Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Nascer e Crescer
versão impressa ISSN 0872-0754versão On-line ISSN 2183-9417
Nascer e Crescer vol.28 no.2 Porto jun. 2019
https://doi.org/10.25753/BirthGrowthMJ.v28.i2.14853
CASE REPORTS | CASOS CLÍNICOS
Chronic rhinosinusitis with bone destruction in a teenager with cystic fibrosis
Rinossinusite crónica com destruição óssea numa adolescente com fibrose quística
João Rio MartinsI, João Fonseca NevesII, Teresa Reis SilvaI, Miguel FélixI
I Pediatric Cystic Fibrosis Center, Hospital Pediátrico de Coimbra, Centro Hospitalar e Universitário de Coimbra. 3000-602 Coimbra, Portugal. joaoriomartins@gmail.com; trs.mail@gmail.com; miguelfelixff@gmail.com
II Department of Otorhinolaryngology, Hospital Pediátrico de Coimbra, Centro Hospitalar e Universitário de Coimbra. 3000-602 Coimbra, Portugal. j.fonsecaneves@gmail.com
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Introduction: Chronic rhinosinusitis (CRS) is almost invariably present in cystic fibrosis (CF) patients, with a detrimental impact in their quality of life. Functional endoscopic sinus surgery (FESS) has been proven effective when medical management approaches are exhausted.
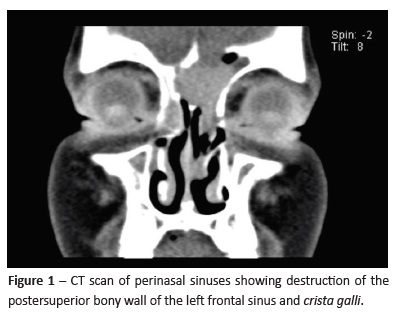
Case Summary: A twelve-year-old female with CF and a several-month history of intermittent fever, recurrent cough, and purulent sputum despite intensive medical management was admitted due to fever and frontal headaches starting a few days after initiation of nocturnal non-invasive ventilation. Perinasal and cerebral sinuses’ computed tomography scan and magnetic resonance imaging showed a severe CRS complicated with bone destruction of the left frontal sinus and crista galli. Intravenous antibiotics and antifungal were started, and FESS was performed with significant clinical improvement. Microbiologic study was positive for methicillin-resistant Staphylococcus aureus.
Discussion: This case shows that regular assessment of sinusal disease in CF children is essential, especially in those with chronic infections. FESS may be usefull when medical management approaches are exhausted, effectively improving patients’s quality of life.
Keywords: bone destruction; chronic rhinosinusitis; cystic fibrosis; endoscopic sinus surgery; methicillin-resistant Staphylococcus aureus
RESUMO
Introdução: A rinossinusite crónica está quase invariavelmente presente nos doentes com fibrose quística (FQ), influenciando negativamente a sua qualidade de vida. A cirurgia endoscópica nasossinusal (CENS) tem demonstrado ser efetiva quando a abordagem médica é esgotada. Caso clínico: Uma adolescente com FQ e história prolongada de febre e tosse recorrente com secreções purulentas apesar de terapêutica médica otimizada foi admitida por febre e cefaleias frontais com início poucos dias após ter iniciado ventilação não-invasiva noturna. Tomografia computorizada e ressonância magnética dos seios perinasais e cerebral revelaram a presença de rinossinusite crónica grave, com destruição óssea do seio frontal esquerdo e da crista galli. Foi iniciada terapêutica antibiótica e antifúngica endovenosas e realizada CENS, com melhoria clínica significativa. A cultura de secreções identificou Staphilococcus aureus meticicilno-resistente.
Discussão: Este caso demonstra que a abordagem da doença sinusal é essencial em crianças com FQ, particularmente naquelas com infeções crónicas. A CENS pode ser útil quando a terapêutica médica é insuficiente, melhorando significativamente a qualidade de vida destes doentes.
Palavras-chave: destruição óssea; rinossinusite crónica; fibrose quística; cirurgia endoscópica sinusal; Staphilococcus aureus meticicilno- resistente
Introduction
Chronic rhinosinusitis (CRS) has been shown to negatively impact patient’s quality of life and is an independent risk factor for development of airflow obstruction in patients without lower respiratory disease.1
The most common life-shortening complication of cystic fibrosis (CF) is pulmonary deterioration from frequent lung infections. However, chronic paranasal and sinus disease is present in nearly 100% of CF patients, with two thirds developing nasal polyps and up to 24% requiring surgical management of sinus disease.2
CF-associated CRS has a different physiopathology from the non- CF disease. Impaired chloride ion transport leads to sodium and water absorption from the cell luminal surface, reducing secretion water content and increasing mucus viscosity. The distinctive viscous mucus leads to impaired ciliary function, mucous stasis, and bacterial superinfection. When involving the adjacent bony framework of paranasal sinuses, the long-standing inflammation caused by sinonasal polyposis and sinusitis may lead to localized osteitis and, less frequently, bone destruction.
Methicillin-susceptible Staphylococcus aureus is the most common pathogen found in sinuses of children with CF, followed by Pseudomonas aeruginosa and Haemophilus influenzae.3 The prevalence of methicillin-resistant Staphylococcus aureus (MRSA) in lower respiratory tract and sinus culture significantly increased over the last two decades, with concordance rates between both reported to be as high as 80%.3
Although medical therapy is the mainstay of treatment, functional endoscopic sinus surgery (FESS) is indicated for CRS treatment in patients with CF when medical management approaches fail, effectively improving sinusitis subjective symptoms and self-reported quality of life.4 The optimal treatment, surgical indications, and outcomes of CF CRS remain unknown, leading to a wide variation in practice patterns.
Case report
A 12-year-old female patient with cystic fibrosis (homozygous for F508del-CFTR mutation) and chronic infection with MRSA and Haemophilus influenza presented with a several-month history of intermittent fever, productive cough, and purulent sputum.
Fever was mild, ranging from 37.5 to 38.5ºC once a day and controlled with antipyretic medication, and was associated with an increase in cough frequency and purulent sputum production.
These complaints led to multiple hospital admissions and to an extensive etiologic study including multiple blood and sputum cultures, chest radiography, chest computed tomography (CT), broncofibroscopy with bronchoalveolar lavage, echocardiogram, abdominal ultrasound, and several courses of broad-spectrum antibiotic treatments (amoxicillin and clavulanic acid, ciprofloxacin, linezolid, cotrimoxazole, erythromycin, meropenem, and teicoplanin). After each antibiotic course, the girl remained asymptomatic for a short period of time ranging from a few days to three weeks. The symptom-free intervals became shorter over time and failure to gain weight was observed.
On March 2018, the girl was admitted to our department with fever relapse, paroxysmal cough with purulent sputum, and complaints of frontal headaches with morning predominance, noticed some days after starting nocturnal non-invasive ventilation (bilevel, via nasal mask). Perinasal sinuses and cerebral CT scan complemented with magnetic resonance imaging were performed, showing signs of severe chronic rhinosinusitis (Lund-Mackay Score = 24 points) complicated with destruction of the posterosuperior bony wall of the left frontal sinus and part of crista galli resulting in communication to the adjacent frontal lobe parenchyma (Figure 1), with no signs of epidural abscess.
Antibiotic treatment with meropenem and teicoplanin and antifungal treatment with voriconazole were instituted, and FESS drainage was performed. A bilateral middle meatal antrostomy with anterior ethmoidectomy was performed, followed by a Type I Draft in the right frontal recess and a Type IIa Draft on the left frontal recess. Purulent content was collected from the left frontal sinus and microbiology study was positive for MRSA. No fungi were identified. Hystopathology identified a nasal polyp. Intravenous antibiotherapy was maintained for three weeks following surgery, followed by two weeks of oral antibiotherapy with linezolide. The patient remained afebrile and with occasional complaints of mild frontal pressure, especially during nasal washings. Non-invasive ventilation was temporarily suspended. The girl was hospital discharged three weeks after surgery, and two months after FESS she remains asymptomatic.
Discussion
Children with CF have a high incidence of CRS, but the true impact of sinusal disease on these patients’s quality of life is not well understood yet.
Evidence shows no significant improvement in pulmonary function tests (PFT) in CF patients after FESS, and PFT gains after surgery may be temporary due to CF progression. On the other hand, a decrease in the number and length of hospital admissions, need for antibiotic therapy, and respiratory exacerbations have been reported.5
This case describes a particularly severe and advanced stage of CRS complicated with bone destruction in a child with CF, MRSA chronic infection, and a long-lasting history of intermittent fever, cough, and purulent sputum despite intensive medical management approaches, with a significant clinical improvement after FESS. Previous reports of cases with the same level of local severity, including bony destruction, have not been found in the literature.
The authors believe that this report supports the potentially beneficial role of FESS in children with CF and CRS and highlights the need for regular sinusal disease assessment in these children, particularly those with chronic infections and initiating non-invansive ventilation, as persistent inflamation and increased airway pressure can induce dramatic cranial bone destruction only a few years after CF diagnosis. There is also a need for quality evidence on postoperative quality of life improvement and adjunct medical therapy efficacy in children with CF.
REFERENCES
1. Yousof AM, Awada OG, Fattahb MTA, Ahmadac SF. Pulmonary function tests in patients with chronic rhinosinusitis and the effect of surgery. Egyptian Journal of Bronchology 2017; 11:283-7. [ Links ]
2. Virgin FW. Clinical Chronic Rhinosinusitis Outcomes in Pediatric Patients with Cystic Fibrosis. Laryngoscope Investig Otolaryngol. 2017; 2:276-80. [ Links ]
3. Digoy GP, Dunn JD, Stoner JA, Christie A, Jones DT. Bacteriology of the paranasal sinuses in pediatric cystic fibrosis patients. International Journal of Pediatric Otorhinolaryngology 2012; 76:934-8. [ Links ]
4. Tumin D, Hayes Jr. D, Kirkby SE, Tobias JD, McKee C. Safety of endoscopic sinus surgery in children with cystic fibrosis. International Journal of Pediatric Otorhinolaryngology 2017; 98:25-8. [ Links ]
5. Liang J, Higgins TS, Ishman SL, Boss EF, Benke JR, Lin SY. Surgical management of chronic rhinosinusitis in cystic fibrosis: a systematic review. International Forum of Allergy & Rhinology 2013; 3:814-22. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
João Rio Martins
Pediatric Cystic Fibrosis Center Hospital Pediátrico de Coimbra
Centro Hospitalar e Universitário de Coimbra Av. Afonso Romão
3000-602 Coimbra
Email: joaoriomartins@gmail.com
Received for publication: 01.08.2018
Accepted in revised form: 16.01.2019