Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Nascer e Crescer
versão impressa ISSN 0872-0754versão On-line ISSN 2183-9417
Nascer e Crescer vol.29 no.2 Porto jun. 2020
https://doi.org/10.25753/BirthGrowthMJ.v29.i2.17896
REVIEW ARTICLES | ARTIGOS DE REVISÃO
Anaphylaxis in pediatric age: an overview
Anafilaxia em idade pediátrica: uma visão global
Maria Luís MarquesI, Joana GouveiaI, Inês Machado CunhaI, Eva Rebelo GomesI
I. Department of Allergy and Clinical Immunology, Centro Hospitalar Universitário do Porto. 4099-001 Porto, Portugal. maluis234@gmail.com; joanamngouveia@gmail.com; inesrjmcunha@gmail.com; evamariasrg@gmx.com
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Anaphylaxis is defined as an acute severe, life-threatening hypersensitivity reaction. The condition’s real prevalence and incidence are difficult to estimate, but seem to be increasing, particularly in children. Anaphylaxis clinical presentation varies according to age and other individual factors. Although consensual clinical criteria exist, including in pediatric age, diagnosis can be challenging. Food allergy is the most common anaphylaxis cause in children, particularly in preschool age. Drug-induced reactions and hymenoptera venom sting are other major triggers, which importance increases after adolescence. Management involves diagnosis, appropriate identification of possible triggers, acute phase treatment, and long-term planning. Prompt referral to a Pediatric Allergy specialist is recommended, as complete allergy workup is usually required to implement future preventive measures. In this review, the authors discuss particular aspects regarding anaphylaxis in pediatric age to provide information that can help improve disease management.
Keywords: Adolescence; anaphylaxis; children; epinephrine; systemic allergic reaction
RESUMO
A anafilaxia define-se como uma reação de hipersensibilidade aguda grave, que pode estar associada a risco de vida. A sua prevalência e incidência são difíceis de estimar, mas parecem estar a aumentar, sobretudo na faixa etária pediátrica. A apresentação clínica da anafilaxia varia de acordo com a idade e fatores individuais. Apesar de existirem critérios clínicos já estabelecidos, inclusive em idade pediátrica, o diagnóstico desta entidade pode ser difícil. A alergia alimentar é a causa mais comum de anafilaxia em idade pediátrica, especialmente em idade pré-escolar. As reações desencadeadas por fármacos e por veneno de himenópteros são também importantes, sendo que a sua relevância vai aumentado depois da adolescência. A abordagem desta condição envolve o diagnóstico, identificação apropriada dos agentes implicados, tratamento de fase aguda e planificação da abordagem a longo prazo. A referenciação rápida para um Imunoalergologista é recomendada, uma vez que o estudo alergológico é fundamental para a implementação de medidas preventivas. Nesta revisão, os autores discutem aspetos da anafilaxia em idade pediátrica, com o objetivo de fornecer informação que possa otimizar a abordagem desta entidade.
Palavras-Chave: Adolescência; adrenalina; anafilaxia; crianças; reação alérgica sistémica
Introduction
Anaphylaxis is a clinical emergency that should be promptly recognized to avoid acute treatment delays. The most commonly used anaphylaxis grading classification was proposed by Ring and Messmer1 and considers four grades, with grade IV accounting for the most serious reactions with respiratory or cardiovascular arrest. Several criteria have been established to help diagnosis and classify disease severity. However, diagnosis can be challenging, and this is particularly true in pediatric age. All patients should be referred to formal workup to identify potentially avoidable triggers and prevent future reactions. Most common triggers vary between adults and children and this should be considered during diagnostic workup.
In this article, the authors review current anaphylaxis general concepts and focus on specific pediatric aspects of diagnosis, management, and treatment.
Epidemiology
Anaphylaxis is defined as an acute, potentially life threatening systemic hypersensitivity reaction occurring without warning.2-4 Although major efforts have been done over the last decades to establish an unanimous case definition and diagnostic criteria, implementation of a standardized clinical practice approach remains a significant challenge.5 As a consequence, underdiagnosis and underreporting remain well-acknowledged problems. Additionally, tools currently used to report anaphylaxis (ICD-9, ICD-10, and ICD-11) still lack sensitivity and specificity.
Anaphylaxis epidemiological data is retrieved from several sources, including Emergency Departments (EDs), regional and national databases, and health organizations.6
The real prevalence and incidence of pediatric anaphylaxis are difficult to estimate. In 2006, the National Institute of Allergy and Infectious Disease and the Food Allergy and Anaphylaxis Network (NIAID-FAAN) established criteria for diagnosis of anaphylaxis, after which several studies have been published, including regarding anaphylaxis incidence and prevalence in pediatric age.5,7-16
Based on recent publications, the estimated overall anaphylaxis incidence ranges between 50−112 episodes per 100.000 person-years, and the estimated prevalence between 0.3−5.1%.6 Lifetime anaphylaxis prevalence has been estimated to vary between 0.5−2%.16
In Sweden, a population-based case study of ED visits examined 385 records of children aged 0−18 years and estimated a total food anaphylaxis incidence of 32 per 100.000 person-years in this age group.15 In a Spanish study conducted by Alonso T et al including 325.046 people, a peak incidence of 313.58 per 100.000 person-years was reported in the 0−4-year-old age group, which was significantly higher (p <0.05) compared with other age groups.8 In the UK, a review of 816 of 401.152 (0.2%) ambulance calls due to anaphylaxis revealed that 180 (22%) cases occurred in children.17
Incidence, prevalence, and relevance of anaphylaxis triggers seem to vary according to age, gender, geographic area, healthcare access, among other factors. While foods are the most commonly implicated anaphylaxis triggers in young children, drugs are consistently found to be the most frequent triggers in adolescents and adults.6,18-21
The European Anaphylaxis Registry resulted from a multicenter study conducted in 10 European countries which analysed information on anaphylactic reactions through a web-based data entry system including 1970 anaphylaxis events in pediatric patients (1865 with known elicitors). The study found that foods were the most common elicitors (69.2%), followed by hymenoptera stings (20.4%) and drugs (5.4%).12 Drugs accounted for only 3.1% of anaphylaxis events in preschoolers aged <6 years, 4.1% in children aged 6−12 years, and 12.1% in adolescents aged 13−17 years. Analgesics were the most frequently implicated drugs.12
Among children, males seem to be particularly affected, as they represent 57−70% of all pediatric cases, but among adults, women are more prone to suffer from an anaphylactic event.13,22,23 Pre-school children (0−4 years) seem to be more affected, with a threefold higher incidence compared with other age groups, as recently reported in one Spanish and one Australian study.7,24
Fatal anaphylaxis in pediatric age seems to be rare.5,12,25,26 As described by Liew et al, death from anaphylaxis is generally preceded by non-fatal anaphylaxis.26 The most frequent elicitors in fatal cases are foods, especially cow milk, hazelnut, and peanut.6 According to European Anaphylaxis Registry data, approximately 1.3% (26 in 1970) of children in pediatric age experienced life-threatening or fatal reactions, all having food as trigger: 11 experienced Ring and Messmer classification grade III reactions with Intensive Care Unit (ICU) admission; 10 experienced grade IV symptoms, three of which requiring ICU admission, one requiring treatment by a family member and another by an emergency doctor, and five with no information; and five died.12
ED visits and hospitalizations due to anaphylaxis seem to be increasing over the last decade, including in children.9 In Spain, a 1.89-fold increase in anaphylactic events was reported between 1998−2011, particularly among children under 14 years of age.27 In the USA, a recent study reported a fourfold increase in emergency admissions and in the UK admission rates increased from 0.5 to 3.6/100.000 persons per year between 1991 and 2001.24,28 In Australia, an analysis comparing 1993−1994 and 2004−2005 anaphylaxis events found an increase from 4.5 to 8.2/100.000 persons per year, which was particularly prominent in children aged between 5−14 years old.29
Causative agents and risk factors
According to last findings from the European Anaphylaxis Registry, food-induced anaphylaxis is the most common entity in children and adolescents, accounting for 66% of cases. Other less frequent causes include insect bites/stings (19%) and drug allergy (5%). Relevance of each trigger varies according to age; for example, 88% of preschoolers suffer from food-induced anaphylaxis, followed by 13% with drug-induced anaphylaxis, and 7% with insect sting bite anaphylaxis. Relevance of drug-induced and insect sting bite anaphylaxis increases with age, accounting for 22% and 16% of adolescent cases, respectively.12 Anaphylaxis due to specific aeroallergen immunotherapy administration has also been reported, with a predictable increase in the number of iatrogenic anaphylaxis events with the increasing number of food desensitization protocols.20,30-32 The first European case of fatal anaphylaxis during an oral food challenge involved a three-year-old boy and occurred in 2017.33 Anaphylaxis from non-immunologic triggers is less common, but cases have been reported associated with cold, exercise, heat, and some medications such as opioids.34 In children, cold anaphylaxis is an important event that should be considered. It was reported in two Portuguese studies, with a significant 1.4−4.6% prevalence.11,35 Cold anaphylaxis seems to be present in one third of patients with cold-induced urticaria.36
Several reports suggest that approximately 20% of all anaphylaxis episodes are idiopathic.5
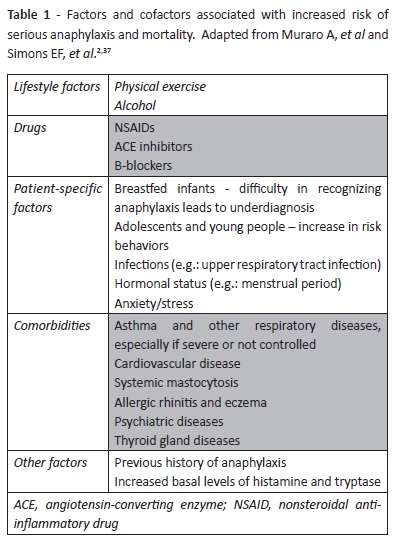
The main acknowledged risk factors and cofactors associated with anaphylaxis in pediatric age are described in Table 1.
Results
In pediatric populations, the main risk factors and cofactors associated with an increased anaphylaxis mortality risk are coexisting asthma − especially if severe or uncontrolled − and history of previous anaphylactic reactions.37,38
Cofactors such as physical exertion and nonsteroidal anti-inflammatory drug (NSAID) and/or alcohol intake have been associated with more serious events and can be particularly important among adolescents. Anaphylaxis associated with food intake in the context of physical exercise should be considered within the frame of a special entity, known as food-dependent exercise-induced anaphylaxis (FDEIA). In FDEIA, anaphylaxis onset during exercise is preceded by ingestion of the causal food allergen(s), while both food allergen ingestion and exercise are tolerated if done independently. Although uncommon, this diagnosis should be considered in cases of suggestive exercise-induced anaphylaxis.39
Clinical presentation and diagnosis
Although anaphylaxis definition is virtually unanimous, diagnosis is essentially clinical and diagnostic criteria vary according to different guidelines.2,5,37,38,40 It is a concern that many physicians still fail to recognize anaphylaxis and diagnose the condition and to evaluate its severity. A study conducted by Thomson et al evaluated ED presentation of 60.143 pediatric patients and identified 1.551 allergy-related episodes. Among those, 211 anaphylaxis events were identified (0.35% of all ED and 13.6% of ED allergy-related visits), but anaphylaxis diagnosis in ED was only established for 105 cases, the remaining 106 receiving an alternative diagnosis. The authors further identified 24 episodes that were classified as anaphylaxis without meeting established diagnostic criteria.41
This highlights the need of standardizing anaphylaxis clinical criteria as well as improving knowledge of healthcare professionals dealing with the condition.42
Primary diagnostic criteria include acute skin onset and/or mucosal symptoms, along with either respiratory compromise (e.g.: bronchospasm, stridor, shortness of breath), and/or gastrointestinal symptoms (e.g.: crampy abdominal pain, vomiting), and/or reduced blood pressure or end-organ dysfunction-associated symptoms (e.g.: hypotonia, syncope, incontinence).20 In cases of serum tryptase elevation, diagnosis may be supported within a few hours after reaction compared with patient baseline levels; however, in children, particularly with food-triggered reactions, levels are often normal.43
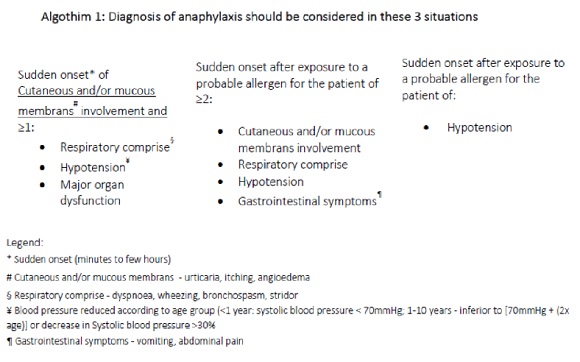
Three clinical scenarios should be considered when establishing an anaphylaxis diagnosis, which are described in Algorithm 1.1,4
Clinical history is the most important tool for diagnosis and etiology determination.
In a 2012 study describing a cohort of pediatric and adult anaphylaxis patients from Central Europe (German, Austria, and Switzerland), skin involvement was the most frequently reported symptom (84%), followed by cardiovascular symptoms (72%), and respiratory symptoms (68%).44 Another study reported clinical anaphylaxis manifestations according to age in a group of 605 children evaluated at ED for a period of six years. Although skin involvement is not mandatory in anaphylactic reactions, study authors found that it was predominant (≥85%) in all age groups (infancy, preschool age, school age, and adolescence).45
More than 50% of children presented with gastrointestinal symptoms and respiratory symptoms were present in more than 70% of cases, being particularly prevalent in preschool age (around 80%).35,46
Complete anamnesis is necessary in the diagnostic approach: symptom onset time, place/environment where the reaction occurred, number and characterization of past episodes, administered treatments, and all suspected causes and possible cofactors at the time of the episode.14,47 Dietary and drug intake, hymenoptera sting bite, latex contact, physical activity, and factors as cold, heat, and alcohol intake should always be investigated.14,38
Anaphylaxis diagnosis in infants can be challenging, and this difficulty may be related to several factors: difficulty in expressing complaints/describing signs; subjectivity in identifying signs and symptoms as part of anaphylaxis clinical presentation (e.g.: pruritus, nasal congestion, abdominal cramps or nausea, regurgitation, diarrhea, irritability, hoarseness, and dysphonia); and presence of easily recognizable but non-specific signs, such as generalized urticaria, sudden respiratory symptoms (e.g.: cough, choking and wheezing), or altered consciousness.48,49 In infants, recurrent vomiting, irritability, persistent crying and hypotonia, and hyporresponsiveness can be part of initial anaphylaxis presentation. Simple findings as irritability may correspond to cardiovascular system involvement in anaphylaxis in infants.46
Cardiovascular evaluation, including blood pressure and capillary refill time measurement, during anaphylaxis episodes seems to be neglected, particularly in infants, possibly due to difficulty in evaluating blood pressure in a crying and irritable infant.13,46 Factors as availability of appropriate-sized sphygmomanometer cuffs for infants may also be decisive.46
Symptoms are more specific in older children and adolescents, with cutaneous symptoms predominance, followed by respiratory and gastrointestinal manifestations.32,46
However, most fatal anaphylaxis events occur during adolescence, what can be partially explained by factors as less caregiver supervision, lack of responsibility and risk-taking behaviors.40,50,51 Cardiovascular symptoms seem to be more frequent (12%) in adolescents compared with children.45 Additionally, also exercise-related anaphylaxis (dependent or not on food ingestion) is more frequent at this age.37
The place where anaphylaxis episodes take place varies. Most occur at home, almost 30% on the outside, and 10−18% of allergic food reactions occur at school.35,52
Anaphylaxis diagnosis should be considered in all age groups and both acute urticaria and asthma attack should be considered in the differential diagnosis.2 In infants and preschoolers, respiratory distress is a common manifestation of several respiratory infections, like laryngitis, bronchiolitis, and foreign body aspiration. Gastrointestinal symptoms may be explained by several gastrointestinal conditions, including acute gastroenteritis, intestinal intussusception, appendicitis, protein-induced enterocolitis, and many others. Regarding neurological symptoms, seizures, post-ictal state, traumatic head injury, drug intoxication, and metabolic disease should be taken into account in differential diagnosis.48,49 Other important differential diagnoses, especially among adolescents, are panic attacks and vasovagal reactions, which can be accompanied by hypotension and are commonly associated with pallor and diaphoresis.14,38
Anaphylaxis emergency management
Anaphylaxis is a clinical emergency and healthcare professionals should be familiar with its recognition and management. Patients require immediate assessment using an Airway, Breathing, Circulation, Disability, and Exposure (ABCDE) approach. First-line treatment consists of intramuscular (IM) epinephrine and should be administered to all patients experiencing anaphylaxis. Epinephrine acts as an alphaand beta-adrenergic agonist, resulting in vasoconstriction and decreased mucosal edema. It has positive inotropic and chronotropic effects and induces bronchodilation and decreased mediator release from mast cells and basophils.37,53 In children, recommended epinephrine dose is 0.01 mg/kg (maximum 0.5 mg) of a 1:1000 (1 mg/mL) solution via IM injection into the mid-anterolateral thigh.14
Auto-injector epinephrine dosing is 0.15 mg for children weighing 10-25 kg and 0.3 mg for those weighing >25 kg.54 Repeated doses after five minutes are recommended in cases of suboptimal response or symptom progression.14,54 Intravenous epinephrine infusion or bolus should be considered in specific circumstances, such as severely hypotensive patients, patients in cardiac or respiratory arrest (together with cardiorespiratory resuscitation), and patients failing to respond to multiple IM epinephrine injections. In such cases, continuous hemodynamic monitoring is mandatory.14 Patients may experience self-limited adverse effects after epinephrine administration, such as pallor, tremor, anxiety, palpitations, dizziness, and headaches.
Second-line intervention
If possible, the likely anaphylaxis trigger should be immediately removed and help requested from the hospital emergency services or resuscitation team.37 Although it is generally recommended to place the patient in a recumbent position with lower extremities elevated, individuals experiencing respiratory distress (common in children) or vomiting should instead be placed in a comfortable position.2 Supplemental oxygen should be administered by face mask or oropharyngeal airway at a 6-8 L/min flowrate. Fluid administration with normal saline is also an appropriate starting measure. Children in shock may require up to 30 mL/kg of saline solution in the first hour.2,55 Although inhaled bronchodilators and inhaled nebulized adrenaline may be used as adjuncts for lower airway symptoms, they are not recommended in anaphylaxis for not relieving upper airway constriction or shock.51
H1-antihistamines are not recommended as initial anaphylaxis treatment because, despite decreasing urticaria and itching, they do not relieve life-threatening respiratory symptoms or shock. Although glucocorticoids can be used, as they potentially prevent biphasic anaphylaxis, their action onset takes hours and therefore are not drugs of choice for initial anaphylaxis treatment.2
After acute anaphylaxis therapy, patients should be kept under surveillance: those presenting with respiratory compromise should be closely monitored for at least 6-8 hours, and those presenting with hypotension for at least 12-24 hours. One of the reasons for maintaining monitoring is the occurrence of biphasic reactions in 1−23% of cases.37 In pediatric populations, the reported incidence of biphasic reactions is lower (up to 11%) and most biphasic reactions seem to be either milder or of similar severity compared with the original presentation, but there are no reliable methods for predicting biphasic reactions.56 Factors that have been implicated in development of biphasic reactions include absence or delay of epinephrine administration during initial anaphylactic reaction, initial event severity (receiving >1 epinephrine dose), and slow initial reaction resolution. Failure to administer corticosteroids may predispose to a biphasic response, although this has not been categorically shown. To date, no study has reported prior anaphylaxis history or presence of asthma or specific allergen triggers as factors predisposing to biphasic reactions.57
Anaphylaxis treatment does not end with acute episode resolution in a healthcare facility. Patients should be discharged with epinephrine or an epinephrine prescription, preferably in the form of epinephrine auto-injectors. Patients should be given a personalized written anaphylaxis emergency plan that helps them recognize anaphylaxis symptoms, coached in using self-injectable epinephrine, and referred to a pediatric allergy specialist for potential trigger assessment.58 Educational materials including emergency plans are published and available in Portuguese to improve anaphylaxis knowledge and management among patients, parents, and caregivers.59
Long-term anaphylaxis management
Anaphylaxis education should begin prior to ED discharge and include a personalized written anaphylaxis emergency action plan. Patients at high risk for anaphylaxis may need to carry two epinephrine doses, for cases in which the first dose is not effectively administered, symptoms persist despite successful first injection, or patients live far from medical resource settings or experience biphasic anaphylaxis.60 Epinephrine auto-injectors are designed for self-administration or for administration by another person, but patients should seek prompt professional treatment immediately following epinephrine administration.61 It has been shown that many children and adolescents suffering from anaphylaxis, even associated with severe respiratory distress, wheezing, or loss of consciousness, do not use their epinephrine auto-injector, which reinforces the need for future information campaigns.32
The European Academy of Allergy and Clinical Immunology (EAACI) guidelines refer to six absolute indications for epinephrine auto-injector prescription:4,20
- Previous anaphylaxis with food, latex, or unavoidable triggers;
- Previous exercise-induced anaphylaxis;
- Previous idiopathic anaphylaxis;
- Co-existent unstable or moderate-to-severe, persistent asthma with food allergy;
- Venom allergy in adults with previous systemic reactions (unless receiving maintenance VIT) and children with more than systemic cutaneous reactions;
- Underlying mast cell disorders or elevated baseline serum tryptase concentrations together with any previous systemic allergic reactions to insect stings, even in VIT-treated patients.37
Anaphylaxis management plan
A personalized written anaphylaxis emergency plan should include avoidance advice, contact details, and an anaphylaxis emergency action plan with likely presenting symptoms and how to respond to each.37 A UK study showed that a management plan implemented in a Pediatric Allergy Clinic had a positive effect on parental knowledge of avoidance measures and emergency reaction treatment.62
Focused preventive measures after diagnostic workup may reduce risk of new episodes in susceptible individuals. Venom immunotherapy is recommended for patients who experienced a systemic reaction after an insect sting and shown evidence of specific IgE to venom allergens.63 In pediatric patients, protection efficacy has been shown to be as high as 98%.58 At present, the only measure for food-induced anaphylaxis is strict dietary avoidance, but therapies to prevent food-induced anaphylaxis are under investigation.61 In selected patients, desensitization or oral immunotherapy with food allergens as milk, egg, peanut, or tree nut confirm that incremental dosing leads to clinical desensitization and possibly to immune tolerance development.41 In latex allergy, precautions should be taken during medical and surgical treatments. The possibility of cross-reactivity with fruits or other foods should also be investigated.64 In exercise-induced anaphylaxis, strict avoidance of the relevant co-trigger (as food or NSAIDs) should be recommended three hours prior to planned exercise and one hour following exercise. In physically active young children, it may be necessary to totally eliminate the food from diet to achieve successful separation of food ingestion and exercise.65
Information about future anaphylaxis risk may lead to stress and anxiety and this should be addressed as part of educational training to minimize the impact on patients’ quality of life, as some patients may require psychological intervention.66
Conclusion
Anaphylaxis is the cornerstone of an acute allergic reaction requiring immediate treatment. Although still a rare clinical condition, it seems to be on the rise among both adults and children. Young children seem to be particularly affected and males have an increased risk during childhood. In pediatric reports, foods are the main triggers, followed by drugs and insect venoms. Diagnosis is based on a plethora of signs and symptoms that can be easily missed in young patients. Immediate treatment should comprise IM epinephrine, but a personalized action plan must be designed for each patient after acute phase resolution to enable prompt recognition and treatment of future episodes. All patients should be assessed to identify triggers and implement preventive avoidance measures.
REFERENCES
1. Ring J, Messmer K. Incidence and severity of anaphylactoid reactions to colloid volume substitutes. Lancet. 1977; 1:466-9. [ Links ]
2. Simons FER, Ardusso LRF, Bilò MB, El-Gamal YM, Ledford DK, Ring J, et al. World Allergy Organization Guidelines for the Assessment and Management of Anaphylaxis. World Allergy Organ J. 2011; 4:13-37. [ Links ]
3. Simons FER, Ardusso LR, Bilò MB, Cardona B, Ebisawa M, El-Gamal YM, et al. International consensus on (ICON) anaphylaxis. World Allergy Organ J. 2014; 7:9. [ Links ]
4. Muraro A, Roberts G, Worm M, Bilò MB, Brockow K, Rivas KB, et al. Anaphylaxis: guidelines from the European Academy of Allergy and Clinical Immunology. Allergy. 2014; 69:1026-45. [ Links ]
5. Sampson HA, Muñoz-Furlong A, Campbell RL, Adkinson NF Jr, Bock SA, Branum A, et al. Second symposium on the definition and management of anaphylaxis: summary report-Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. J Allergy Clin Immunol. 2006; 117:391-7.
6. Tejedor-AlonsoM A, Moro-Moro M, Múgica-García MV. Epidemiology of Anaphylaxis: Contributions From the Last 10 Years. Journal of investigational allergology & clinical immunology. 2015; 25:163-75. [ Links ]
7. Tejedor Alonso MA, Moro Moro M, Múgica García MV, Hernández JE, Ingelmo AR, Albelda CV, et al. Incidence of anaphylaxis in the city of Alcorcon (Spain): a population-based study. Clin Exp Allergy. 2012; 42:578-89. [ Links ]
8. Tejedor Alonso MA, Moro MM, Hernández JE, Múgica García MV, Vila Albelda C, Rosado Ingelmo A, et al. Incidence of anaphylaxis in hospitalized patients. Int Arch Allergy Immunol. 2011; 156:212-20. [ Links ]
9. Rudders SA, Banerji A, Vassallo MF, Clark S, Camargo CA. Trends in pediatric emergency department visits for food-induced anaphylaxis. J Allergy Clin Immunol. 2010; 126:385-8. [ Links ]
10. Alvarez-Perea A, Ameiro B, Morales C, Zambrano G, Rodríguez A, Guzmán M, et al. Anaphylaxis in the Pediatric Emergency Department: Analysis of 133 Cases After an Allergy Workup. J Allergy Clin Immunol Pract. 2017; 5:1256-63. [ Links ]
11. Gaspar Â, Santos N, Piedade S, Santa-Marta C, Pires G, Sampaio G, et al. One-year survey of paediatric anaphylaxis in an allergy department. Eur Ann Allergy Clin Immunol. 2015; 47:197-205. [ Links ]
12. Grabenhenrich LB, Dölle S, Moneret-Vautrin A, Köhli A, Lange A, Spindler T, et al. Anaphylaxis in children and adolescents: The European Anaphylaxis Registry. J Allergy Clin Immunol. 2016; 137:1128-37.e1. [ Links ]
13. Wright CD, Longjohn M, Lieberman PL, Lieberman JA. An analysis of anaphylaxis cases at a single pediatric emergency department during a 1-year period. Ann Allergy Asthma Immunol. 2017; 118:461-4. [ Links ]
14. Lieberman P, Nicklas RA, Oppenheimer J, Kemp SF, Lang DM, Bernstein DI, et al. The diagnosis and management of anaphylaxis practice parameter: 2010 Update. Journal of Allergy and Clinical Immunology. 2010; 126:477-80.e42. [ Links ]
15. Vetander M, Helander D, Flodström C, Ostblom E, Alfvén T, Ly DH, et al. Anaphylaxis and reactions to foods in children - a population-based case study of emergency department visits. Clinical & Experimental Allergy. 2012; 42:568-77. [ Links ]
16. Lieberman P, Camargo Jr CA, Bohlke K, Jick H, Miller RL, Sheikh A, et al. Epidemiology of Anaphylaxis: Findings of the American College of Allergy, Asthma and Immunology Epidemiology of Anaphylaxis Working Group.; 2006. [ Links ]
17. Capps JA, Sharma V, Arkwright PD. Prevalence, outcome and pre-hospital management of anaphylaxis by first aiders and paramedical ambulance staff in Manchester, UK. Resuscitation. 2010; 81:653-7. [ Links ]
18. Panesar SS, Javad S, de Silva D, Nwaru BI, Hickstein L, Muraro A, et al. The epidemiology of anaphylaxis in Europe: a systematic review. Allergy. 2013; 68:1353-61. [ Links ]
19. Turner PJ, Gowland MH, Sharma V, Ierodiakonou D, Harper N, Garcez T, et al. Increase in anaphylaxis-related hospitalizations but no increase in fatalities: an analysis of United Kingdom national anaphylaxis data, 1992-2012. J Allergy Clin Immunol. 2015; 135:956-63.e1. [ Links ]
20. Muraro A, Roberts G, Clark A, Eigenmann PA, Halken S, Lack G, et al. The management of anaphylaxis in childhood: position paper of the European academy of allergology and clinical immunology. Allergy. 2007; 62:857-71. [ Links ]
21. Sole D, Ivancevich JC, Borges MS, Coelho MA, Rosario NA, Ardusso LRF, et al. Anaphylaxis in Latin America: a report of the online Latin American survey on anaphylaxis (OLASA). Clinics. 2011; 66:943-7. [ Links ]
22. Amaral R, Morais-Almeida M, Gaspar Â, Sa-Sousa A, Martins H, Fonseca J. A anafilaxia em Portugal: Primeiros registos do Catálogo Português de Alergias e outras Reacções Adversas. Revista Portuguesa de Imunoalergologia. 2014; 22:23-32. [ Links ]
23. Lee S, Hess EP, Lohse C, Gilani W, Chamberlain AM, Campbell RL. Trends, characteristics, and incidence of anaphylaxis in 2001-2010: A population-based study. J Allergy Clin Immunol. 2017; 139:182-8.e2. [ Links ]
24. Gupta R, Sheikh A, Strachan DP, Anderson HR. Time trends in allergic disorders in the UK. Thorax. 2007; 62:91-6. [ Links ]
25. Jerschow E, Lin RY, Scaperotti MM, McGinn AP. Fatal anaphylaxis in the United States, 1999-2010: temporal patterns and demographic associations. J Allergy Clin Immunol. 2014; 134:1318-28.e7. [ Links ]
26. Liew WK, Williamson E, Tang MLK. Anaphylaxis fatalities and admissions in Australia. J Allergy Clin Immunol. 2009; 123:434-42. [ Links ]
27. Tejedor-Alonso MA, Moro-Moro M, Mosquera González M, Rodriguez-Alvarez M, Pérez Fernández E, Zamalloa PL, et al. Increased incidence of admissions for anaphylaxis in Spain 1998-2011. Allergy. 2015; 70:880-3. [ Links ]
28. Lin RY, Anderson AS, Shah SN, Nurruzzaman F. Increasing anaphylaxis hospitalizations in the first 2 decades of life: New York State, 1990-2006. Annals of Allergy, Asthma & Immunology. 2008; 101:387-93. [ Links ]
29. Poulos LM, Waters A-M, Correll PK, Loblay RH, Marks GB. Trends in hospitalizations for anaphylaxis, angioedema, and urticaria in Australia, 1993-1994 to 2004-2005. J Allergy Clin Immunol. 2007; 120:878-84. [ Links ]
30. Russell S, Monroe K, Losek JD. Anaphylaxis management in the pediatric emergency department: opportunities for improvement. Pediatr Emerg Care. 2010; 26:71-6. [ Links ]
31. Bernstein DI, Wanner M, Borish L, Liss GM, the Immunotherapy Committee of the American Academy of Allergy A and I. Twelve-year survey of fatal reactions to allergen injections and skin testing: 1990-2001. Journal of Allergy and Clinical Immunology. 2004; 113:1129-36. [ Links ]
32. Chipps BE. Update in Pediatric Anaphylaxis: A Systematic Review. Clin Pediatr (Phila). 2013; 52:451-61. [ Links ]
33. Smith G. Alabama Boy, 3, Dies of Severe Reaction During Baked Milk Challenge Test. allergicliving.com. Published August 2017. https://www.allergicliving.com/2017/08/02/alabama-boy-3-dies-of-severe-reaction-during-baked-milk-challenge-test/. [ Links ]
34. Simons FER. Anaphylaxis: Recent advances in assessment and treatment. J Allergy Clin Immunol. 2009; 124:625-36; quiz 637-8. [ Links ]
35. de Silva IL, Mehr SS, Tey D, Tang MLK. Paediatric anaphylaxis: a 5 year retrospective review. Allergy. 2008; 63:1071-6. [ Links ]
36. Alangari AA, Twarog FJ, Shih M-C, Schneider LC. Clinical Features and Anaphylaxis in Children With Cold Urticaria. Pediatrics. 2004; 113:e313-7. [ Links ]
37. Muraro A, Roberts G, Worm M, Bilò MB, Brockow K, Rivas MF, et al. Anaphylaxis: Guidelines from the European Academy of Allergy and Clinical Immunology. Allergy: European Journal of Allergy and Clinical Immunology. 2014; 69:1026-45. [ Links ]
38. Simons FER, Ardusso LR, Bilò MB, Cardona V, Ebisawa M, El-Gamal YM, et al. International consensus on (ICON) anaphylaxis. World Allergy Organ J. 2014; 7:9. [ Links ]
39. Castells MC, Horan RF, Sheffer AL. Exercise-induced Anaphylaxis. Curr Allergy Asthma Rep. 2003; 3:15-21. [ Links ]
40. Campbell RL, Hagan JB, Manivannan V, Decker WW, Kanthala AR, Bellolio MF, et al. Evaluation of national institute of allergy and infectious diseases/food allergy and anaphylaxis network criteria for the diagnosis of anaphylaxis in emergency department patients. J Allergy Clin Immunol. 2012; 129:748-52. [ Links ]
41. Thomson H, Seith R, Craig S. Downstream consequences of diagnostic error in pediatric anaphylaxis. BMC Pediatr. 2018; 18:40. [ Links ]
42. EAACI_White_Paper.pdf. Accessed May 2, 2019. http://www.eaaci.org/documents/EAACI_White_Paper.pdf. [ Links ]
43. Sala-Cunill A, Cardona V, Labrador-Horrillo M, Luengo O, Esteso O, Garriga T, et al. Usefulness and limitations of sequential serum tryptase for the diagnosis of anaphylaxis in 102 patients. Int Arch Allergy Immunol. 2013; 160:192-9. [ Links ]
44. Worm M, Edenharter G, Ruëff F, Scherer K, Pföhler C, Mahler V, et al. Symptom profile and risk factors of anaphylaxis in Central Europe. Allergy. 2012; 67:691-8. [ Links ]
45. Rudders SA, Banerji A, Clark S, Camargo CA. Age-related differences in the clinical presentation of food-induced anaphylaxis. J Pediatr. 2011; 158:326-8. [ Links ]
46. Topal E, Bakirtas A, Yilmaz O, Karagol IHE, Arga M, Demirsoy MS, et al. Anaphylaxis in infancy compared with older children. Allergy Asthma Proc. 2013; 34:233-8. [ Links ]
47. Simons FER, Frew AJ, Ansotegui IJ, Bochner BS, Golden DBK, Finkelman FD, et al. Risk assessment in anaphylaxis: current and future approaches. J Allergy Clin Immunol. 2007; 120:S2-24. [ Links ]
48. Simons FER. Anaphylaxis in infants: Can recognition and management be improved? Journal of Allergy and Clinical Immunology. 2007; 120:537-40. [ Links ]
49. Dosanjh A. Infant anaphylaxis: the importance of early recognition. J Asthma Allergy. 2013; 6:103-7. [ Links ]
50. Gallagher M, Worth A, Cunningham-Burley S, Sheikh A. Strategies for living with the risk of anaphylaxis in adolescence: qualitative study of young people and their parents. Prim Care Respir J. 2012; 21:392-7. [ Links ]
51. Marrs T, Lack G. Why do few food-allergic adolescents treat anaphylaxis with adrenaline?-Reviewing a pressing issue. Pediatr Allergy Immunol. 2013; 24:222-9. [ Links ]
52. Muñoz-Furlong A. Food allergy in schools: concerns for allergists, pediatricians, parents, and school staff. Ann Allergy Asthma Immunol. 2004; 93:S47-50. [ Links ]
53. Sheikh A, Shehata YA, Brown SGA, Simons FER. Adrenaline for the treatment of anaphylaxis: cochrane systematic review. Allergy. 2009; 64:204-12. [ Links ]
54. Burks AW, Jones SM, Boyce JA, Sicherer SH, Wood RA, Assa’ad A, et al. NIAID-sponsored 2010 guidelines for managing food allergy: applications in the pediatric population. Pediatrics. 2011; 128:955-65. [ Links ]
55. Liberman DB, Teach SJ. Management of anaphylaxis in children. Pediatr Emerg Care. 2008; 24:861-6; quiz 867-9. [ Links ]
56. Mehr S, Liew WK, Tey D, Tang MLK. Clinical predictors for biphasic reactions in children presenting with anaphylaxis. Clin Exp Allergy. 2009; 39:1390-6. [ Links ]
57. Tole JW, Lieberman P. Biphasic anaphylaxis: review of incidence, clinical predictors, and observation recommendations. Immunol Allergy Clin North Am. 2007; 27:309-26. [ Links ]
58. Simons FER. Anaphylaxis, killer allergy: long-term management in the community. J Allergy Clin Immunol. 2006; 117:367-77. [ Links ]
59. Carneiro-Leão L, Santos N, Gaspar Â. Anafilaxia na comunidade - Materiais educacionais. Revista Portuguesa de Imunoalergologia. 2018; 26:121-6. [ Links ]
60. Dinakar C. Anaphylaxis in Children: Current Understanding and Key Issues in Diagnosis and Treatment. Curr Allergy Asthma Rep. 2012; 12:641-9. [ Links ]
61. Järvinen KM, Celestin J. Anaphylaxis avoidance and management: educating patients and their caregivers. J Asthma Allergy. 2014; 7:95-104. [ Links ]
62. Kapoor S, Roberts G, Bynoe Y, Gaughan M, Habibi P, Lack G. Influence of a multidisciplinary paediatric allergy clinic on parental knowledge and rate of subsequent allergic reactions. Allergy. 2004; 59:185-91. [ Links ]
63. Moffitt JE, Golden DBK, Reisman RE, Lee R, Nicklas R, Freeman T, et al. Stinging insect hypersensitivity: a practice parameter update. J Allergy Clin Immunol. 2004; 114:869-86. [ Links ]
64. Gaspar Â, Faria E. Alergia ao látex. Revista Portuguesa de Imunoalergologia. 2012; 20:173-92. [ Links ]
65. Robson-Ansley P, Toit GD. Pathophysiology, diagnosis and management of exercise-induced anaphylaxis. Curr Opin Allergy Clin Immunol. 2010; 10:312-7. [ Links ]
66. Manassis K. Managing Anxiety Related to Anaphylaxis in Childhood: A Systematic Review. Journal of Allergy. 2012; 2012:1-7. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Maria Luís Marques
Department of Allergy and Clinical Immunology
Centro Hospitalar Universitário do Porto
Largo Prof. Abel Salazar
4099-001 Porto
Email: maluis234@gmail.com
Received for publication: 19.05.2019. Accepted in revised form: 23.01.2020