Serviços Personalizados
Journal
Artigo
Indicadores
Links relacionados
Compartilhar
Nascer e Crescer
versão impressa ISSN 0872-0754versão On-line ISSN 2183-9417
Nascer e Crescer vol.27 no.4 Porto dez. 2018
https://doi.org/10.25753/BirthGrowthMJ.v27.i4.14041
QUAL O SEU DIAGNÓSTICO? | WHAT IS YOUR DIAGNOSIS?
Perinatal clinical case
Caso clínico perinatal
Marta AlvesI, Liliana BrancoII, Andreia LopesI, Bárbara PereiraI
I Pediatrics Department, Hospital Senhora da Oliveira - Guimarães. 4835-044 Guimarães, Portugal. martaalves@hospitaldeguimaraes.min-saude.pt; andreia.m.castro.lopes@gmail.com; bsgopereira@gmail.com
II Pediatrics Department, Hospital de Braga 4710-243 Braga, Portugal. brancoliliana@hotmail.com
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
A 16-day-old male was observed at the Emergency Department for a right cervical mass noticed on the same day by the parents, with no other associated symptoms. He was a full-term child, delivered by vacuum extraction, with an uneventful perinatal period.
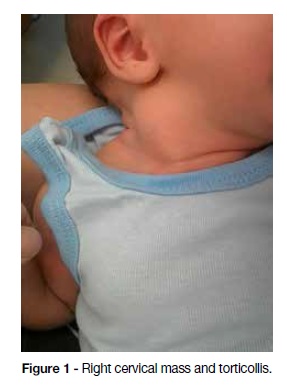
At the time of physical examination, a cervical mass was palpable in the inferior portion of the right sternocleidomastoid muscle, in association with ipsilateral torticollis.
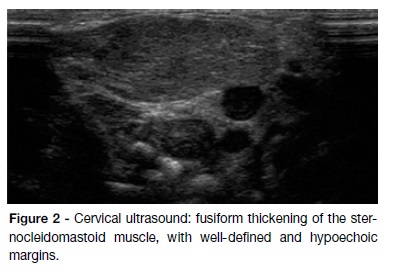
Cervical ultrasound revealed a fusiform thickening of the sternocleidomastoid muscle, with well-defined, hypoechoic margins, confirming the diagnosis of fibromatosis colli.
Parents were instructed to adopt positioning measures and physical therapy was initiated, with clinical resolution by seven months of age.
Fibromatosis colli is the most severe presentation of congenital muscular torticollis. Although typical clinical findings usually enable the diagnosis, cervical ultrasound is useful to confirm muscular origin of the mass.
Torticollis in the opposite direction of the mass, spinal deformities, abnormal eye movements, or other abnormal neurological findings should prompt the investigation of alternative etiologies.
Keywords: Fibromatosis colli; Newborn; Torticollis
RESUMO
Um recém-nascido de 16 dias, do sexo masculino, foi observado no Serviço de Urgência devido a uma tumefação cervical direita, observada no próprio dia pelos pais. Tratava-se de um recém-nascido de termo, nascido de parto por ventosa, sem intercorrências no período perinatal.
Ao exame físico, apresentava uma tumefação na porção inferior do músculo esternocleidomastoideu direito, associada a torcicolo ipsilateral.
A ecografia cervical revelou um espessamento fusiforme do músculo esternocleidomastoideu, com margens bem delimitadas, hipoecóicas, confirmando o diagnóstico de fibromatose coli.
A instituição de medidas posturais foi recomendada aos pais e iniciado tratamento fisiátrico, com resolução clínica aos sete meses de idade.
A fibromatose coli constitui a apresentação mais grave de torcicolo muscular congénito. Embora os achados clínicos típicos geralmente possibilitem o diagnóstico, a ecografia cervical é útil na confirmação da origem muscular da massa.
Torcicolo na direção oposta à massa, deformidades da coluna vertebral ou alterações ao exame neurológico devem motivar a investigação de etiologias alternativas.
Palavras-chave: Fibromatosis colli; Recém-nascido; Torcicolo
Medically supervised pregnancy occurred normally and the child was born by vacuum extraction at 38 weeks of gestation, with good adaptation to extrauterine life and adequate somatometry for gestational age.
At the time of physical examination, a right cervical mass with a 2 cm of approximate diameter was palpable in the inferior portion of the sternocleidomastoid muscle. The mass had regular contours, elastic consistency, and no inflammatory signs. It was associated with a right torticollis, slight rotation of the chin to the opposite side, and mildly limited passive range of motion (Figure 1). Neurological examination was normal, as was the remaining physical exam.
Cervical ultrasound revealed a heterogeneous and fusiform thickening of the sternocleidomastoid muscle, with well-defined and hypoechoic margins, with an anteroposterior diameter of 1.2 cm (Figure 2).
What is your diagnosis?
Diagnosis
Fibromatosis colli
Orientation
Parents were instructed to adopt positioning and handling measures and physical therapy was initiated, with clinical resolution at seven months of age.
Discussion
Fibromatosis colli refers to the fibrous thickening of the sternocleidomastoid muscle causing limited passive range of motion and is the most severe presentation of congenital muscular torticollis.1 Although typical clinical findings usually enable the diagnosis, cervical ultrasound is useful to confirm muscular origin of the mass.1
Torticollis in the opposite direction of the mass, spinal deformities, abnormal eye movements, or other abnormal neurological findings, should prompt the investigation of alternative causes of torticollis (vertebral anomalies, ocular torticollis, central nervous system lesions).1
Fibromatosis colli is usually associated with good prognosis, once postural measures and physical therapy are implemented.2 Nonetheless, vigilance should be kept in order to identify craniofacial deformities that may arise as a complication of this form of congenital muscular torticollis. Duration of physical therapy depends on clinical severity and age at diagnosis.3 In cases where physiotherapy fails, surgery may be indicated.3
REFERENCES
1. Macias CG, Gan V. Congenital muscular torticollis: Clinical features and diagnosis. UpToDate. 2017. Retrieved February 2018 from: www.uptodate.com/contents/congenital-muscular-torticollis-clinical-features-and-diagnosis. [ Links ]
2. Cheng JC, Wong MW, Tang SP, Chen TM, Shum SL, Wong EM. Clinical determinants of the outcome of manual stretching in the treatment of congenital muscular torticollis in infants. A prospective study of eight hundred and twenty-one cases. J Bone Joint Surg Am 2001; 83-A:679. [ Links ]
3. Kaplan SL, Coulter C, Fetters L. Physical therapy management of congenital muscular torticollis: an evidence-based clinical practice guideline: from the Section on Pediatrics of the American Physical Therapy Association. Pediatr Phys Ther. 2013; 25:348-94. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Marta Alves
Pediatrics Department
Hospital Senhora da Oliveira
Rua dos Cutileiros
Creixomil 4835-044
Guimarães
Email: martaalves@hospitaldeguimaraes.min-saude.pt
Received for publication: 07.03.2018
Accepted in revised form: 24.05.2018