Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Nascer e Crescer
versão impressa ISSN 0872-0754versão On-line ISSN 2183-9417
Nascer e Crescer vol.29 no.3 Porto set. 2020
https://doi.org/10.25753/BirthGrowthMJ.v29.i3.18356
CASE REPORTS | CASOS CLÍNICOS
Idiopathic spinal accessory nerve injury
Lesão idiopática do nervo espinhal acessório
Pedro Cubelo PereiraI, Benedita Bianchi de AguiarII, Inês Machado VazIII, Duarte DantasI
I Department of Physical Medicine and Rehabilitation, Hospital Pedro Hispano, Unidade Local de Saúde de Matosinhos. 4464-513 Senhora da Hora, Portugal. pedrocubelopereira@gmail.com; djldantas@gmail.com
II Department of Pediatrics, Centro Hospital Entre Douro e Vouga. 4520-211 Santa Maria da Feira, Portugal. beneditabaguiar@gmail.com
III General Rehabilitation Unit, Centro de Reabilitação do Norte. 4405-565 Valadares, Portugal. inessgmv@gmail.com
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Palsy of the eleventh cranial nerve - or spinal accessory nerve (SAN) − is a rare cause of scapular winging, leading to painful upper extremity disability due to weakness and atrophy of the trapezius muscle. Most SAN injuries are iatrogenic, and no specific pediatric epidemiology is known.
Herein is described the case of a 17-year-old adolescent referred to Physical and Rehabilitation Medicine consultation due to insidious right shoulder pain with two years of evolution.
Shoulder pain combined with muscular atrophy is suggestive of nerve lesion. Electromyography is the gold standard exam and showed segmental demyelination and axonotmesis in this case. After evaluation, the patient underwent physiotherapy, with excellent results.
In conclusion, SAN injury treatment can be conservative or surgical and physiotherapy is the basis of early treatment in most cases. Recovery can occur even after a significant period of time.
Keywords: muscular atrophy; nerve injury; pain; physiotherapy; shoulder pain; spinal accessory nerve
RESUMO
Paralisia do décimo primeiro nervo craniano - ou nervo espinhal acessório (NEA) − é uma causa rara de escápula alada, levando a incapacidade dolorosa do membro superior devido a diminuição da força e atrofia do músculo trapézio. A maioria das lesões do NEA são iatrogénicas e não é conhecida epidemiologia específica na população pediátrica.
Este estudo descreve o caso de uma adolescente de 17 anos de idade referenciada para consulta de Medicina Física e de Reabilitação por omalgia direita insidiosa com dois anos de evolução.
Omalgia combinada com atrofia muscular sugere a ocorrência de lesão nervosa. A eletromiografia é o exame de eleição que, neste caso, revelou desmielinização segmentar e axonotmesis. Após avaliação, a jovem realizou fisioterapia, com excelentes resultados.
Em conclusão, o tratamento de lesões do NEA pode ser conservador ou cirúrgico, sendo a fisioterapia o principal tratamento precoce na maioria dos casos. A recuperação pode ocorrer mesmo após um período significativo de tempo.
Palavras-chave: atrofia muscular; dor; fisioterapia; lesão nervosa; nervo espinhal acessório; omalgia
Introduction
Palsy of the eleventh cranial nerve − or spinal accessory nerve (SAN) − is a rare cause of scapular winging, leading to painful upper extremity disability due to weakness and atrophy of the trapezius muscle. When SAN lesion is the cause of scapular winging, scapula rotates distally as well as laterally and slightly flares. This results in a medial superior scapula angle closer to the midline than the inferior scapula angle. This type of winging is sometimes referred to as lateral winging, as there is lateral scapula displacement without trapezius medial pull.1
Most SAN lesions are iatrogenic, mostly due to lymph node biopsy (2−10% of procedure cases) and radical neck dissection, although alternative traumatic mechanisms (such as carotid endarterectomy and internal jugular vein catheterization) have been described. No specific pediatric epidemiology is acknowledged.2-7 Traction can injure the nerve, resulting in segmental demyelination and nerve function loss.
Injured nerve may be the main branch or a small branch innervating the upper trapezius muscle. Most presenting signs and symptoms are attributed to denervation of the upper trapezius muscle.1,2
Herein, the authors describe a rare case of typical SAN lesion with no identifiable factor in an adolescent.
Clinical case
A 17-year-old adolescent was referred to Orthopedic consultation due to insidious right shoulder pain with two years of evolution. No previous history of surgery or trauma was reported. During clinical assessment, the girl presented with sloping shoulder and lateral deviation of the inferior scapula angle. Shoulder and elbow motion range was normal, although scapular dyskinesis was evident during lateral shoulder elevation, with early right scapula rotation. Neurological exam showed no further abnormalities. Rotator cuff and shoulder impingement tests were negative.
Due to suspicion of SAN lesion, the patient underwent computed tomography (CT) scan, with normal findings, and electromyography (EMG), with results compatible with moderate axonotmesis of the right SAN nerve.
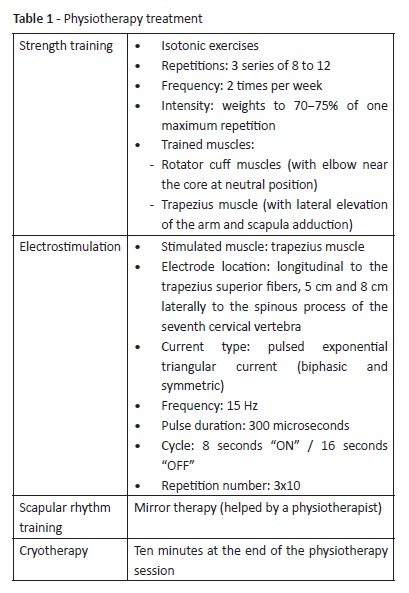
The patient was submitted to a comprehensive rehabilitation program directed at pain control and strength and function recovery. Physical therapy main goal was rotator cuff muscle and trapezius strengthening, to diminish asymmetry and arrhythmic scapular movements. Physiotherapy sessions were designed based on strength training, electrostimulation, scapular rhythm training, and cryotherapy (Table I).
Results were satisfactory, with diminished pain and minimal muscle trophy asymmetry. Functionally, the patient was always totally independent and currently maintains strengthening training, with improved self-esteem.
Comments
Traditional SAN descriptions distinguish between a spinal and a cranial part. SAN is considered the eleventh of twelve cranial nerve pairs, as part of it was formerly believed to originate in the brain. SAN supplies sternocleidomastoid and trapezius muscles and is a purely motor nerve. Integrity of the spinal accessory nerve is crucial for thoracoscapular function and scapulohumeral rhythm.1 Sternocleidomastoid primary actions include head rotation to the opposite side and neck flexion. Trapezius is the major shoulder girdle suspensory muscle. Upper fibers elevate the scapula and rotate the lateral angle upward. The intermediate portion adducts and retracts the scapula, and the inferior region depresses and rotates the scapula downward. SAN lesions usually present with pain; evident trapezius upper third atrophy; sag shoulder and scapular winging; shoulder lateral elevation limited to less than 90 degrees with early scapular rotation; shoulder girdle and arm weakness; weak anterior shoulder elevation; and sensory disturbance of the third and fourth cervical nerve areas (pulling sensation or aching).2 For this reason, shoulder pain combined with muscular atrophy potentially indicates nerve lesion, and sagged shoulder due to trapezius muscle atrophy along with scapular winging potentially suggests SAN lesion.
Owing to its anatomy, SAN is vulnerable to injury along its superficial course. Iatrogenic nerve damage of the posterior neck triangle is most frequent, although alternative traumatic mechanisms have been described. In this particular case, as the patient had no prior history of neck surgery or trauma, lesion was of probable idiopathic origin.3 Differential diagnosis includes long thoracic nerve lesions (paralysis of serratus anterior), brachial plexus neuropathy, and myofascial pain syndromes of the shoulder girdle region.
EMG is the gold standard exam, usually showing segmental demyelination and axonotmesis. High-resolution ultrasonography enables visualization of the normal spinal accessory nerve.8 CT and nerve magnetic resonance imaging scan can be performed to exclude other pathologies.9 In this case, EMG result compatible with moderate axonotmesis of the right SAN nerve together with clinical presentation were key for diagnosis.
Like most nerve injuries, recovery can occur even after a significant period of time, usually more than six months. Treatment can be conservative or surgical.1 Early nonoperative treatment is paramount, except in particular cases, and consists of pain control and motion range and strengthening exercises, to stimulate trapezius muscle or compensate its lack of strength. Electric neurostimulation can be performed.10
Surgical treatment is indicated in one of the following situations: iatrogenic intraoperative nerve transection, delayed diagnosis with substantial shoulder symptoms, SAN palsy with no improvement with conservative management, and severe paralysis.11 Surgical treatment consists of neurolysis, nerve repair with or without graft, or Eden-Lange muscle transfer.
As in the present case, treatment should be mostly conservative. The patient showed positive evolution, with little muscle atrophy asymmetry and no associated pain.
REFERENCES
1. Camp SJ, Birch R. Injuries to the spinal accessory nerve. J Bone Joint Surg. 2011; 93-B: 62-7. [ Links ]
2. Chandawarkar RY, Cervino AL, Pennington GA. Management of iatrogenic injury to the spinal accessory nerve. Plast Reconstr Surg. 2003; 111:611-7. [ Links ]
3. London J, London N, Kay S. latrogenic accessory nerve injury. Ann R Coll Surg Engl. 1996; 78:146-50. [ Links ]
4. Valtonen EJ, Lilius HG. Late sequelae of iatrogenic spinal accessory nerve injury. Acta Chir Scand. 1974; 140:453-5. [ Links ]
5. Prim MP, De Diego JI, Verdaguer JM, Sastre N, Rabanal I. Neurological complications following functional neck dissection. Eur Arch Otorhinolaryngol. 2006; 263:473-6. [ Links ]
6. Grossman JAI, Ruchelsman DE, Schwarzkopf R. Iatrogenic spinal accessory nerve injury in children. J Pediatric Surg. 2008. 43:1732-5. [ Links ]
7. Nakamichi KI, Tachibana S. Iatrogenic injury of the spinal accessory nerve. J Bone Joint Surg Am .1998; 80:1616-21. [ Links ]
8. Shen J, Chen W, Ye X, Qiu Y, Xu J, Zhu Y, et al. Ultrasound in the management of iatrogenic spinal accessory nerve palsy at the posterior cervical triangle area. Muscle Nerve. 2018; 59:64-9. [ Links ]
9. Nguyen C, Guérini H, Roren A, Zauderer J, Vuillemin V, Seror P, et al. Neuromuscular dynamic scapular winging: Clinical, electromyographic and magnetic resonance imaging diagnosis. Presse Med. 2015; 44:1256-65. [ Links ]
10. Akgun K, Aktas I, Uluc K. Conservative treatment for late-diagnosed spinal accessory nerve injury. Am J Phys Med Rehabil. 2008; 87:1015-21. [ Links ]
11. Göransson H, Leppänen OV, Vastamäki M. Patient outcome after surgical management of the spinal accessory nerve injury: A long-term follow-up study. SAGE Open Med. 2016; 4:2050312116645731. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Pedro Cubelo Pereira
Department of Physical Medicine and Rehabilitation
Hospital Pedro Hispano
Unidade Local de Saúde de Matosinhos
Rua Dr. Eduardo Torres
4464-513 Senhora da Hora
Email: pedrocubelopereira@gmail.com
Received for publication: 22.07.2019. Accepted in revised form: 03.02.2020