Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Nascer e Crescer
versão impressa ISSN 0872-0754versão On-line ISSN 2183-9417
Nascer e Crescer vol.29 no.1 Porto jan. 2020
https://doi.org/10.25753/BirthGrowthMJ.v29.i1.15709
CASE REPORTS | CASOS CLÍNICOS
Insulin-induced edema in a pediatric patient - clinical case
Edema insulínico em idade pediátrica - caso clínico
Catarina Ferraz de LizI, Joaquim CunhaI, Susana LiraI
I. Department of Pediatric and Neonatology, Centro Hospitalar do Tâmega e Sousa. 4560-136 Penafiel, Portugal. catarina.liz@gmail.com; jac321@sapo.pt; susanacosta.lira@gmail.com
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Introduction: Insulin edema is a rare condition associated with improved glycemic control shortly after diabetes diagnosis or following a period of insulin omission. Clinical findings range from mild edema to severe heart failure and pleural effusion. Diagnosis is clinical and other edema causes should be excluded. Since it is a self-limited condition, there is no need to modify insulin regimen. In more severe cases, diuretic therapy may be required.
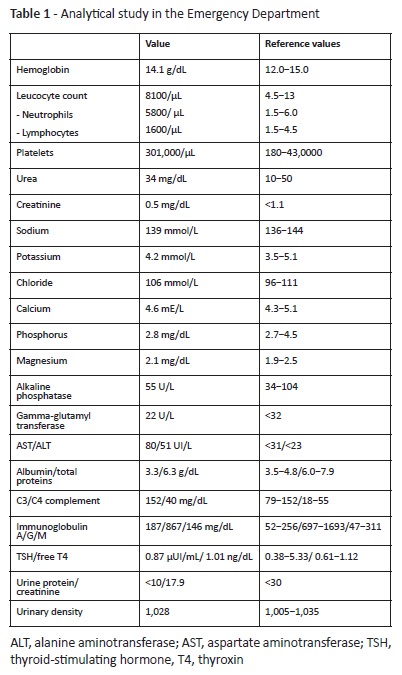
Clinical case: A 14-year-old female was brought to the Emergency Department due to weight gain and leg swelling with three days of evolution. She had been diagnosed with type 1 diabetes at the age of nine. The girl had poor metabolic control which led to multiple hospitalizations, the last one occurring the week before with a glycated hemoglobin higher than 15%. In physical examination, lower limb edema and a 7-kg weight gain were noted. No jugular vein distension, hepatomegaly, or other forms of edema were found. The girl was hemodynamically stable, with diuresis within the normal range. Analytical study consisting of hemogram, ionogram (sodium and potassium), and renal and hepatic function was normal. Urine analysis revealed glycosuria and chest x-ray showed no abnormalities.
The diagnosis of insulin-induced edema was established and water and saline restriction recommended, with total symptom resolution three weeks later.
Conclusion: Despite rare, clinicians should be aware of this condition, as most cases do not require modifying the insulin regimen.
Keywords: children and adolescents; complication; diabetes mellitus type 1; insulin; edema
RESUMO
Introdução: Edema insulínico é uma entidade rara associada a melhoria do controlo glicémico logo após o diagnóstico de diabetes ou após um período de omissão de insulina. Os achados clínicos variam de edema leve a casos graves de insuficiência cardíaca e derrame pleural. O diagnóstico é clínico e devem ser excluídas outras causas de edema. Tratando-se de uma condição auto-limitada, não é necessário modificar o esquema de insulina. Em casos mais graves, pode ser necessária terapêutica com diuréticos.
Caso clínico: Uma adolescente de 14 anos de idade foi levada ao Serviço de Urgência por aumento de peso e edema dos membros inferiores com três dias de evolução. Como antecedentes, a jovem tinha sido diagnosticada com diabetes tipo 1 aos nove anos de idade. Mantinha um mau controlo metabólico com necessidade de múltiplas hospitalizações, a última das quais na semana anterior com um valor de hemoglobina glicosilada superior a 15%. No exame físico, observou-se edema dos membros inferiores e ganho ponderal de sete quilos. Não foi observada turgescência da veia jugular, hepatomegalia ou outras formas de edema. A doente encontrava-se hemodinamicamente estável, com diurese dentro do normal. O estudo analítico que incluiu hemograma, ionograma e função renal e hepática foi normal. A análise de urina revelou glicosúria com densidade urinária normal e a radiografia de tórax não mostrou alterações. Foi estabelecido o diagnóstico de edema induzido por insulina e recomendada restrição hídrica e salina. Após três semanas, a doente apresentava resolução completa da sintomatologia.
Conclusão: Apesar de rara, os clínicos devem estar atentos a esta condição, pois na maioria dos casos não requer modificação do esquema insulínico.
Palavras-chave: crianças e adolescentes; complicação; diabetes mellitus tipo 1; insulina; edema
Introduction
Insulin-induced edema is a rare condition, with only a few cases described in the literature in children and adolescents.1
The condition occurs as a complication of type 1 or type 2 diabetes, associated with improved glycemic control shortly after diagnosis or following a period of insulin omission.1,2
Clinical findings range from mild edema, mostly in the lower extremities, to anasarca. In rare cases, more severe findings, such as heart failure, pleural effusion, and nephrotic syndrome, have been described.1,2
Diagnosis is clinical and established after exclusion of other edema causes, including cardiac, hepatic, or renal disease.
This is a self-limited condition, with no need for additional therapy in most cases. Fluid and salt restriction can be helpful and, in more severe cases, diuretic therapy can be administered.
Herein is reported a case of insulin-induced edema in a 14-year-old girl with a history of poor metabolic control.
Clinical Case
A 14-year-old caucasian female, from a nuclear family, living in a rural area, was diagnosed with type 1 diabetes at the age of nine and treated with insulin glargine and insulin lispro.
Poor metabolic control led to multiple hospitalizations, with the girl being admitted to the hospital one week earlier due to insulin administration omissions and a mean glucose value of 275 mg/dL. She presented with weight loss and polydipsia and was moderately dehydrated. Blood gas analysis revealed metabolic acidosis (pH 7.25, HCO3 16.7 mmol/L) and glycated hemoglobin (HgbA1c) was higher than 15%. During hospital stay, the girl showed good clinical evolution, with metabolic disorder correction, and was discharged five days after, reaching 51.5 kg of weight (Body Mass Index [BMI] 21 kg/m2). She maintained the same insulin treatment with a 1 U/kg/day total insulin dosage (40% basal and 60% bolus − insulin sensitivity factor of 30 and insulin to carbohydrate ratio of 1/10).
Five days later, the girl was brought to the Emergency Department due to weight gain and leg swelling with three days of evolution. She maintained the same treatment and no insulin dosages had been missed. Mean glucose level in the previous week was 125 mg/dL. The girl denied fever, shortness of breath, urinary or gastrointestinal symptoms and had no known drug allergies.
Physical examination was irrelevant, with stable vital signs (temperature 36.4ºC, heart rate 72 bpm, blood pressure 112/77 mmHg, respiratory rate 15 bpm with 98% oxygen saturation). Bilateral pitting edema of the lower limbs was evident up to the knee. Additionally, the girl had a 7-kg weight gain in the last five days (weight 58.5 kg, height 156 cm, BMI 24 kg/m2). No other inflammatory signs were present.
No jugular vein distension, hepatomegaly, ascites, or other forms of edema were found.
Analytical study (hemogram, ionogram, renal, hepatic and thyroid function) showed no alterations besides mildly raised aminotransferases (Table 1). Urine analysis revealed glycosuria with normal density and protein-to-creatinine ratio. Chest x-ray showed no abnormalities.
The girl presented a 2.3 mL/kg/day diuresis and was hemodynamically stable.
Considering the patient’s poor metabolic control and excluding other edema causes, the case was interpreted as insulin-induced edema and the patient was discharged with recommendation of water and saline restriction.
The girl was re-evaluated three weeks later, with total symptom resolution and improved glycemic control.
Discussion
Insulin-induced edema is a rare and underdiagnosed complication of diabetes.3
Most cases are reported in adults with type 1 or 2 diabetes. The first case described in children was in 1979, with sporadic reports published since.2,4
The pathophysiological mechanism remains unclear, with numerous contributing factors. Increased capillary permeability caused by chronic hyperglycemia leads to transcapillary loss of albumin, causing hypovolemia. Another determinant factor is insulin regulatory role in reducing salt and water renal excretion through Na+-K+-ATPase and Na+/H+ exchanger present in proximal tubules. In a volume-depleted state, increased insulin levels − particularly associated with intensive fluid resuscitation − induce renal reabsorption of sodium and free water, leading to edema. Insulin therapy leads to hyperaldosteronism, potentially also contributing to edema. Other theories propose that fluid accumulation is secondary to rapid glycogen deposition. Furthermore, glycemic control improvement causes a decrease in plasma osmolarity, resulting in intracellular water retention.1,5-10
In patients with type 1 diabetes, this condition is mostly described shortly after initial diagnosis. In the present case, the patient had been diagnosed at the age of nine, with adherence to insulin regimen and improved glycemic control as determinant factor.1,8
Diagnosis is established after exclusion of other edema causes, such as nephrotic syndrome and cardiac or liver failure. This patient had no chest pain or shortness of breath. In physical examination, cardiac and pulmonary examination were normal. Chest x-ray showed no abnormalities, excluding cardiac etiology. Hepatic disease was ruled out due to absence of jaundice and hepatomegaly. Since liver function (albumin and total protein) were normal, mildly raised aminotransferase was interpreted as resulting from metabolic decompensation five days earlier. Serum urea and creatinine were both normal and no proteinuria was found, with a normal protein-to-creatinine ratio excluding renal disease. Thyroid function was determined to rule out hypo or hyperthyroidism and insulin-induced edema diagnosis was subsequently established.
Insulin-induced edema is mostly a benign condition, with complete resolution achieved in few weeks without specific treatment. Water and salt restriction are often recommended, but there is no need to modify the insulin regimen. Use of diuretics has been described in severe cases with cardiac failure or pleural effusion, with these patients requiring closely monitoring due to increased risk of complications.8-10
The reason why only some patients develop this complication is yet to be determined. With increased use of insulin pumps in patients with poor metabolic control, incidence of this complication will probably increase in the future.11,12
Despite rare in pediatric age, insulin-induced edema should be considered after exclusion of more common edema causes. The condition results from rapid glycemic improvement shortly after diagnosis or after poor metabolic control. In these cases, gradual insulin increase together with glycemic control may prevent the complication. Diuretic therapy should be used in severe cases of anasarca.
REFERENCES
1. Aravamudhan A, Gardner C, Smith C, Senniappan S. Insulin oedema in a child with newly diagnosed diabetes mellitus. European Journal of Pediatrics. 2013; 173:685-7. [ Links ]
2. Adamo L, Thoelke M. Generalised insulin oedema after intensification of treatment with insulin analogues. BMJ Case Rep. 2013; 2013: bcr2012007037. [ Links ]
3. Chaker F, Yazid M, Chihaoui M, Rached A, Slimane H. Insulin-Induced Edema: An Unusual Complication in a Patient With Diabetic Ketosis. Tunis Med. 2017; 95:142-4. [ Links ]
4. Lawrence JR. Diabetic (insulin) oedema. BMJ. 1979; 2:445. [ Links ]
5. Kan Y, Anno T, Kawasaki F, Takai M, Shigemoto R, Kaneto H, et al. Bilateral lower limb edema induced by rapid improvement of glycemic control with insulin therapy in a subject with poorly controlled type 2 diabetes. Acta Diabetologica. 2017; 54:611-3. [ Links ]
6. Klisic J, Hu M, Nief V, Reyes L, Fuster D, Moe O, et al. Insulin activates Na+/H+ exchanger 3: biphasic response and glucocorticoid dependence. American Journal of Physiology-Renal Physiology. 2002; 283:F532-9. [ Links ]
7. Kalambokis G, Tsatsoulis A, Economou G, Tsianos E. A case of insulin edema with inappropriate hyperaldosteronism. Journal of Endocrinological Investigation. 2004; 27:957-60. [ Links ]
8. Chelliah A, Burge MR. Insulin edema in the twenty-first century: review of the existing literature. J Investig Med 2004; 52:104-8. [ Links ]
9. Goturu A, Jain N, Lewis I. Bilateral cataracts and insulin oedema in a child with type 1 diabetes mellitus. Case Reports. 2013; 2013:bcr2012008235. [ Links ]
10. Bas V, Cetinkaya S, Yilmaz Agladioglu S, Peltek Kendirci H, Bilgili H, Yildirim N, et al. Insulin Oedema in Newly Diagnosed Type 1 Diabetes Mellitus. Journal of Clinical Research in Pediatric Endocrinology. 2010; 2:46-8. [ Links ]
11. Greco D. Severe Weight Gain and Generalized Insulin Edema after the Starting of an Insulin Pump. Canadian Journal of Diabetes. 2015; 39:21-3. [ Links ]
12. Rothacker K, Kaye J. Insulin oedema and treatment-induced neuropathy occurring in a 20-year-old patient with Type 1 diabetes commenced on an insulin pump. Diabetic Medicine. 2013; 31:e6-e10. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Catarina Ferraz de Liz
Department of Pediatric and Neonatology
Centro Hospitalar do Tâmega e Sousa
Avenida do Hospital Padre Américo, Nº 210
4560-136 Guilhufe - Penafiel
Email: catarina.liz@gmail.com
Received for publication: 24.11.2018
Accepted in revised form: 11.06.2019