Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Nascer e Crescer
versão impressa ISSN 0872-0754versão On-line ISSN 2183-9417
Nascer e Crescer vol.28 no.2 Porto jun. 2019
https://doi.org/10.25753/BirthGrowthMJ.v28.i2.14322
ORIGINAL ARTICLES | ARTIGOS ORIGINAIS
Anti-n-methyl-d-aspartate receptor encephalitis in pediatric age
Encefalite anti-recetor n-metil-d-aspartato em idade pediátrica
Mariana BrancoI, Luísa SousaII, Cristina GarridoI, Inês CarrilhoI, Manuela SantosI, Teresa TemudoI, Ana Martins SilvaII, Sónia FigueiroaI
I Neuropediatrics Department, Centro Materno-Infantil do Norte, Centro Hospitalar Universitário do Porto. 4050-651 Porto, Portugal. mariana.a.branco@hotmail.com; cgarridopt@gmail.com; icccarrilho@gmail.com; manuela.a.santos@gmail.com; ttemudo11@gmail.com; sonia.figueiroa@gmail.com
II Neurology Department, Centro Hospitalar Universitário do Porto. 4099-001 Porto, Portugal. luisacmsousa@gmail.com; anaadmsilva@gmail.com
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Introduction: Anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis is an immune-mediated syndrome characterized by psychiatric symptoms, movement disorders, insomnia, seizures, altered level of consciousness and autonomic dysfunction. The aim of this study was described the cases of anti-NMDAR encephalitis admitted to a Neuropediatrics Department, in order to alert for the importance of early recognition of this clinical entity due to its implications in prognosis.
Material and Methods: A retrospective review of the clinical processes of patients with anti-NMDAR encephalitis admitted to the Neuropediatrics Department of a University Hospital in the period between May 2009 and May 2016 was conducted.
Results: Diagnosis of anti-NMDAR encephalitis was established in nine patients. Mean age at diagnosis was 9.4 years and five patients were male. Most cases (88.9%) presented with neuropsychiatric symptomatology. Movement disorders were another frequent finding (88.9%) and include chorea, dystonia and dyskinesias. Altered level of consciousness occurred in 77.8% of cases, insomnia and speech disturbance in 66.7%, seizures in 55.6% and autonomic dysfunction in 22.2%. Anti-NMDAR antibodies were identified in the cerebrospinal fluid of all patients. One patient had an underlying neoplasm. All patients underwent immunosuppressive therapy and seven patients fully recovered. In the remaining patients, sequelae included refractory epilepsy and cognitive impairment.
Discussion: The diagnosis of anti-NMDAR encephalitis should be considered in children and adolescents presenting with psychiatric symptoms associated and movement disorders. In this sample, although most patients responded very favorably to treatment, severe sequelae were also observed. This highlights the importance of an early diagnosis to initiate treatment as soon as possible.
Keywords: antibodies; encephalitis; neoplasm
RESUMO
Introdução: A encefalite anti-recetor N-metil-D-aspartato (NMDAR) é uma síndrome imunomediada, que se caracteriza por sintomas psiquiátricos, distúrbios do movimento, insónia, crises epiléticas, alterações do estado de consciência e instabilidade autonómica. O objetivo deste estudo foi efetuar uma descrição dos casos de encefalite anti-receptor N-metil-D-aspartato admitidos no Serviço de Neuropediatria, de modo a alertar para a importância do reconhecimento precoce desta entidade clínica devido às suas implicações prognósticas.
Material e Métodos: Foi realizado um estudo retrospetivo com revisão dos processos clínicos dos doentes com diagnóstico de encefalite anti-NMDAR admitidos no Serviço de Neuropediatria de um Hospital Universitário no período entre maio de 2009 e maio de 2016.
Resultados: Foi estabelecido o diagnóstico de encefalite anti-NMDAR em nove doentes. A idade média ao diagnóstico foi de 9,4 anos e cinco casos ocorreram no sexo masculino. A maioria dos casos (88,9%) apresentou sintomatologia neuropsiquiátrica. Distúrbios do movimento, caracterizados por coreia, distonia ou discinesias, foram igualmente frequentes (88,9%). Alterações do estado de consciência ocorreram em 77,8% dos casos, insónia e alterações na linguagem em 66,7%, crises epiléticas em 55,6% e sintomas disautonómicos em 22,2%. Em todos os doentes foram identificados anticorpos anti-NMDAR no líquido cefalorraquidiano. Um dos doentes apresentava uma neoplasia subjacente. Todos os doentes realizaram tratamento imunossupressor e sete recuperaram completamente. Os restantes doentes apresentaram sequelas que incluíram epilepsia refratária e alterações cognitivas.
Discussão: O diagnóstico de encefalite anti-NMDAR deve ser considerado em crianças e adolescentes que apresentam sintomas psiquiátricos e distúrbios do movimento. Na presente amostra, embora a maioria dos doentes tenha respondido favoravelmente ao tratamento, também se verificou a ocorrência de sequelas graves. Com este trabalho, pretende reforçar-se a importância do diagnóstico precoce e instituição de terapêutica para esta entidade clínica.
Palavras-chave: anticorpos; encefalite; neoplasia
INTRODUCTION
Encephalitis comprises a group of disorders characterized by acute dysfunction of the central nervous system with imaging and/ or laboratory evidence of cerebral inflammation. There are several possible causes and differential diagnoses of encephalitis, especially when considering infectious agents. In a significant portion of patients, however, the etiology remains indeterminate.1,2
In recent years, some of these cases have been associated with antibodies against receptors and cell surface proteins involved in synaptic transmission, plasticity or neuronal excitability, allowing a definitive diagnosis of auto-immune or paraneoplastic encephalitis.2,3 In 2007, Dalmau et al. reported the discovery of an antibody associated with a condition characterized by acute psychiatric symptoms, seizures, altered level of consciousness, among others, which reacted with NR1 / NR2 heteromers of the N-methyl-D- aspartate receptor (NMDAR). In 2008, the syndrome was fully delineated in a case series of 100 patients and the target epitopes were identified in the NR1 subunit of NMDAR. The syndrome is now referred to as anti-NMDAR encephalitis. Although initially described in women with ovarian teratoma, it has since then also been described in men and, more recently, in children and adolescents.4,5 Anti-NMDAR encephalitis is a neuropsychiatric syndrome caused by immune-mediated processes, with autoantibodies in serum or cerebrospinal fluid directed against an epitope located in the extracellular domain of the N-methyl-D-aspartate receptor.5-7
It is the most common autoimmune encephalitis in pediatric age, with a reported prevalence of 4% among all encephalitis` cases, according to a multicenter U.K. study.5 The syndrome occurs predominantly in children and young adults and may or may not be associated with tumors. The co-occurrence of neoplastic disease is dependent on age, sex and race, being more frequent in females older than 18 years of age and slightly more common in the patients of African descent.3,5
The syndrome has a typical progression in adults and adolescents and usually starts with a prodromal phase with fever, headache or symptoms similar to an upper respiratory infection that often go unnoticed, followed by psychiatric symptoms and insomnia a few days to weeks later, finally progressing to changes in the state of consciousness, seizures, movement disorders and autonomic dysfunction. In children, although the phenotype is similar, presenting symptoms usually include movement disorders, seizures and speech disturbances.2,3,7
Patients with suspected autoimmune encephalitis should perform brain magnetic resonance imaging (MRI), electroencephalogram (EEG), lumbar puncture and a serological study to confirm the diagnosis and exclude alternative etiologies.3,5,7 The definitive diagnosis is confirmed by detection of antibodies against the NMDA receptor in cerebrospinal fluid and/or serum. Presence of an underlying neoplasm should also be thouroughly assessed.2,4,7 Although no standard treatment has been established to date, evidence suggests that tumor excision, when present, and immunosuppressive treatment improve prognosis.5,7
This work intends to describe the cases of anti-NMDAR encephalitis identified in a Neuropediatric Department, with the aim of raising awareness of the importance of early recognition of this clinical entity due to its prognostic implications.
MATERIALS AND METHODS
A retrospective study was conducted by reviewing clinical charts of patients with anti-NMDAR encephalitis admitted to the Neuropediatric Department of a University Hospital in the period between May 2009 and May 2016. Variables analyzed included age at diagnosis, gender, clinical manifestations, diagnostic tests performed, associated tumors, treatment, mortality and relapses. An analytical study was performed for all patients, which included cerebrospinal fluid (CSF) analysis, EEG and brain MRI with gadolinium, including T1, T2, FLAIR, and diffusion weighted images. Disease diagnosis was confirmed upon detection of antibodies against the NMDA receptor in cerebrospinal fluid and/or serum. Abdominal ultrasound, scrotal ultrasound and/or thoracic, abdominal and pelvic computed tomography were performed in all patients to exclude tumors. Descriptive analysis of variables was performed with SPSS 20.0.
RESULTS
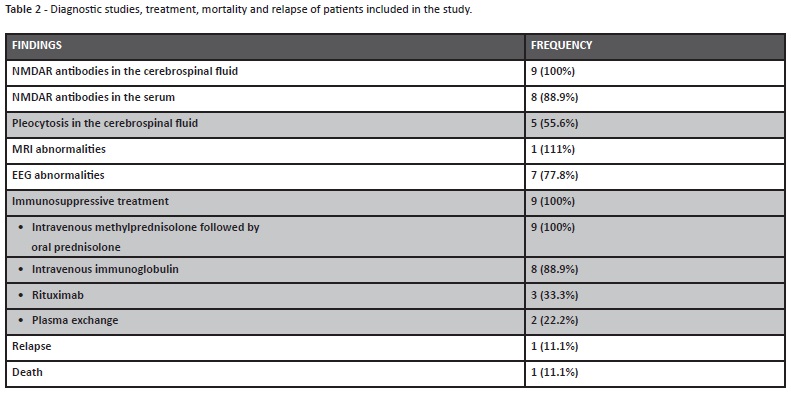
Anti-NMDAR encephalitis diagnosis was established in nine patients. Mean and median age at diagnosis were 9.4 and 8 years, respectively, with ages between two and 17 years old. A total of 55.6% of patients were male. Table 1 shows demographic and clinical manifestations of each patient.
(clique para ampliar ! click to enlarge)
Two patients developed prodromal symptoms a few days before the full-blown phase, including fever and vomiting in one case and fever and odynophagia in another case. In four patients, the first symptom was neuropsychiatric and included behavioral change with temper tantrums and apathy in one child and a combination of anxiety, agitation, heteroagressivity, social isolation and hallucinatory activity in three adolescents. Noteworthy, one of these cases, a 17-year-old male had three admissions in a psychiatric department in a period of seven months before diagnosis. Clinical presentation was characterized by acute and exuberant auditory, visual and olfactory hallucinations that responded to antipsychotic treatment but recurred. The florid presentation and resistance to treatment led to patient referral to the Neuropediatric department due to suspicion of an underlying neurological condition. It is also worth mentioning the case of a 17-year-old female adolescent, with gradual installation of behavioral changes with social isolation and low frustration tolerance followed by episodes of psychomotor agitation with disorganized speech, insomnia and hallucinatory activity. An initial hypothesis of toxic psychosis was considered and the patient was admitted to psychiatry department and medicated with antipsychotics. During hospitalization, she developed periods of mutism and fluctuating levels of consciousness. The girl subsequently exhibited an episode of cervical hyperextension, conjugate deviation of the eyes, apnea and perioral cyanosis, which led to admission to an intensive care unit due to suspicion of neuroleptic malignant syndrome. However, clinical evolution allowed a definitive diagnosis in both cases. In the remaining patients, the first symptom was seizures (two cases), movement disorders (two cases) and speech disturbance (one case). Overall, psychiatric symptomatology characterized by behavioral changes and/or psychotic symptoms occurred in 88.9% of cases. Movement disorders, characterized by chorea, dystonia or dyskinesias also occurred in 88.9% of cases. Altered level of consciousness occurred in 77.8% of cases, insomnia and speech disturbance in 66.7%, seizures in 55.6% and autonomic dysfunction in 22.2%.
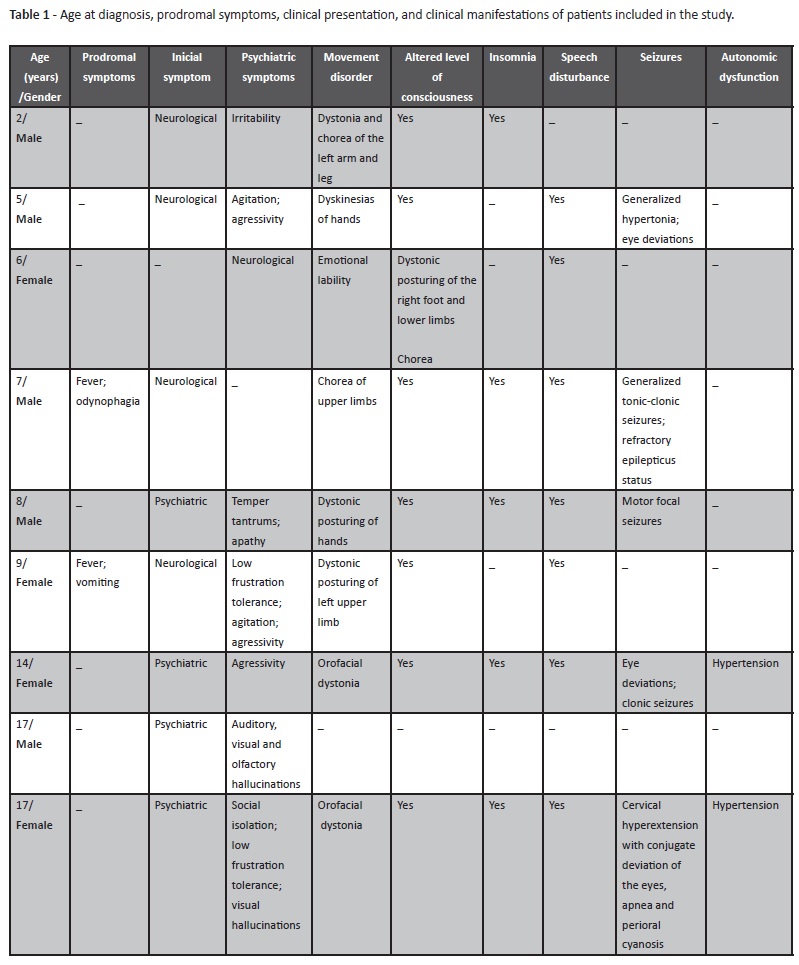
Regarding work-up, NMDAR antibodies were identified in the cerebrospinal fluid of all patients and in the serum of eight (Table 2). In five patients, pleocytosis was observed in the cerebrospinal fluid. Brain MRI changes were only found in one case, with hyperintensity of the right frontal cortex and right insular cortex with loss of differentiation between white and gray matter. In seven patients, the electroencephalogram showed altered background rhythm with generalized slow activity and focal or generalized paroxysmal activity. Importantly, the extreme delta brush pattern was not identified in any patient. No tumors were detected during the initial investigation but and 18-year-old patient was diagnosed with an ovarian teratoma after 19 months of follow-up.
All patients underwent immunosuppressive therapy, initially with intravenous methylprednisolone followed by oral prednisolone. Eight patients required treatment with intravenous immunoglobulin and two with plasma exchange. Three patients received rituximab. Plasma exchange was performed in two patients due to lack of response to corticosteroids and intravenous immunoglobulin. Rituximab was administered to two patients due to lack of response to plasma exchange and in one patient after no response to corticosteroids and intravenous immunoglobulin.
Four patients required admission to the Intensive Care Unit due to decreased level of consciousness and refractory status epilepticus. One patient required surgery with left occipital lobectomy for refractory epilepticus status.
The mean length of hospital stay was 38.7 days with a minimum of three days and a maximum of 126 days.
At discharge, seven patients had persistent disease manifestations, including movement disorders (dystonia and chorea), psychiatric symptoms (emotional lability and agitation), speech disturbances (reduction of verbal output and impaired of verbal fluency and articulation) and epilepsy. After an average follow-up of 31.7 months (minimum 2 months, maximum 69 months), five patients fully recovered. In this sample, one relapse occurred two years after diagnosis in a patient with refractory epilepsy. The patient died, two years later, due to septic shock with multiorgan failure.
DISCUSSION
Clinical suspicion of anti-NMDAR encephalitis is based on a myriad of characteristic signs and symptoms and the present study supports the concept that anti-NMDAR encephalitis presentation in children may be different compared with adults.2,3,8 In this sample, all adolescents included presented with psychotic symptoms, while children exhibited more subtle behavioral changes, such as anxiety, agitation, or bizarre behavior. This pattern has been previously reported and may contribute to delayed diagnosis in earlier ages.3,4,9 One the other hand, presentation with isolated psychiatric symptoms lead to two hospitalizations in Psychiatry Department and associated treatment delay. In these cases, as in others described in the literature, the clinical course was decisive for determination of a definitive diagnosis.2,4,7
It should be noted, that, in young children, first symptoms recognized are predominantly non-psychiatric. Orofacial dyskinesias are the most characteristic movement disorders of anti-NMDAR encephalitis, although other types of movement disorders may occur such as choreoathetosis, dystonia, and rigidity. In this sample, movement disorders were identified in 88.9% of cases, and this proportion is in accordance with the literature.4,5,9 In more severe and advanced stages, patients may present with opisthotonic postures and oculogyric crises, which are associated with tachycardia and hypertension.4
Insomnia, a usually prominent and early symptom was frequently observed in this study. In fact, patients may not be able to sleep for days despite sedative medication, and insomnia resolution may be one of the first signs of clinical improvement. In contrast, during recovery, patients may have hypersomnia.4,5 Speech disturbance ranges from reduction of verbal output to mutism and cannot be attributed to cortical aphasia.5,9
Seizures occur at early stages of the disease and may be difficult to diagnose and treat. Epilepsy may become refractory, as evidenced in one patient in this study who required surgery.4,5,10
Autonomic dysfunction occurred in only 22% of patients and, although less frequent in pediatric age, it is a potentially fatal complication that must be addressed. Manifestations include hyperthermia, blood pressure fluctuations, tachycardia, bradycardia, and sometimes hypoventilation.5,6
One should be cautious when accepting the diagnosis of anti- NMDAR encephalitis in monosymptomatic cases. This was evident in one adolescent included in this cohort for whom symptomatology was exclusively psychiatric and is further complicated by variable frequencies of false positive results of anti-NMDAR antibodies due to different methods employed. A cell-based IgG anti-NMDAR test should be preferred, and in dubious cases a reassessment of antibodies in the cerebrospinal fluid and/or serum should be considered.8,11,12 To increase specificity, CSF measurement of anti- NMDAR should be preferred over serum values.12
Although the presence of pleocytosis is not universal and some studies report a frequency around 87%, in this sample it was observed only in five cases.4,8,11
Only one patient had brain MRI findings. The frequency of MRI abnormalities is lower in children than adults and particularly useful to exclude other pathologies such as a cerebrovascular events or neoplastic disease.7,8,11 In contrast, EEG was abnormal in most patients. Changes are generally nonspecific as evidenced in the present study. Although an extreme delta brush pattern, associated with a longer disease, is reported in approximately on third of adult patients with anti-NMDAR encephalitis, was not found in this cohort. Although preceding infections have been suspected to play a role in triggering autoimmune encephalitis, this was only demonstrated for herpes simplex viral encephalitis to date, and in this sample cases of anti-NMDAR encephalitis after herpetic encephalitis were not reported.7
Although association with tumors is less frequent in pediatric age, this should always be addressed. Ovarian teratomas are identified in around 56% of women older than 18 years of age. By contrast, these tumors occur in less than 30% of adolescents younger than 18 years of age. In males, the occurrence of tumors is rare. Other tumors reported in the literature include testicular germ cell tumor, teratoma of the mediastinum, Hodgkin lymphoma, and neuroblastoma.2,7,12 In this study an ovarian teratoma was identified in one patient after 19 months of follow-up, highlighting the importance of long-term follow-up of these patients.
Once diagnosis has been established through detection of NMDAR antibodies, immunosuppressive treatment should be instituted rapidly, as early treatment can improve prognosis, accelerate recovery, and reduce the risk of relapse.2,4,7
In absence of randomized studies, treatment should be individualized and take into account patient’s age, clinical severity, and tumor presence. Initial treatment usually includes intravenous methylprednisolone followed by intravenous immunoglobulin or plasma exchange and tumor excision, whenever indicated. In absence of clinical improvement, which occurs approximately 30-40% of cases, second line treatment should be initiated with rituximab, cyclophosphamide or both. There is increasing evidence that the use of rituximab in critically ill patients is very effective. Given the potential adverse effects of cyclophosphamide, this agent is only used when the above mentioned treatments have failed.2,7,14 As treatment should be individualized, patients in this study were offered different treatment approaches, with adjustments in timing of change to second line immunotherapy and in duration of treatment according to clinical course and severity.
Relapse is reported to occur in 15-24% of cases, sometimes years after diagnosis, and may be monosymptomatic and less severe than initial presentation.7,8 As an exception, one patient in this cohort experienced relapse with severe refractory epilepsy.
Prognosis of this condition is highly variable, depending on presence of an underlying tumor and its stage and on symptom severity. Studies demonstrate that approximately 75% of patients substantially or fully recover. Diagnosis and treatment delay has been associated with poorer prognosis.4,5,7 Residual symptoms usually reflect a fronto-limbic dysfunction, which includes difficulty in attention and planning, impulsivity, and behavioral disinhibition. However, long-term follow-up shows that in many patients these symptoms continue to improve over time.3,4
Sequelae were reported on discharge in seven cases and included movement disorders, speech disturbance, psychiatric symptoms and epilepsy. However, five of these patients fully recovered after an average follow-up of 31.7 months.
Results of this study suggest that initial symptoms in children may be different from adults, predominantly neurological in younger ages and more psychiatric in adolescents and adults. Although this disease is potentially fatal most patients respond to immunotherapy and the second line immunotherapy with rituximab is often effective. Early consideration of this diagnosis is of utmost importance to initiate treatment as early as possible and prevent complications.
REFERENCES
1. Brito MJ, Luís C, Silva R, Gouveia C, Vieira JP. Encefalites - Recomendações da Sociedade de Infecciologia Pediátrica e da Sociedade Portuguesa de Neuropediatria. Acta Pediatr Port 2011: 42:284-91. [ Links ]
2. Armangue T, Pedrol MP, Dalmau J. Autoimmune Encephalitis in Children. J Child Neurol. 2012; 27:1460-9. [ Links ]
3. Ferdinand P, Mitchell L. Anti-NMDA Receptor Encephalitis. J Clin cell Immunol 2012; S 10:007. [ Links ]
4. Florance-Ryan N, Dalmau J. Update on anti-N-methyl-D- aspartate receptor encephalitis in children and adolescents. Current Opinion in Pediatrics 2010; 22:739-44. [ Links ]
5. Dalmau J, Lancaster E, Hernandez EM, Rosenfeld MR, Gordon RB. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol 2011; 10:63-74. [ Links ]
6. Borlot F, Santos MLF, Bandeira M, Liberalesso PB, Kok F, Lohr A, et al. Anti-N-methyl D-aspartate receptor encephalitis in childhood. J Pediatr (Rio J) 2012; 88:275-8. [ Links ]
7. Dalmau J, Rosenfeld MR. Paraneoplastic and autoimmune encephalitis. UpToDate 2017. [ Links ]
8. Armangue T, Titulaer MJ, Málaga I, Bataller L, Gabilondo I, Graus F, et al. Pediatric Anti-NMDA encephalitis - Clinical analysis and novel findings in a series of 20 patients. J Pediatr. 2013; 162:850- 6. [ Links ]
9. Baker J, Jeziorkowski C, Siebe C, Osborn MB. Two Cases of Anti- NMDA Receptor Encephalitis. West J Emerg Med.2016; 17:623-6. [ Links ]
10. Matoq AA, Rappoport AS, Yang Y, O` Babatunde J, Bakerywala R, Sheth RD. Anti-NMDA- receptor antibody encephalitis in infants. Epilepsy and Behavior Case Reports 4 (2015): 99-101. [ Links ]
11. Graus F, Titulaer M, Balu R, Benseler S, Bien CG, Cellucci T, et al. A clinical approach to diagnosis of autoimmune encephalitis. The Lancet Neurology. 2016; 15:391-404. [ Links ]
12. Hara M, Martinez-Hernandez E, Ariño H, Armangué T, Spatola M, Petit-Pedrol M, et al. Clinical and pathogenic significance of IgG, IgA, and IgM antibodies against the NMDA receptor. Neurology 2018; 0:1-9. [ Links ]
13. Kubota S, Fuchigami T, Momoki E, Hoshi R, Furuya T, Kusumi Y, et al. Anti-N-Methyl-D-Aspartate Receptor Encephalitis and Ovarian Teratoma: A Case Report. Int J Clin Pediatr. 2017; 6:20-3. [ Links ]
14. Bartolini L. How do you treat anti-NMDA receptor encephalitis? Neurol Clin Pract 2016; 6: 69-72. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Mariana Branco Neuropediatrics Department
Unidade Local de Saúde do Alto Minho Estrada da Santa Luzia,
4901-858 Viana do Castelo
E-mail: mariana.a.branco@hotmail.com
Received for publication: 16.05.2018
Accepted in revised form: 23.11.2018