Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Nascer e Crescer
versão impressa ISSN 0872-0754versão On-line ISSN 2183-9417
Nascer e Crescer vol.27 no.2 Porto jun. 2018
CASE REPORTS | CASOS CLÍNICOS
Uncommon Pathogens Causing an Infrequent Disease - Two cases of Nonpuerperal Mastitis
Patógenos Incomuns Causam Doença Infrequente – Dois Casos de Mastite Não Puerperal
Inês MaioI; Joana LorenzoI; Susana TavaresII
I Department of Pediatrics, Centro Materno-Infantil do Norte, Centro Hospitalar do Porto. 4099-001 Porto, Portugal. inesmaiogoncalves@gmail.com; joanalorenzof@gmail.com
II Department of Pediatrics and Neonatology, Centro Hospitalar Entre Douro e Vouga. 4520-161 Santa Maria da Feira, Portugal. susanamrtavares@gmail.com
ABSTRACT
Mastitis is an uncommon condition in children and non-puerperal adolescents that is mostly caused by Staphylococcus aureus. We describe two cases, at different ages, without recalled trauma, and with an identification of atypical causative agents. Both patients were successfully treated with oral antibiotics.
Keywords: Adolescents; Aeromonas; Children; Elizabethkingia; Mastitis
RESUMO
A Mastite é uma patologia incomum em crianças e em adolescentes não puérperas, causada mais frequentemente pelo Staphylococcus aureus. Descrevemos dois casos em idades distintas, sem história de trauma e com identificação de agentes causais atípicos. Ambos os doentes foram tratados, com sucesso, com recurso a antibióticos orais.
Palavras-Chave: Adolescentes; Aeromonas; Crianças; Elizabethkingia; Mastite
INTRODUCTION
Mastitis, an inflammation of the breast tissue, are most frequently described in lactating women and neonates.1,2 Mastitis in children and adolescents is an uncommon condition whose risk factors and pathophysiology are not fully understood.1
Staphylococcus aureus (S. aureus) and Gram negatives, such as Escherichia coli, are the most common isolates in this condition.1-4 S. aureus accounts for more than 75% of all cases.2
Whenever possible, the pus should be sent to culture and the empirical treatment should use antibiotics that cover the most common pathogens. The treatment can be reviewed later, according to the identified bacteria, its resistance profile and the clinical evolution. The surgical treatment with open drainage should be reserved to large abscesses (>5cm), cases with systemic sepsis, or for abscesses that recur despite percutaneous drainage, since in these cases oral antibiotics are not effective.4
CASE DESCRIPTION
Case 1
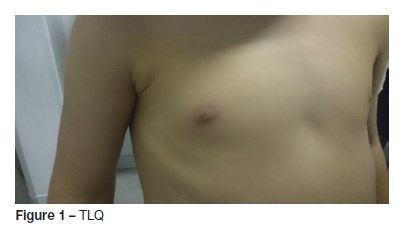
TLQ, a four-year-old boy, without relevant past medical history, namely of recurrent infections, resident in an urban household, was admitted to the emergency Department (ED) with right peri-mammillary edema erythema and persistent multiple discharge manifestations in the previous 24 hours. He was afebrile and there was no recalled trauma. An inverted nipple was observed on physical exploration (Figure 1). There were no visible skin lesions (such as fissures) and no palpable lymphadenopathies.
Oral antibiotic (flucloxacillin) was started, empirically and nipple damage was sent for culture and gram stain.
Three days later, redness and swelling persisted. The culture of the exudate was positive for Elizabethkingia meningoseptica, resistant to Flucloxacillin, so the antibiotic treatment was substituted to cotrimoxazole with favorable outcome after seven days.
Case 2
SFG is an 11 year-old girl, resident in an urban household, without relevant past medical history, premenarchal and a Tanner stage P2M2. She was brought to our ED because in the last 24 hours she had developed redness, edema and pain of the right breast without spontaneous discharge (Figure 2). Trauma wasnt recalled. She manifested fever - 39. ºC (for the first time). No other symptoms or cutaneous lesions or lymphadenopathies were present.

A swab of the pus was retrieved after gentle expression of the nipple and sent to culture. No other lab tests were thought necessary and the girl was medicated with oral Flucloxacillin for seven days.
Aeromonas hydrophilia resistant to that antibiotic was isolated in the pus, but as the girl experienced a complete recovery no change was made to the therapy.
DISCUSSION/CONCLUSIONS
Flucloxacillin was our drug of choice in both cases to cover the most common isolate described in the literature - S. aureus and oral antibiotics are usually very effective in treating children with mastitis, as we observed in both cases.1-3
The duration of the treatment and the first-line antimicrobial drug are difficult to propose, given the scarcity of clinical essays in this area.1,2 The authors, however, deem reasonable to opt for drug that covers S. aureus (according to the resistance profile of that region) and for a duration similar to that described for other Staphylococcus-associated skin and soft tissues infections – eg.: anti-Staphyloccal Penicillin or Amoxicilin/Clavulanate for seven to ten days.5
The causal factor proposed to explain mastitis in this age group is the enlargement of the breast tissue during puberty.2 This hypothesis, however, could only be applicable in our second case.
In case 1, we propose that the inverted nipple may cause duct obstruction and consequently the infectious process.3,4
Clinicians should be aware that several precipitating factors (such as trauma, duct ectasia, epidermal cysts, skin infection, cystic breast disease or even rarer entities such as Syphilitic chancre, tuberculosis or Granulomatosis with Polyangiitis can be the cause of mastitis and should be ruled out, especially when the patient does not evolve favorably.3
In case 2, who presented with fever, we opted not to order lab tests since the girl didnt have a persistent fever, the infectious focus was very apparent and she had no systemic signs. The good outcome she experienced supported our clinical choice.
Ultrasonography was not considered necessary, since it is most useful to rule out abscess formation and the physical examination was not suggestive of a large abscess and smaller collections can be managed with oral antibiotics.4 The rate of abscess formation is also lower in this age group than in neonates.1
Elizabethkingia meningoseptica, formerly known as Flavobacterium meningosepticum, is a Gram-negative bacterium that has been described as a human pathogen , but there is no available data in the literature about these bacteria causing mastitis.6 The fact that these bacteria are not usual commensal agents, was the only isolate in the pus and that the boy improved after the adjustment of antibiotics according to this agents antibiogram, is highly suggestive that E. meningosepstica was indeed the responsible agent for the infection.
Aeromonas hydrophilia is also a Gram-negative bacterium that is known to cause soft tissue infections in humans, including the breast tissue.7,8 The bacteria are usually transmitted by contaminated water.7 In this case, even though the antibiogram revealed resistance to Flucloxacilin, clinically the patient responded, so we opted to maintain the treatment.
The prognosis of this clinical condition is almost universally favorable.1,2 Whenever there is an atypical clinical course (persistence of inflammatory signs or recurrence of the disease), clinicians should consider the possibility of antimicrobial resistant organisms, the presence of abscesses in need of drainage, the existence of the aforementioned precipitating factors or a differential diagnosis.
The differential diagnoses to be considered in non-puerperal mastitis are: lactational mastitis; Mondors disease, an infrequent condition consisting of a superficial phlebitis of the breast skin that can be precipitated by trauma and that usually improves spontaneously; breast trauma (ruled out in both cases by history); mammary duct ectasia and recurrent subareolar abscess.3
Clinicians should be aware of the existence of this condition in children and non-puerperal adolescents and of the pertinence of the microbiological analysis of the exudates to direct microbial therapy.
REFERENCES
1. Stricker T, Navratil F, Forster I, Hürlimann R, Sennhauser FH. Nonpuerperal mastitis in adolescents. J Pediatr. 2006; 148:278-81. [ Links ]
2. Faden H. Mastitis in children from birth to 17 years. Pediatr Infect Dis J. 2005; 24:1113. [ Links ]
3. Greydanus DE, Matytsina L, Gains M. Breast Disorders in Children and Adolescents. Primary Care: Clinics in Office Practice. 2006; 33:455-502. [ Links ]
4. Warren R, Degnim AC. Uncommon Benign Breast Abnormalities in Adolescents. Semin Plast Surg. 2013; 27:26–8. [ Links ]
5. Bradley JS, Nelson JD. 2015 Nelsons Pediatric Antimicrobial Therapy. 21st. American Academy of Pediatrics; 2015. [ Links ]
6. Beato JN, Espinar MJ, Figueira L, Eremina YO, Ribeiro M, Moreira R, et al. Elizabethkingia meningoseptica e o Uso de Lentes de Contato. Acta Med Port 2016; 29:287-9. [ Links ]
7. Chao CM, Lai CC, Tang HJ, Ko WC, Hsueh PR. Skin and soft-tissue infections caused by Aeromonas species. Eur J Clin Microbiol Infect Dis. 2013; 32:543-7. [ Links ]
8. García-Lozano T, Oroval EA, Mojarrieta JC, Badía FM. Lesiones Vesículo-ampollosas En Un Paciente Oncológico Inmunideprimido. Revista Argentina de Microbiologia; 2012. [ Links ]
CORRESPONDENCE TO
Inês Maio
Department of Pediatrics
Centro Materno-Infantil do Norte
Centro Hospitalar do Porto
Largo Professor Abel Salazar
4099-001 Porto
Email: inesmaiogoncalves@gmail.com
Received for publication: 13.02.2017
Accepted in revised form: 25.09.2017














