of the skin of this area was obtained with EMLA® Cream (lidocaine 2.5% and prilocaine 2.5%). After aseptic measures recommended for epidural technique, a vertical midline incision, about two centimetres long, was made using a scalpel blade over the level of the L3 - L4 intervertebral space until the first muscle-ligament plane was reached. No major bleeding occurred. The Tuohy needle (18 Gauge, eight centimetres long) was introduced directly into the interspinous ligaments without contacting with the dermis, and the epidural space was searched by the loss of resistance to air technique. Loss of resistance occurred at a depth of seven centimetres and the catheter was introduced cephalad until the 11 centimetres mark, leaving four centimetres of catheter in the epidural space. (Figure 1 and 2) Simple interrupted suture with instrument tie was performed using a 2-0 silk filament and the LOCKIT Plus® epidural catheter securement device was fixed directly over the suture. Epidural analgesia was effective throughout labour. The catheter was removed the same day after delivery without complications by simply pulling the catheter without removing the skin suture. At discharge date, 48 hours after delivery, the scar showed good evolution: close borders without signs of infection or haemorrhage. The patient was satisfied with the procedure. Thirty days after de delivery, the patient was examined; the scar was healed without colloid formation.

DISCUSSION
The placement of an epidural catheter through a tattoo is a controversial topic. In our country, Portugal, a survey was conducted to investigate anaesthesiologists behaviour when faced with a patient, for possible neuroaxial block, with a lumbar tattoo. This study was published on 2010. Of the 162 anaesthesiologists responding to the survey, 92 (59,8%)had already been requested to carry out a neuroaxial block on a patient with midline back tattoo. Of these, 55 executed the neuroaxial block on pigment-free skin and 6 (6,5%) always refuse to place an epidural catheter in these patients. Of the 70 respondents that had never been confronted with this situation, 25,7% said they would refuse to perform this technique and 67,2% would prefer to perform a neuroaxial block through tattoo free skin, as they were not sure what the effects of the ink pigment would be when dragged into the spinal canal.4 The coring and deposition of tattoo-ink pigment into epidural space is the main issue of concern claimed by anaesthesiologists who avoid inserting epidural catheters in patients with back tattoos.5,6 These concerns were mainly raised by Douglas and Swenerton based on a theory that tissue coring of fragments of tattoo pigment into the epidural, subdural or subarachnoid space, could lead to epidermoid tumours or arachnoiditis.7 Hollow needles, with or without a stylet, entrap tissue fragments (cores) in their bore as they pass to deeper structures and the injection through these needles may then result in this entrapped tissue being deposited in the deeper site.7 Ferraz IL. et al demonstrated, in a study in rabbits, that intrathecal insertion of a puncture needle through tattooed skin produced histological changes in the meninges, and that these changes were not prevented by the use of needles with stylet.8 Although a direct relationship between tattoo ink pigments and epidermoid tumours or chemical arachnoiditis in humans has not been proven, many anaesthesiologists are reluctant because there is still a remote possibility of the development of these serious long-term complications. There is still no evidence-based guideline that excludes the possibility of developing long-term epidural complications by the entrainment of tattoo pigment from the dermis to the epidural space.9
For these reasons, it is suggested to avoid the introduction of epidural needle directly through skin with tattoo pigments by either selecting a tattoo-free intervertebral space, using a paramedian approach, or by finding a pigment-free skin spot within the area of the tattoo.9,10
However, the latter does not assure the absence of ink pigments because they are taken by macrophages from other areas far from the visible limits of the tattoo.7
Epidural is the gold standard technique for labour analgesia with excellent pain relief, delivering higher maternal satisfaction compared with other techniques of pain relief.3 However, because of our patients midline lumbar tattoo, we proposed an intravenous perfusion of remifentanil as alternative analgesia but she refused and insisted on the epidural. After explaining all the possible risks, we proceeded with an epidural block for analgesia. Surgical incision for placement of epidural has already been proposed as a possible technique but, to our knowledge, has not yet been described in the literature.4,6,11 With the skin incision, the authors aimed to reduce the tissue-coring phenomenon of tattoo-ink pigment into the epidural space. During the tattooing process, tattoo pigments are deposited along the entire needle tract but only the pigment that is in the dermis remains permanently since the epidermis undergoes constant regeneration. The surrounding macrophages phagocyte these pigments and carry them to regional lymphatic and perivascular lymph nodes.7 A report of axillary lymphadenopathy clinically mimicking metastatic melanoma 30 years after a decorative tattoo was described. Microscopic examination of the routine haematoxylin and eosin sections of the lymph node of this patient showed tattoo pigment lying within the macrophages and dispersed outside them in the sinuses.12 To this moment tattoo inks are not regulated by a health organism like the Food and Drug Administration or the Infarmed, so the risk of using non identified toxic pigments that could lead to major complications exists. The authors chose not to consider the placement of the epidural on a pigment free skin spot within the area of the tattoo because of the risk of pigment ink migration and decided to perform a skin incision until the muscle-ligament plane was reached.
Although surgical approach to epidural catheter placement is an invasive procedure with possible complications associated, it seems to be a legitimate alternative since it reduces the risk of the pigment-entrainment phenomenon from the skin to the epidural space.
REFERÊNCIAS BIBLIOGRÁFICAS
1. Kluger N. Body art and pregnancy. Eur J Obstet Gynecol Reprod Biol. 2010; 153: 3-7. [ Links ]
2. Laumann AE, Derick AJ. Tattoos and body piercings in the United States: a national data set. J Am Acad Dermatol 2006; 55:413–21. [ Links ]
3. Sng BL, Kwok SC, Sia AT. Modern neuraxial labour analgesia. Curr Opin Anaesthesiol. 2015; 28:285-9. [ Links ]
4. Gaspar A, Serrano N. Neuroaxial blocks and tattoos: a dilemma? Arch Gynecol Obstet. 2010; 282:255–60. [ Links ]
5. Sleth JC, Guillot B, Kluger N. Lumbar tattoos and neuraxial anaesthesia in obstetrics: practice survey in Languedoc-Roussillon, France. Ann Fr Anesth Reanim. 2010; 29:397–401. [ Links ]
6. Raynaud L, Mercier FJ, Auroy Y, Benhamou D; SOS ALR. Epidural anaesthesia and lumbar tattoo: what to do? Ann Fr Anesth Reanim. 2006; 25:71-3. [ Links ]
7. Douglas M J, Swenerton J E. Epidural anesthesia in three parturients with lumbar tattoos: A review of possible implications. Can J Anesth 2002; 49:1057–60. [ Links ]
8. Ferraz IL, GA Barros Ferreira Neto PG, et al. Does Spinal Block Through Tattooed Skin Cause Histological Changes in Nervous Tissue and Meninges?: An Experimental Model in Rabbits. Reg Anesth Pain Med 2015; 40:533-8. [ Links ]
9. Welliver D, Welliver M, Carroll T, James P. Lumbar epidural catheter placement in the presence of low back tattoos: a review of the safety concerns. AANA J. 2010; 78:197–201. [ Links ]
10. Mercier FJ, Bonnet MP. Tattooing and various piercing: anaesthetic considerations. Curr Opin Anaesthesiol. 2009; 22:436-41. [ Links ]
11. Aguilar Godoy J, Alonso Chico A, González Zarco LM, Ruiz Uchupi P. Comment on the letter Spinal anesthesia and tattos. Rev Esp Anestesiol Reanim. 2004; 51:412-3. [ Links ]
12. Jack CM, Adwani A, Krishnan H. Tattoo pigment in an axillary lymph node simulating metastatic malignant melanoma. Int Semin Surg Oncol. 2005; 2:28. [ Links ]
CORRESPONDENCE TO
Mélanie Duque
Department of Anesthesiology
Hospital de São Teotónio
Centro Hospitalar Tondela-Viseu
Avenida Rei D. Duarte
3504-509 Viseu
Email: melanieduque@gmail.com
Received for publication: 13.08.2016 Accepted in revised form: 02.03.2017














