Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Nascer e Crescer
versão impressa ISSN 0872-0754versão On-line ISSN 2183-9417
Nascer e Crescer vol.28 no.4 Porto dez. 2019
https://doi.org/10.25753/BirthGrowthMJ.v28.i4.15728
CASE REPORTS | CASOS CLÍNICOS
Van Neck-Odelberg disease: a rare cause of childhood limping
Doença de Van Neck-Odelberg: uma causa rara de claudicação na infância
Joana FerreiraI, Maria Cristina GranadoI, Cláudia LemosII, Sara CunhaI, Teresa São SimãoI, Cristina FerreiraI, Cláudia NetoI
I Department of Pediatrics, Hospital Senhora da Oliveira. 4835-044 Guimarães, Portugal; joanaisabelferreira@hospitaldeguimaraes.min-saude.pt, mariagranado@hospitaldeguimaraes.min-saude.pt, saracunha@hospitaldeguimaraes.min-saude.pt, teresapinto@hospitaldeguimaraes.min-saude.pt, cristinaferreira@hospitaldeguimaraes.min-saude.pt, claudianeto@hospitaldeguimaraes.min-saude.pt
II Department of Pediatrics, Centro Materno-Infantil do Norte, Centro Hospitalar Universitário do Porto. 4050-651 Porto, Portugal. claudialemos@hospitaldeguimaraes.min-saude.pt
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Introduction: Joint pain and limping are common in pediatric age. Assessment of a child with joint pain requires differentiating benign conditions from those requiring urgent medical attention.
Case report: A previously healthy nine-year-old boy was brought to the Emergency Department with fever and pain in the left ankle and hip associated with limping. He reported fever, abdominal pain, and slightly dry cough two weeks before admission.
Blood analysis revealed an elevation in erythrocyte sedimentation rate and C-reactive protein serum concentration. Serology tests were positive for Mycoplasma pneumoniae acute infection and imaging studies enabled the diagnosis of Van Neck-Odelberg disease (VND).
Discussion/Conclusion: Presence of joint pain often represents a diagnostic challenge, especially in children who present with fever and elevation of acute-phase reactants. VND is a rare cause of limping and in this case corresponded to an imaging finding. The final diagnosis was reactive arthritis secondary to M. pneumoniae infection.
Keywords: hip; joint pain; M. pneumoniae; Van Neck-Odelberg
RESUMO
Introdução: A dor articular é uma queixa comum em idade pediátrica. A sua investigação é fundamental para distinguir situações benignas daquelas que necessitam de intervenção médica urgente.
Caso Clínico: Uma criança de nove anos, previamente saudável, foi conduzida ao Serviço de Urgência devido a um quadro de febre e dor no tornozelo e anca esquerdos associado a claudicação. A criança referiu febre, dor abdominal e tosse seca duas semanas antes da hospitalização. O estudo analítico demonstrou elevação da velocidade de sedimentação eritrocitária e da proteína C-reactiva. O estudo serológico foi positivo para infeção aguda por Mycoplasma pneumoniae e o estudo imagiológico possibilitou o diagnóstico de doença de Van Neck-Odelberg (VND).
Discussão/Conclusão: A presença de dor articular geralmente representa um desafio diagnóstico, especialmente em crianças que se apresentam com febre e elevação de reagentes de fase aguda. A VND é uma causa rara de claudicação e neste caso correspondeu a um achado imagiológico. Foi estabelecido o diagnóstico final de artrite reativa secundária a infeção por M. pneumoniae.
Palavras-chave: anca; dor articular; M. pneumoniae; Van Neck-Odelberg
Introduction
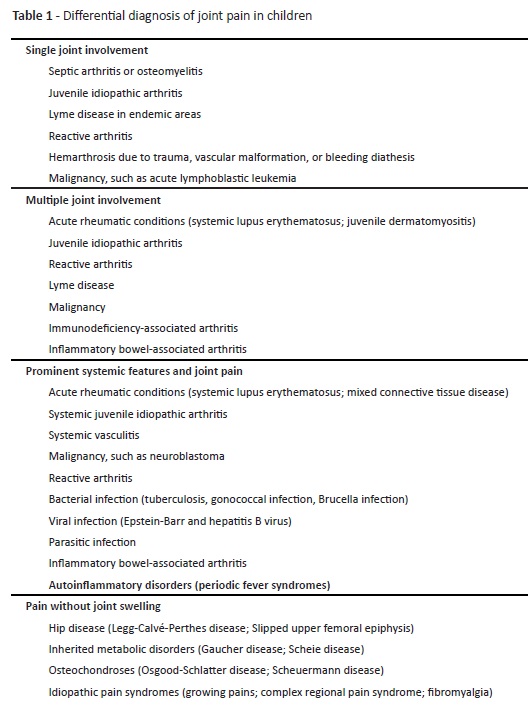
Joint pain in children is a common manifestation of different possible musculoskeletal and rheumatological conditions. Usually, there is an overlap between causes of joint pain, hip pain, and limping.1 The child’s history and examination should be focused on distinguishing between benign and severe causes as a way of determining the appropriate laboratory and radiographic evaluation. Table 1 includes the most common disorders to be considered in children with joint pain.
Several studies and review articles have reported that joint manifestations can occur secondary to bacterial or viral infections and are generally accepted to be reactive.2 Mycoplasma pneumoniae is one possible etiological agent, usually considered a triggering factor.3,4 The term reactive arthritis (ReA) refers to the occurrence of non-purulent arthritis complicating an infection at a distant site in the body. Usually, the previously healthy young patient acquires an infection and, within days or weeks, develops arthritis at a distant site that is commonly asymmetrical and oligoarticular, usually on the lower extremities or sacroiliac joints.5
VND is a poorly known entity characterized by enlargement of the ischiopubic synchondrosis (IPS) that should be acknowledged in the differential diagnosis of groin or hip pain in prepubertal age. Few reports of this condition are available and it can be easily mistaken for other entities, particularly osteomyelitis or malignancies. It is often considered a diagnosis of exclusion, as laboratory values are usually normal and routine radiographic workup may be nonspecific.6
Here in is reported a case of ReA related to Mycoplasma pneumoniae infection associated with Van Neck-Odelberg disease, in which clinical, laboratory and imaging findings enabled the final diagnosis.
Case report
A nine-year-old boy was brought to the Emergency Department with a four-day history of low fever (axillary temperature of 38ºC) associated with pain in the left ankle and hip, with a limp that was keeping the child away from his normal activities. No history of trauma or physical effort and no constitutional symptoms like anorexia or weight loss were reported. The boy had experienced fever, abdominal pain, and slightly dry cough two weeks before admission, after which he was well for a few days. Personal and family history were unremarkable. On physical examination, the left hip and ankle were painful on movement and slight edema and raised local temperature were evident around the ankle. No other joints seemed to be affected. Vital signs were within normal range and the boy had no neurological dysfunction. No lesions or regional lymphadenopathy were observed. Complete blood count revealed 13.800 white blood cells/μL with 9.800/μL neutrophils, 2800/μL lymphocytes, 900/μL monocytes; hemoglobin level of 11.1 g/dL; and platelet count of 472.000/μL. Erythrocyte sedimentation rate (ESR) was raised to 76 mm/hour (reference value, 0−10 mm/hour) and C-reactive protein (CRP) serum concentration to 37.5 mg/L (reference value, <2.9 mg/L). The remaining laboratory tests, including serum electrolytes, blood glucose, ionogram, and calcium and phosphorus levels were within the normal range. Coagulation tests (including prothrombin time and activated partial thromboplastin time), group A screening test and antistreptolysin O titer were also normal.
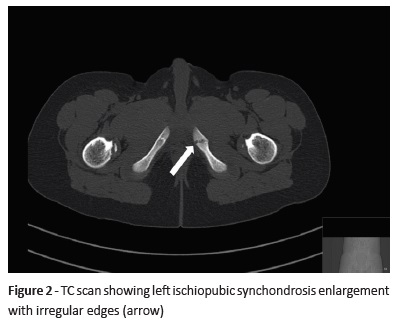
Plain radiography of the ankle and lumbar spine were normal. Chest radiography showed peribronchial and perivascular interstitial infiltrate. On pelvic radiography, a sclerotic shadow was observed in the left ischiopubic region (Figure 1). To better characterize the radiographic changes observed, a computerized tomography (CT) scan was performed, suggesting a left ischiopubic branch “fracture in consolidation” (Figure 2). No identifiable fractures were observed in the proximal femurs or remaining pelvic bones, nor fluid or solid masses were noted in the soft tissues evaluated. Ultrasonography of the affected joints was not performed since it was not accessible at the time. The patient initiated anti-inflammatory therapy (naproxen) and bed rest and was hospitalized for further etiological study. The differential diagnosis included inflammatory, infectious, neoplastic, and autoimmune disorders (including celiac disease). Chronic entities (such as juvenile idiopathic arthritis) and extrinsic causes secondary to abdominal processes were also considered.
Full investigation included biochemical markers of iron status (serum iron, ferritin, transferrin, transferrin saturation, iron-binding capacity); hepatic function panel (aspartate aminotransferase, alanine aminotransferase, bilirubin, alkaline phosphatase, ammonia, serum immunoglobulins [IgA, IgG, IgM], alfa-fetoprotein), and autoimmune markers (antinuclear antibodies, rheumatoid factor, anti-ds DNA antibodies, C3, C4, and CH50), which were all normal. Screening for celiac disease (anti-transglutaminase, anti-gliadin antibodies) was also performed and turned out negative. Serum antibodies, anti-herpes simplex virus 1 and 2, Adenovirus, Cytomegalovirus, Borrelia burgdorferi, Brucella melitensis, and Epstein-Barr virus were also negative. Screening for M. pneumoniae IgM and IgG antibodies was performed by enzyme-linked immunosorbent assay (ELISA) and immunoglobulin concentrations higher than 10 U/ml were considered positive. Evidence of an IgM titer of 27 U/mL and an IgG titer of 4.7 U/mL enabled the diagnosis of acute infection and a macrolide (azithromycin) was added to the anti-inflammatory treatment.
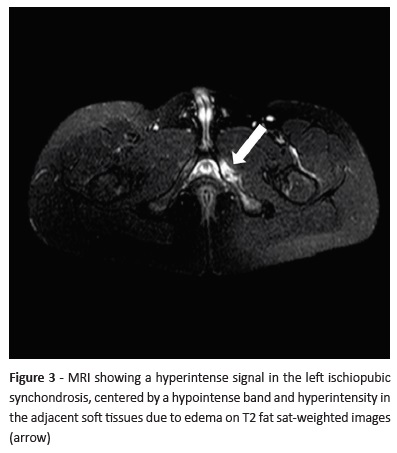
Blood culture was negative. Abdominal ultrasound was also normal. Magnetic resonance imaging (MRI) showed irregularity of both joints of the left ischiopubic synchondrosis coexisting with a slight volumetric increase, as well as discrete bone resorption in its articular surface with moderate marrow edema and mild inflammatory changes of adjacent soft tissues (Figure 3). In the absence of previous trauma history, these alterations were consistent with the diagnosis of Van Neck-Odelberg disease.
Clinical and laboratory evolution was favorable. Within 24 hours, the child became afebrile and after 72 hours complete symptom resolution was evident. Laboratory tests showed a progressive decrease in ESR and CRP values. The patient was discharged on day 8, asymptomatic, after completing five days of antibiotic treatment.
The serological test for M. pneumoniae was repeated three weeks after discharge, showing a fourfold increase in IgG titer and confirming infection. The child is undergoing orthopedic and pediatric follow-up for the last six months and remains asymptomatic until present.
Discussion
Mycoplasma pneumoniae is a well-recognized respiratory pathogen mainly affecting children and young adults. This organism is also responsible for producing a wide spectrum of extra-pulmonary manifestations.3,4 A large number of Mycoplasma species cause acute or chronic arthritis in different animal species via one of the “superantigens”.7,8 However, it remains uncertain whether they elicit the immunopathological process through molecular mimicry or modulation of the immune response via immune cell activation and cytokine production causing a cytokine imbalance (predominant type II response).9
ReA diagnosis in pediatric patients has been mostly established in children developing arthritis after a specific episode of infection or in those with a positive serological test against bacteria.2 In this report, the authors describe the case of a patient who presented with ReA secondary to acute M. pneumoniae infection, predominately affecting ankle and hip joints. The final diagnosis was based on clinical features (asymmetric oligoarthritis involving two joints, in absence of evidence for other defined disease) along with elevated erythrocyte sedimentation rate and C-reactive protein and positive serological test, and after excluding other serious conditions. We believe that the low fever and elevation of acute phase reactants observed can be explained by M. pneumoniae infection.
In the reported case, the patient had gastrointestinal and respiratory symptoms preceding ReA, which may be relevant for clinical practice and emphasize the importance of serological screening in these cases. The patient was observed at an early stage of disease, and the non-steroidal anti-inflammatory therapy along with antibiotic therapy proved effective. However, at present, it is not clear whether appropriate antibiotic therapy can change the course of M. pneumoniae-induced ReA.
In this case, VND diagnosis was established following an imaging finding. As reported in the literature, unbalanced mechanical stress, such as kicking or jumping, may induce an inflammatory reaction and a delayed complete IPS ossification.6,10,11 This finding is currently considered a normal physiologic ossification pattern, frequently showing an age correlation. Its tumor-like appearance on conventional radiographic exam may be mistaken for stress fractures, tumors, or inflammation. Radiography and CT scan usually show an increased size, with lucency and sclerosis. Presence of marrow edema around the IPS, along with absence of surrounding myositis, abscess, and free fluid on MRI, are reliable findings that may confirm diagnosis, as in the present case.11 However, it should be emphasized that this is an exclusion diagnosis and in presence of other signs or symptoms, including fever or abnormal laboratory findings, the patient’s condition should be further investigated.
Conclusion
Joint symptoms are well acknowledged in M. pneumoniae infection, especially in pediatric patients. However, the differential diagnosis for joint pain in children is broad, ranging from benign to serious conditions, some of which can have devastating consequences. With this case, the authors wish to reinforce the need to investigate and exclude serious conditions in children presenting with joint pain, hip pain, or limping and image findings suggestive of VND, especially in presence of other associated symptoms, such as fever and inflammation.
REFERENCES
1. Kimura Y, Southwood T. Evaluation of the child with joint pain and/or swelling. [Accessed january 1, 2019]. Available at https://www.uptodate.com. [ Links ]
2. Harjacek M, Ostojic J, Rode O. Juvenile spondyloarthropathies associated with Mycoplasma pneumoniae infection. Clin Rheumatol 2006; 25:470-5. [ Links ]
3. Sanchez-Vargas FM, Gomez-Duarte OG. Mycoplasma pneumoniae-an emerging extra-pulmonary pathogen. Clin Microbial Infect 2008; 14:105-17. [ Links ]
4. Narita M. Pathogenesis of extrapulmonary manifestations of Mycoplasma pneumoniae infection with special reference to pneumonia. J Infect Chemother 2010; 16:162-9. [ Links ]
5. Sztajnbok1 F, Fonseca A, Campos L. Espondiloartropatias juvenis. Revista Adolescência e Saúde. 2004; 1:6-9. [ Links ]
6. Wait A, Gaskill T, Sarwar Z, Busch M. Van neck disease: Osteochondrosis of the ischiopubic synchondrosis. J Pediatr Orthop 2011; 31:520-4. [ Links ]
7. Kvien TK, Glennas A, Melby K, Granfors K, Andrup O, Karstensen B, et al. Reactive arthritis: incidence, triggering agents and clinical presentation. J Rheumatol 1994; 21:11522. [ Links ]
8. Cole BC. Mycoplasma interactions with the immune system: implications for disease pathology. ASM News 1996; 62:47175. [ Links ]
9. Burmester GR, Daser A, Kamradt T, Krause A, Mitchison NA, Sieper J, et al. Immunology of reactive arthritides. Annu Rev Immunol 1995; 13:229-50. [ Links ]
10. Keats TE. Plain film radiography: Sources of diagnostic errors. In: Resnick D, editor. Diagnosis of Bone and Joint Disorders. 3rd ed. San Diego: Saunders; 1996; p. 27. [ Links ]
11. Herneth AM, Trattnig S, Bader TR, Ba-Ssalamah A, Ponhold W, Wandl-Vergesslich K, et al. MR imaging of the ischiopubic synchondrosis. Magn Reson Imaging. 2000; 18:519-24. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Joana Ferreira
Department of Pediatrics
Hospital Senhora da Oliveira
Rua dos Cutileiros, Creixomil
4835-044 Guimarães
Email: joanaisabelferreira@hospitaldeguimaraes.min-saude.pt
Received for publication: 25.11.2018
Accepted in revised form: 28.03.2019